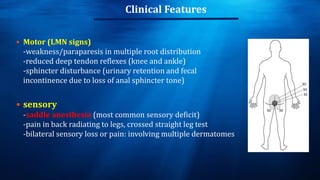
The document provides an overview of various orthopaedic emergencies including open fractures, acute compartment syndrome, dislocations, neurovascular injuries, septic joints, and cauda equina syndrome. Open fractures are classified using the Gustilo-Anderson system and require irrigation, debridement, and antibiotics. Acute compartment syndrome causes increased pressure within muscle compartments and requires urgent fasciotomy. Common dislocations include shoulder, knee, and hip joints. Neurovascular injuries from fractures require prompt assessment. Septic joints usually involve the knee and present with joint pain, swelling, and fever. Cauda equina syndrome is a surgical emergency from compression of lumbosacral nerve roots.