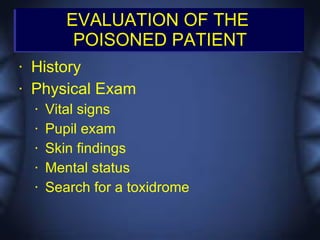
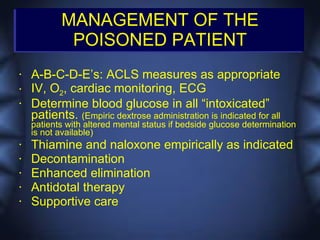
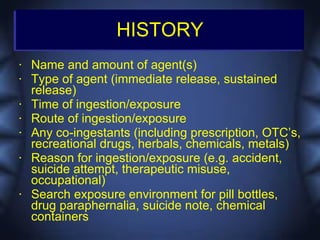
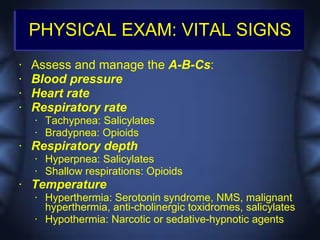
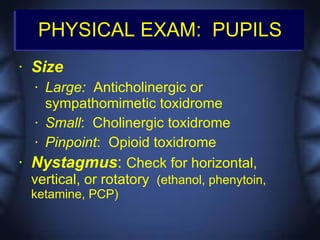
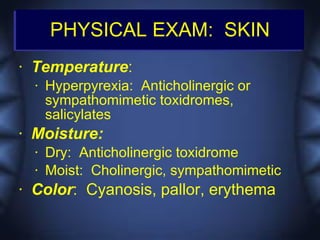
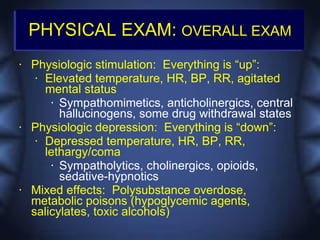
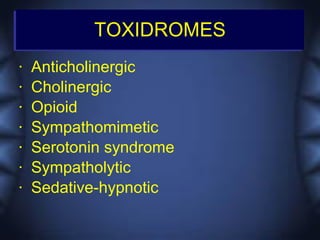
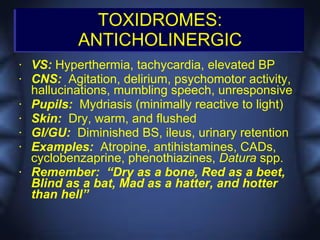
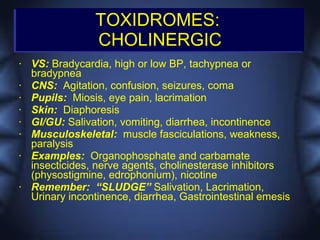
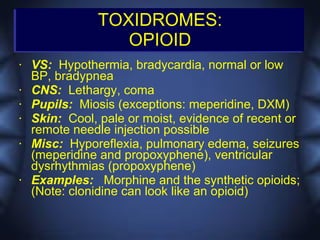
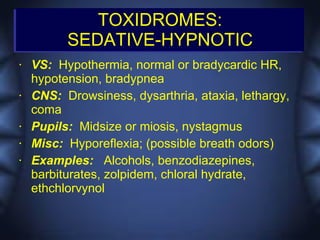
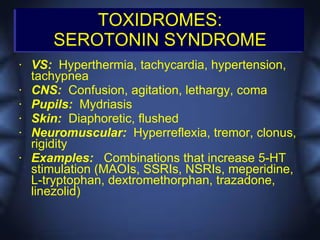
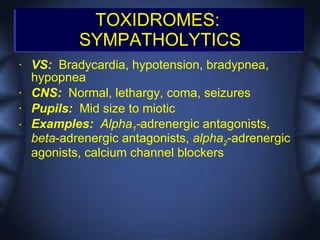
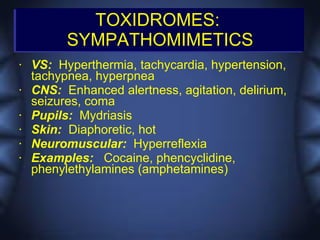
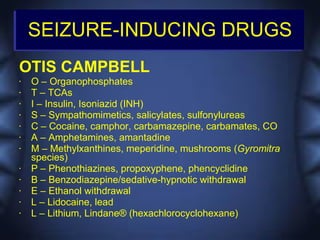
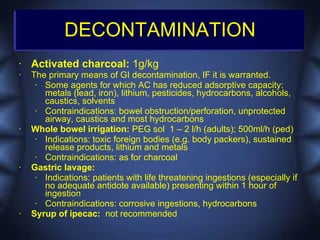
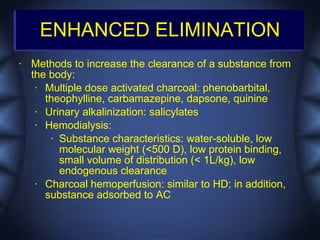
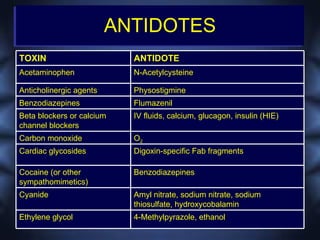
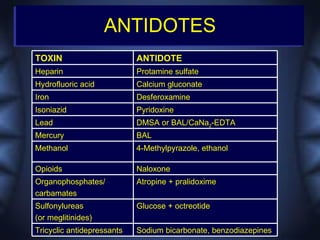
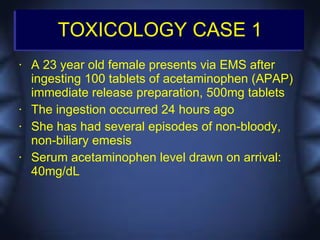
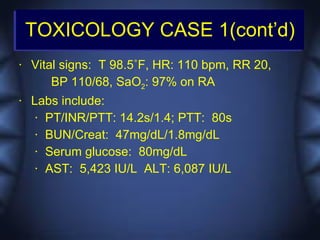
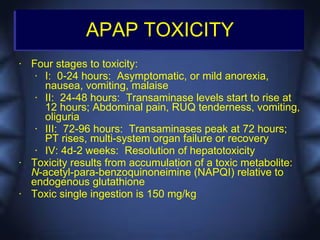
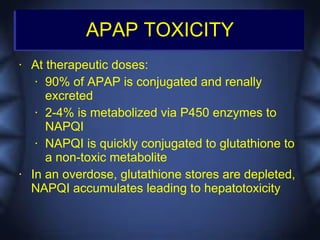
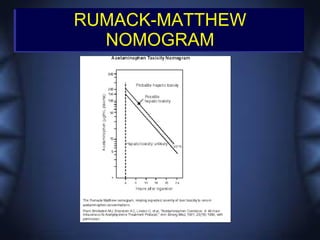
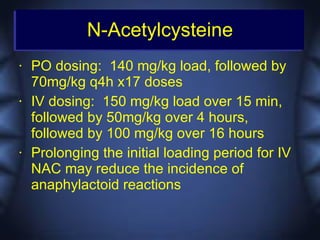
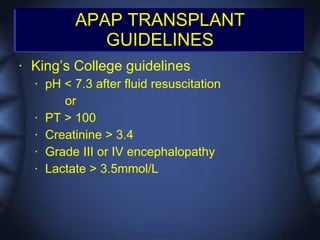
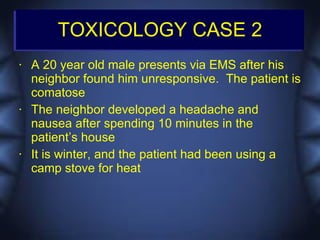
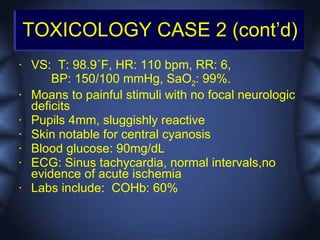
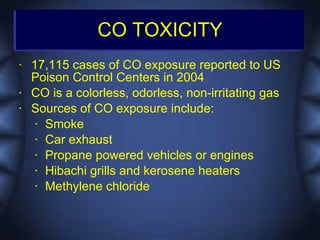
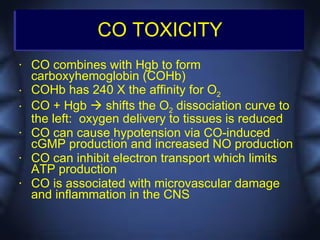
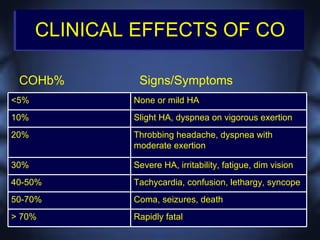
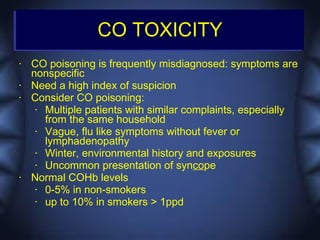
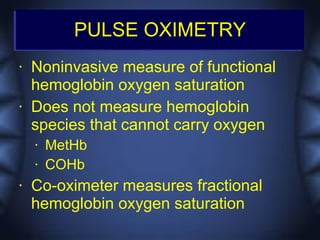
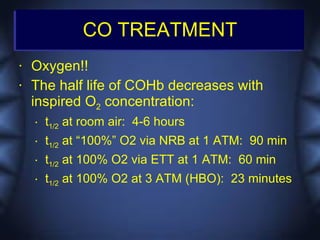
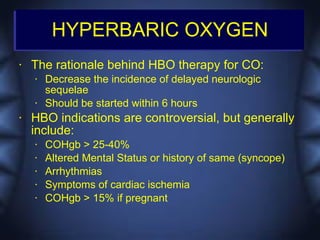
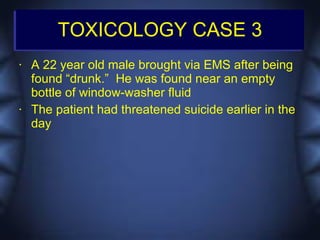
This document discusses toxicologic emergencies. It provides statistics on poisonings in the US and outlines the evaluation and management of poisoned patients. Key aspects of the history and physical exam are reviewed. Common toxidromes such as anticholinergic, opioid, and serotonin syndrome are described. Methods of decontamination, enhanced elimination, and use of antidotes are also outlined. Two case examples involving acetaminophen toxicity and carbon monoxide poisoning are then presented and discussed.