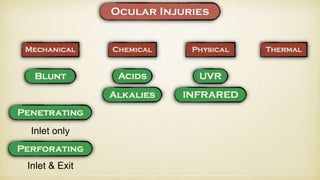
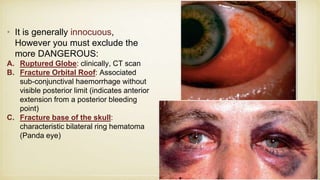
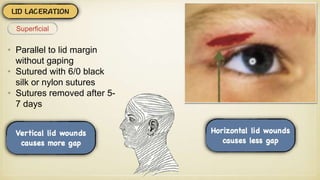
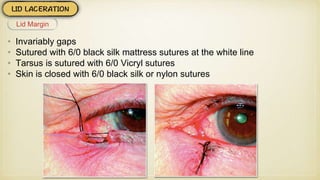
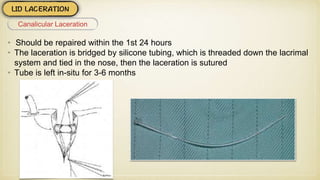
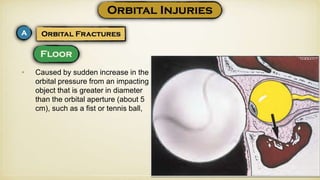
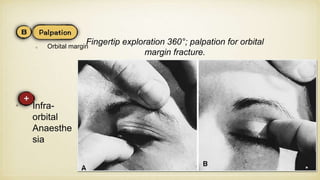
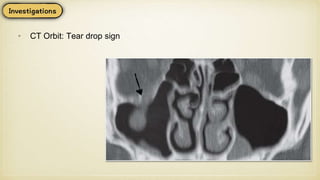
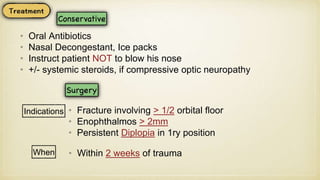
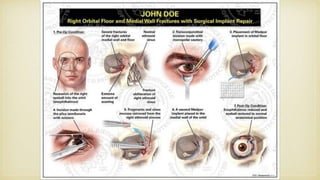
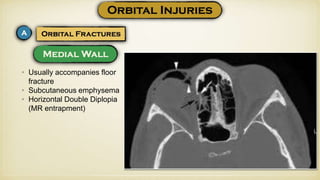
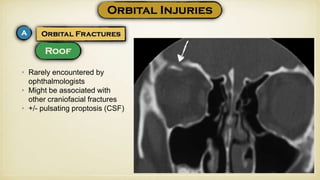
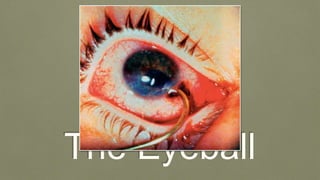
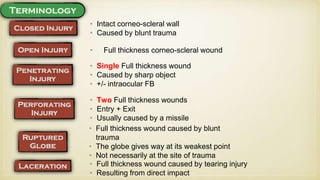
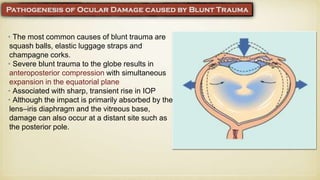
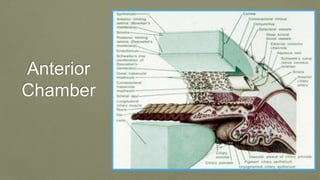
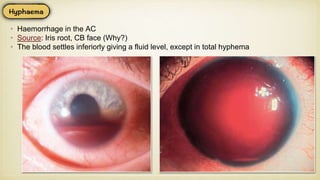
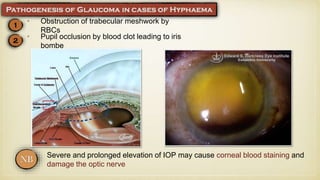
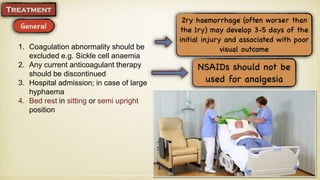
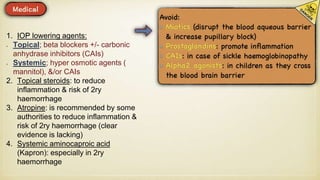
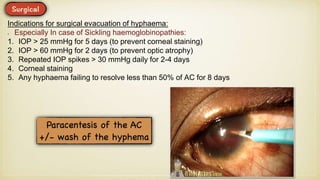
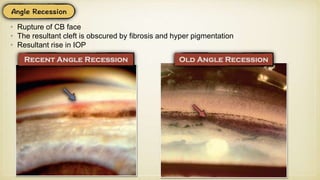
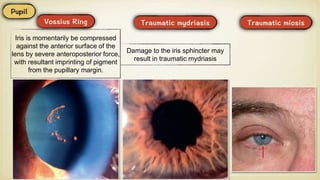
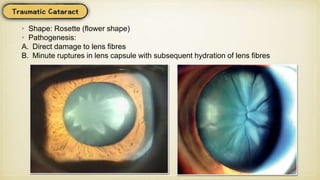
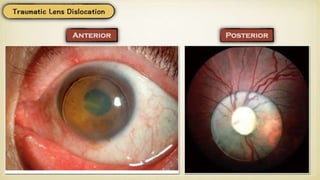
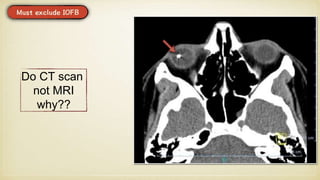
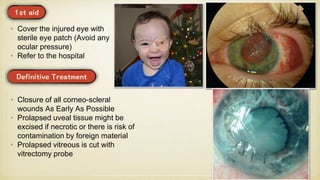
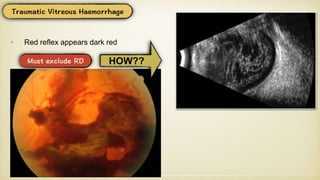
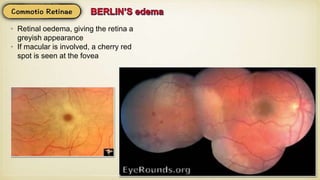
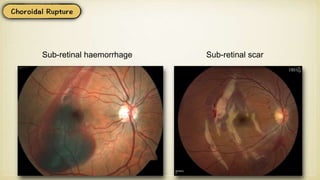
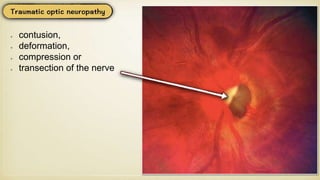
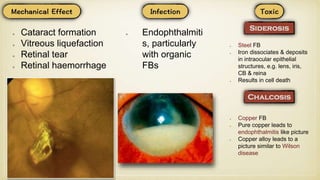
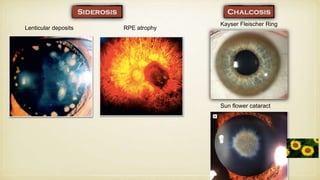
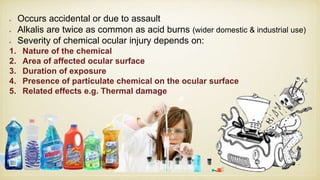
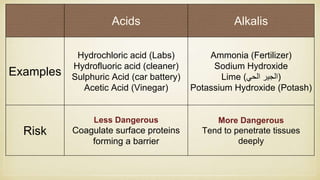
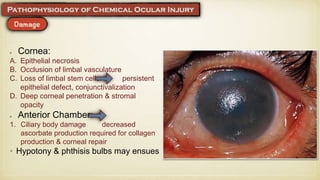
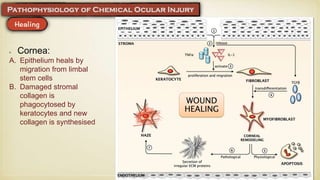
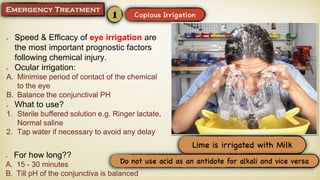
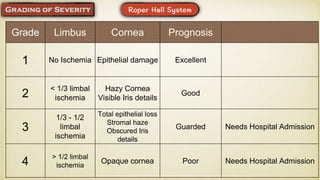
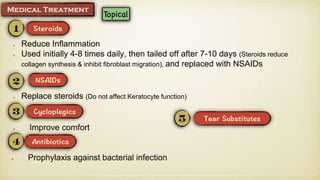
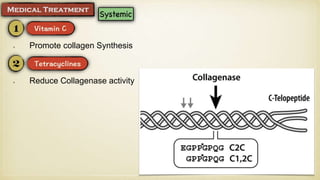
The document discusses various types of ocular trauma including injuries to the eyelid, orbit, eyeball, and adnexal structures. It describes the clinical presentation, investigations, and management of conditions like blunt trauma, penetrating injuries, chemical burns, ruptured globe, hyphema, and intraocular foreign bodies. Key points covered include the importance of thorough examination to exclude serious injuries, indications for imaging like CT scan, and principles of early irrigation in chemical injuries. Surgical repair or observation may be needed depending on the severity and location of injury. The prognosis depends on the extent of damage to structures like the cornea, limbus, and optic nerve.