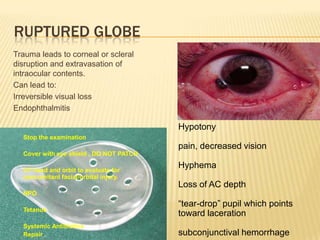
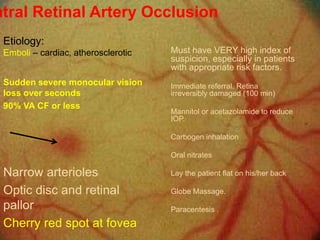
This document provides information on common ocular emergencies for non-ophthalmologists. It discusses how to examine the eye, useful tools, algorithms for diagnosis, key questions to ask patients presenting with red eye, classifications of ocular emergencies from immediate to urgent, and management of specific emergencies like chemical burns, ruptured globe, retinal artery occlusion, angle closure glaucoma, retrobulbar hematoma, orbital fractures, periorbital cellulitis, corneal foreign bodies, corneal injuries, hypopyon, and lid lacerations. The overall aim is to educate non-ophthalmologists on triaging and providing first aid for ocular emergencies until the patient can be referred