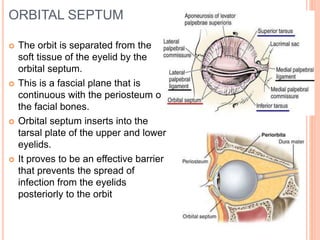
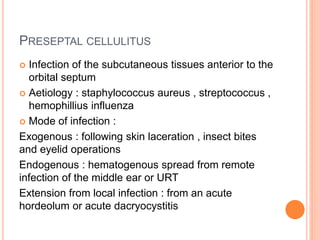
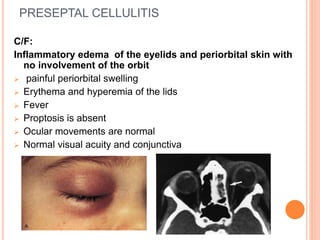
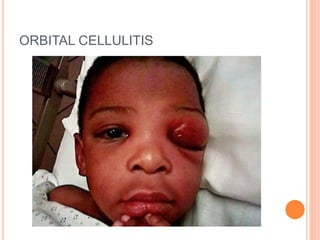
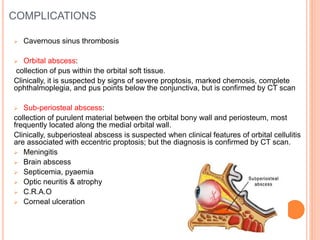
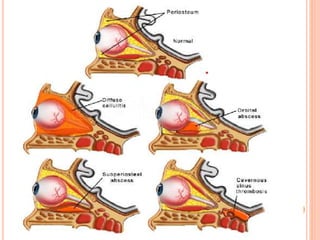
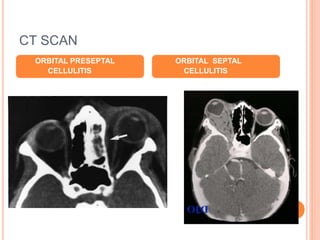
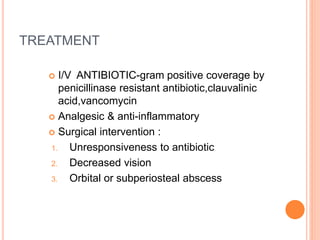
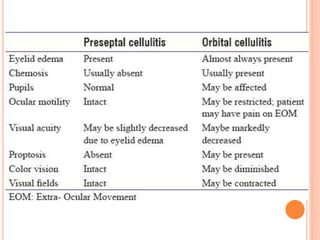
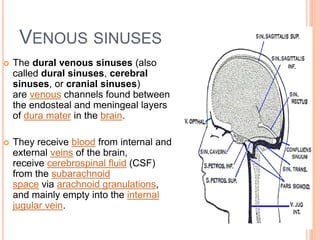
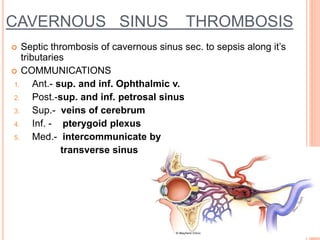
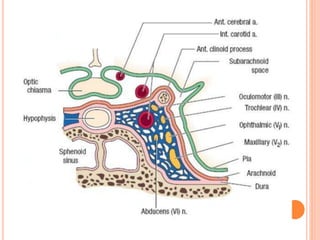
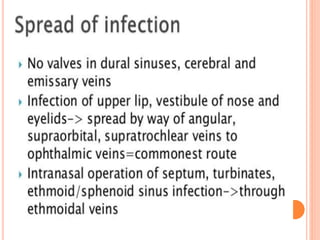
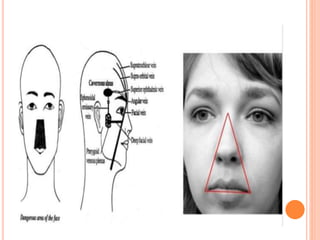
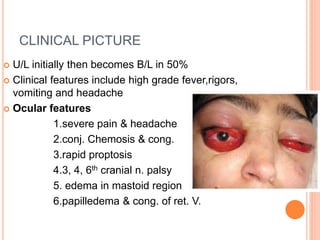
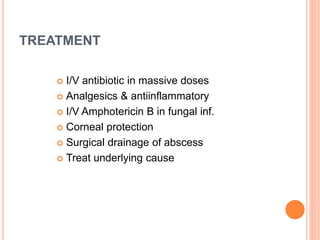
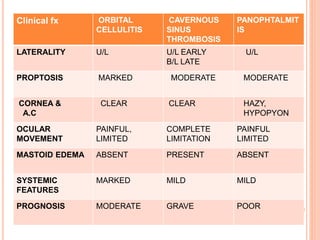
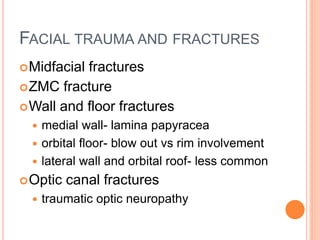
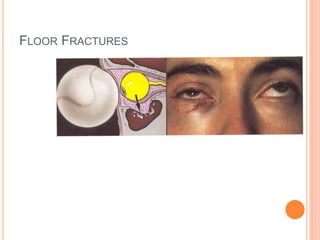
The orbit is separated from the eyelid by the orbital septum, which prevents spread of infection from the eyelids to the orbit. Preseptal cellulitis involves infection of tissues anterior to the septum, causing eyelid swelling and pain but no orbital involvement. Orbital cellulitis is infection behind the septum in the orbit, which can lead to complications like abscesses, cavernous sinus thrombosis, or meningitis if not treated promptly with IV antibiotics. Cavernous sinus thrombosis involves septic thrombosis of the cavernous sinus veins and can cause bilateral proptosis, cranial nerve palsies, and systemic symptoms. Facial trauma can cause fractures of the orbital walls which may require surgical