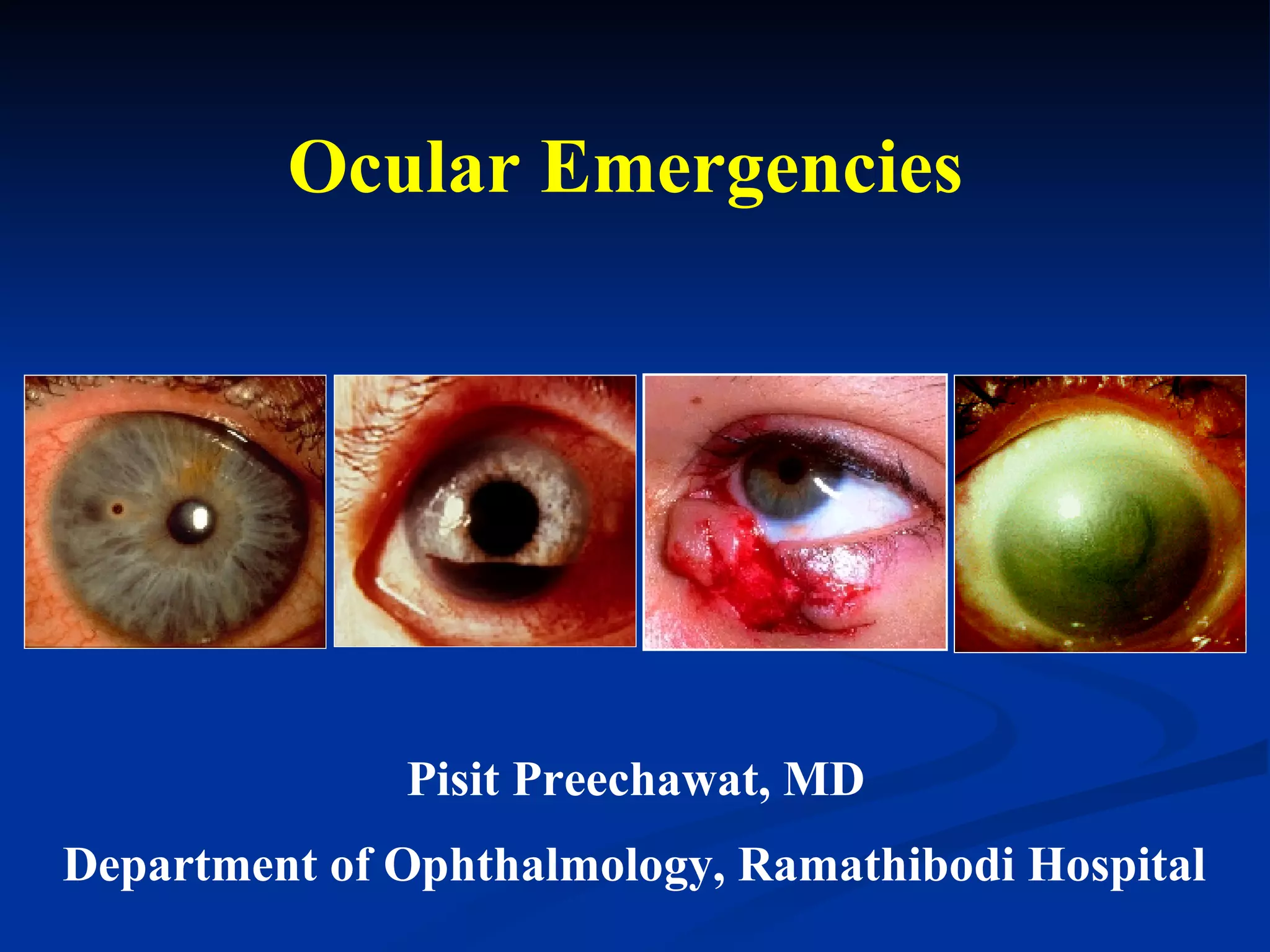
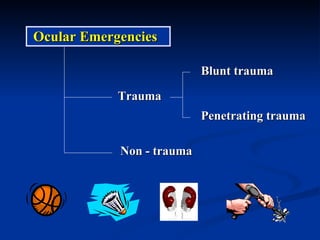
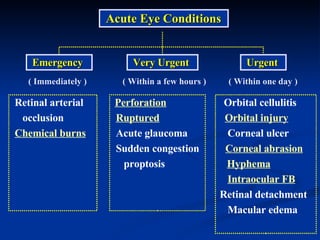
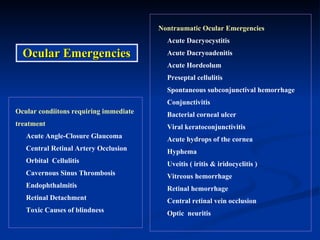
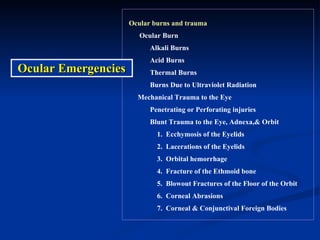
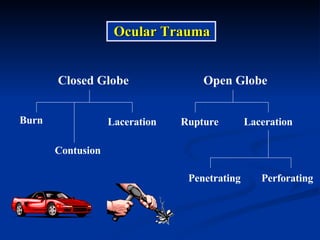
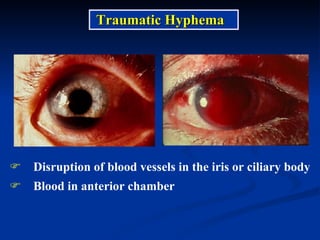
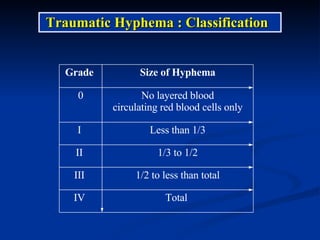
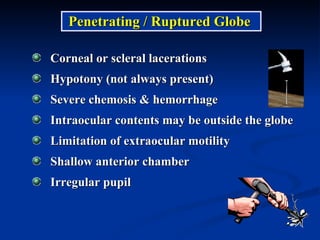
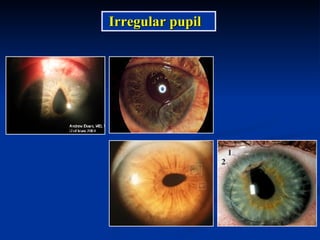
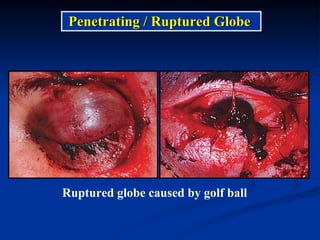
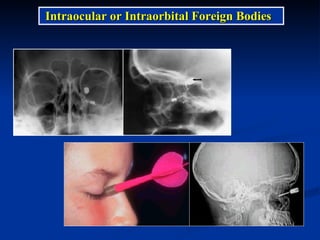
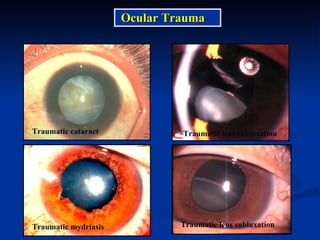
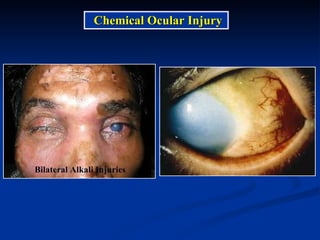
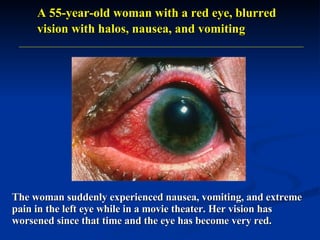
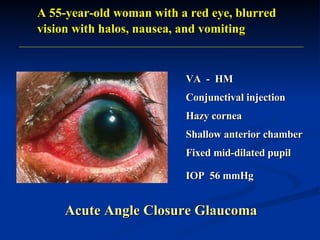
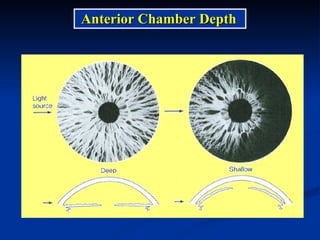
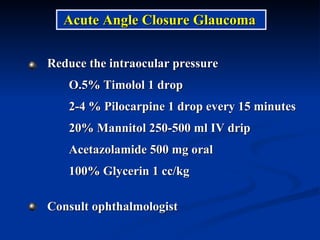
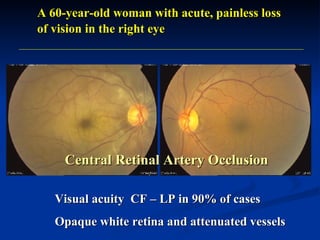
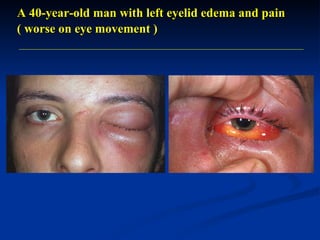
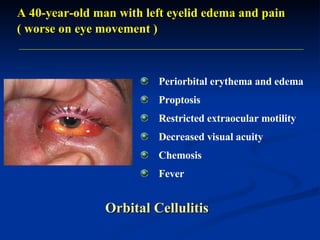
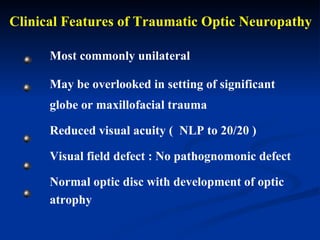
1. The document discusses various ocular emergencies including traumatic injuries like hyphema, ruptured globe, and chemical burns as well as non-traumatic emergencies like acute angle closure glaucoma and orbital cellulitis.
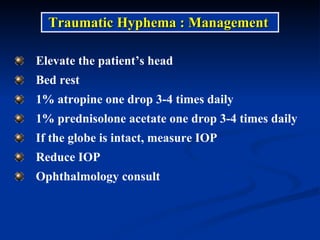
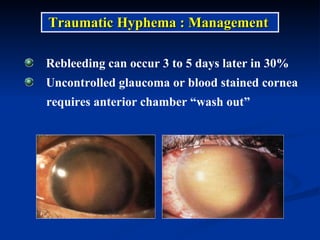
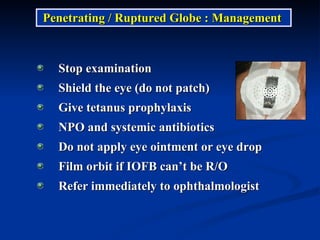
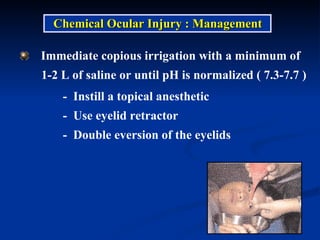
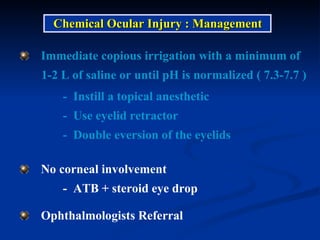
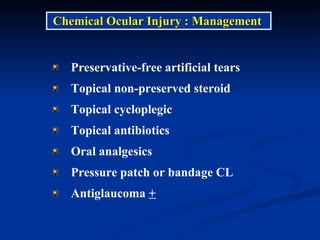
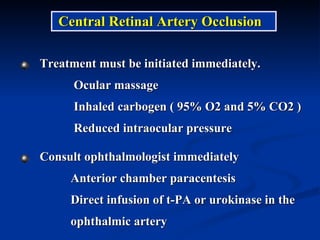
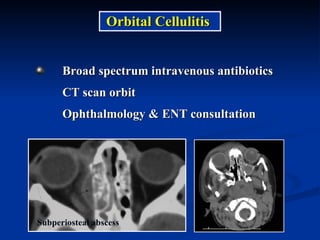
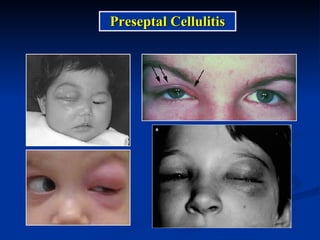
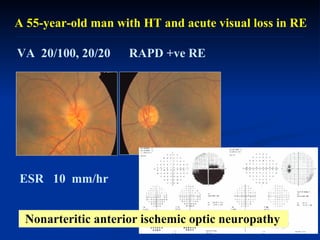
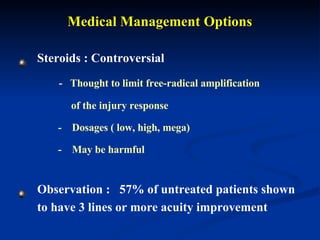
2. Management strategies are provided for different conditions including irrigation for chemical burns, medications to lower IOP for glaucoma, and IV antibiotics for orbital cellulitis.
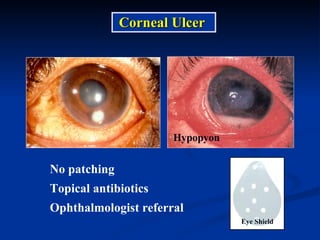
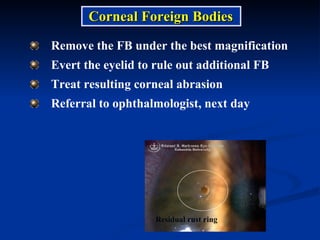
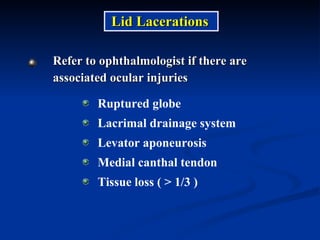
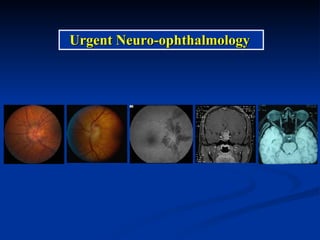
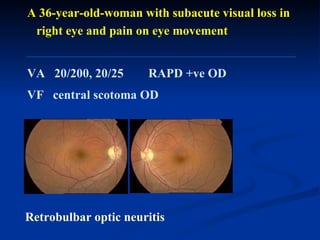
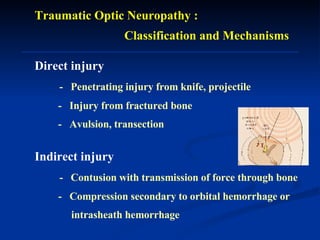
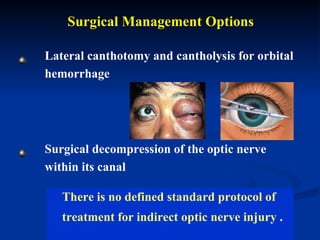
3. Immediate referral to an ophthalmologist is recommended for penetrating injuries, ruptured globe, retinal artery occlusion, and conditions requiring surgery.