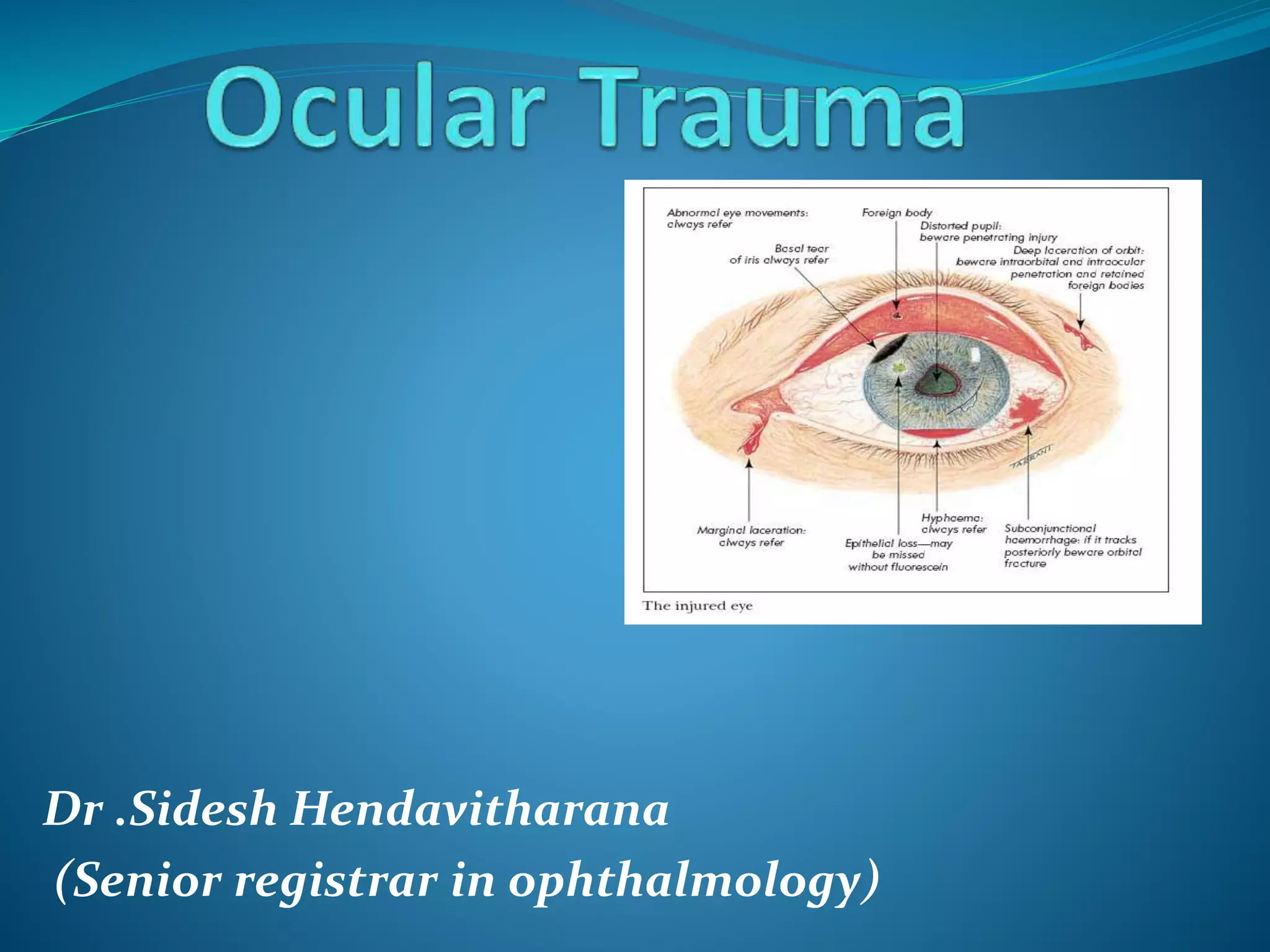
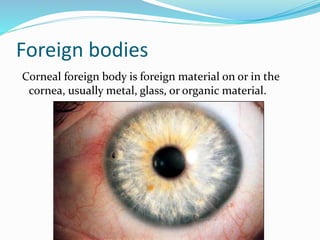
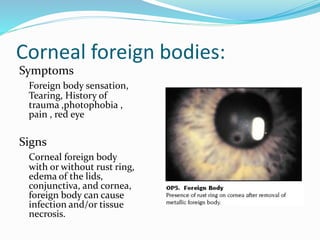
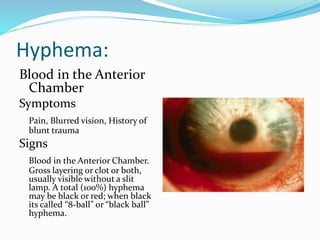
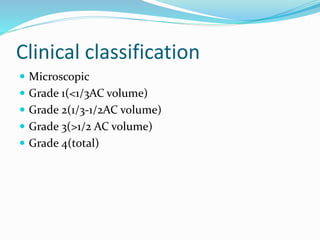
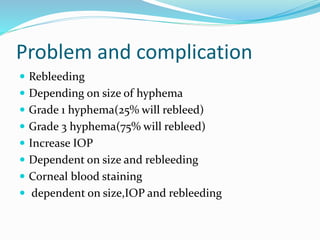
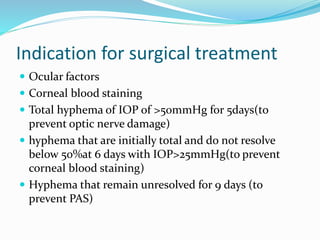
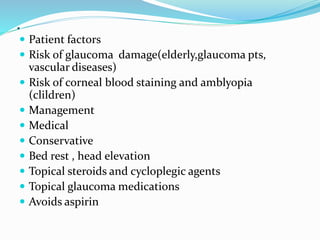
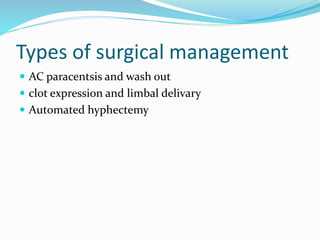
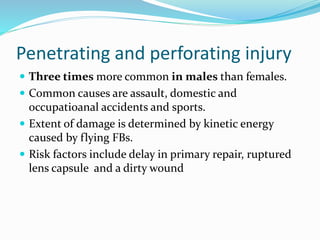
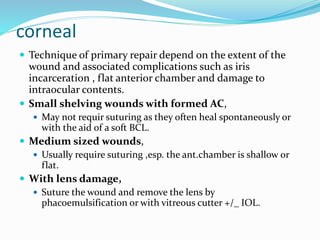
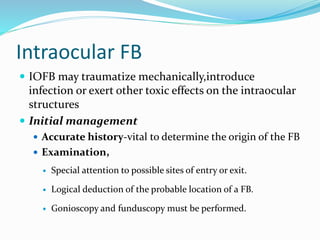
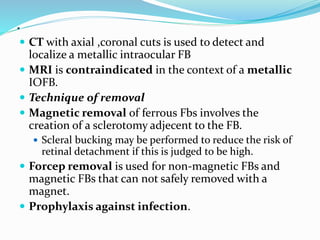
Ocular trauma is a medical emergency that requires prompt treatment. There are various types of ocular injuries including direct injuries from objects penetrating or bluntly impacting the eye, as well as indirect injuries from chemicals, heat, electricity or radiation. Corneal foreign bodies can cause pain, tearing and infection if not removed. Blunt trauma can damage tissues through direct impact, compression waves, and rebound forces. Common signs of blunt trauma include eyelid bruising, corneal abrasions, hyphema (blood in the anterior chamber), retinal tears and detachments, and increased intraocular pressure. Proper evaluation and management depends on the type and severity of injury.