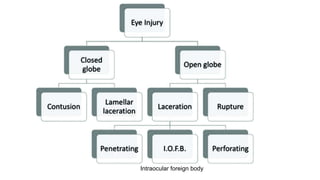
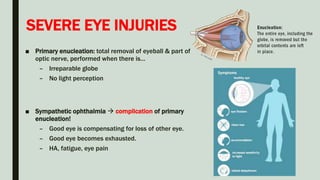
This document provides information on eye trauma, including causes, assessments, interventions, and nursing care. Key points include:
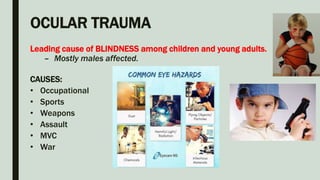
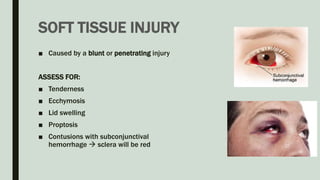
- Eye injuries are often preventable through safety measures. Common causes include accidents, assaults, and work or sports injuries.
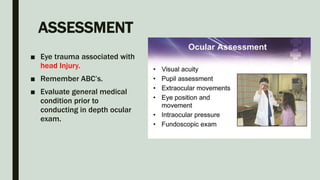
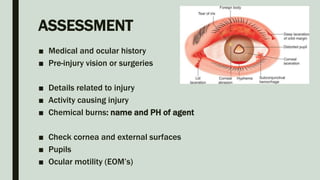
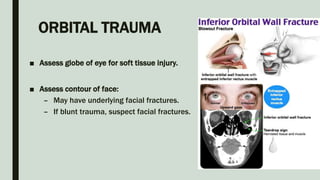
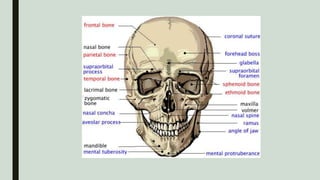
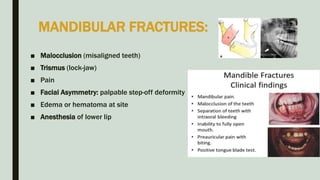
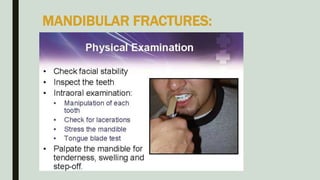
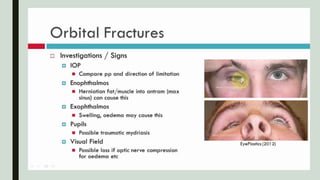
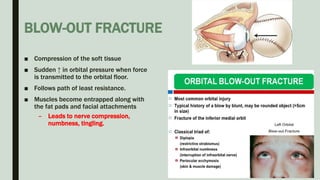
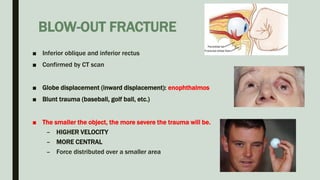
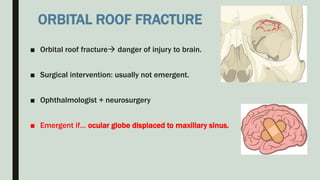
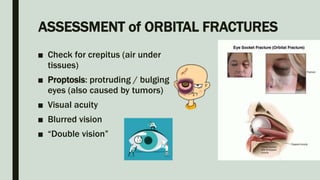
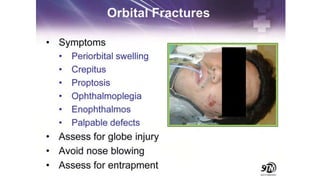
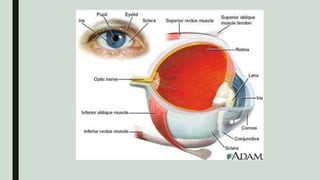
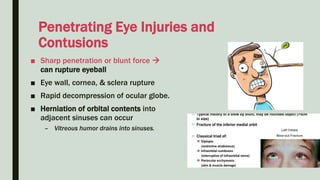
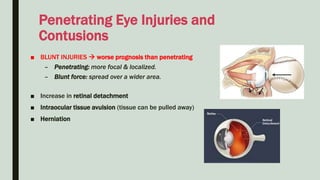
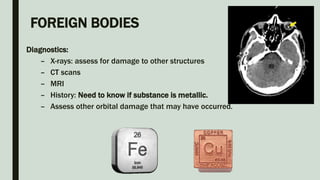
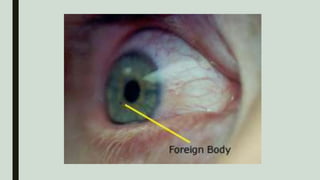
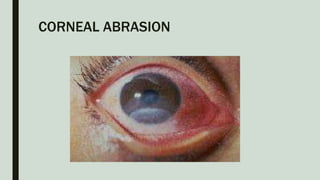
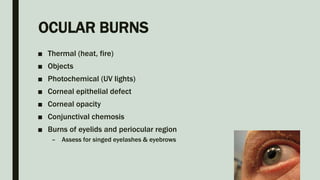
- Assessment of eye trauma involves evaluating visual acuity, eye movements, pupil response, and checking for foreign bodies or orbital fractures. History should include injury details.
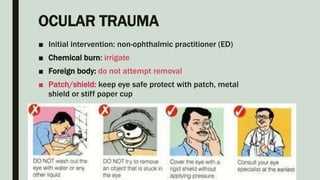
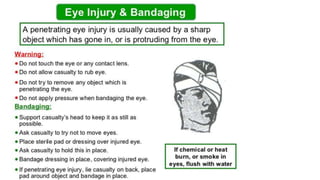
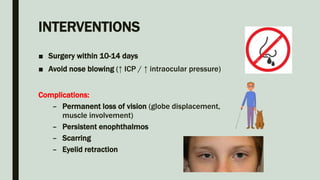
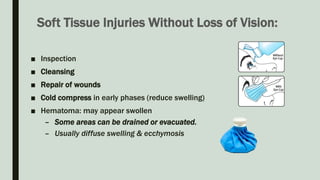
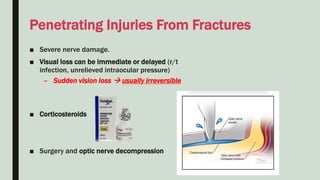
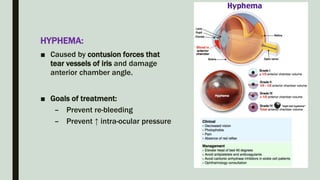
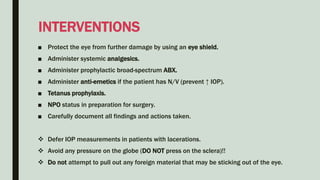
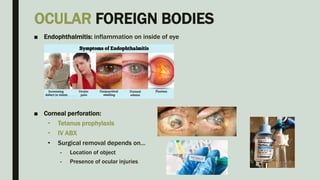
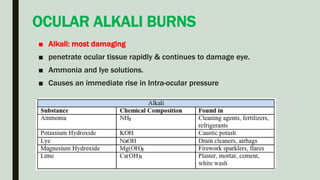
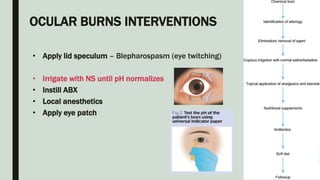
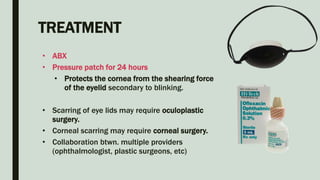
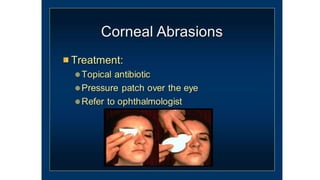
- Interventions depend on injury type but may include wound irrigation, patching, antibiotics, surgery for foreign bodies or fractures, and corticosteroids to reduce inflammation. Goals are to prevent infection and further damage.
- Nursing care focuses on monitoring for complications, educating on activity restrictions, and