This document provides information on fistula-in-ano, including:
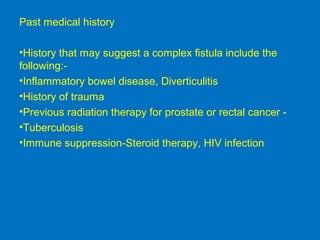
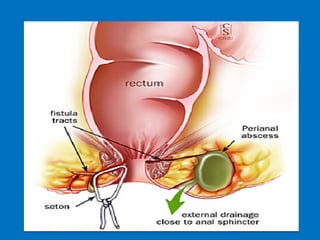
- It defines a fistula-in-ano as a track connecting the anal canal or rectum to the skin around the anus.
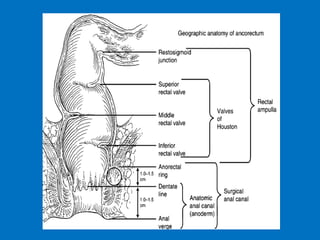
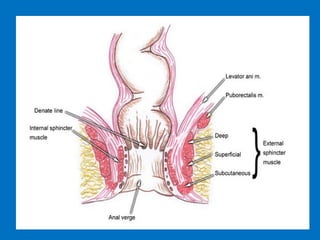
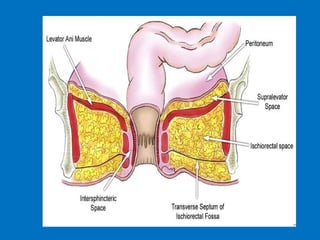
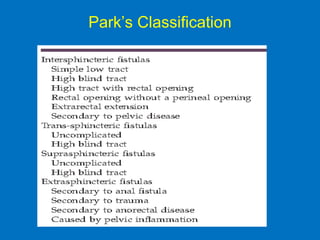
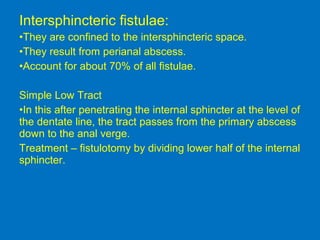
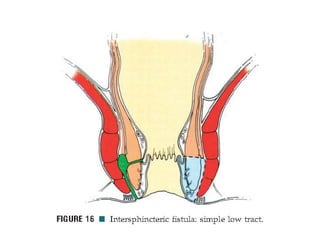
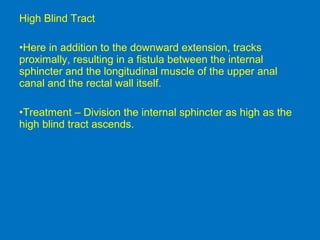
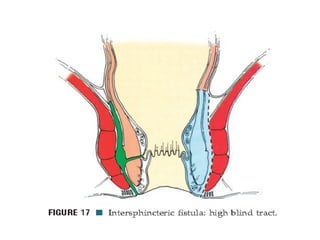
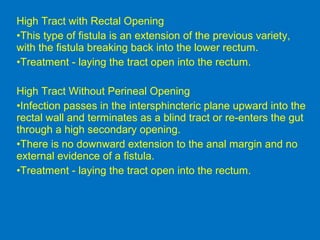
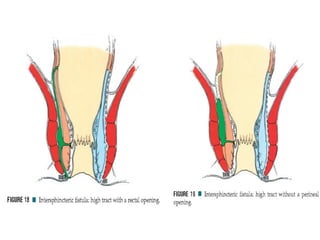
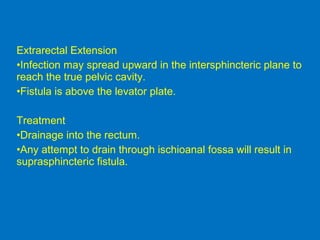
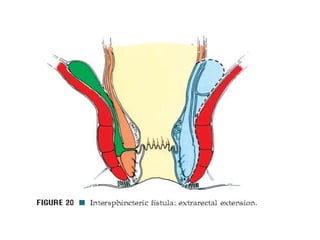
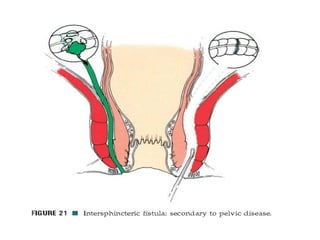
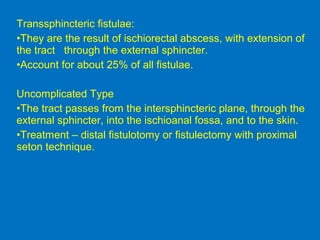
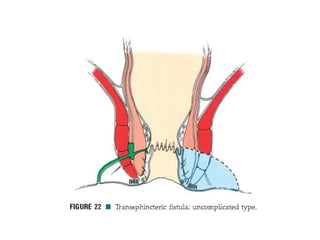
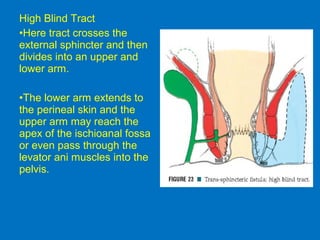
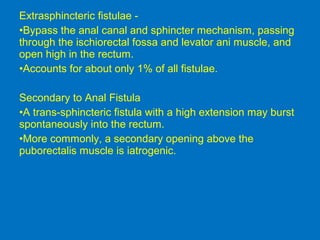
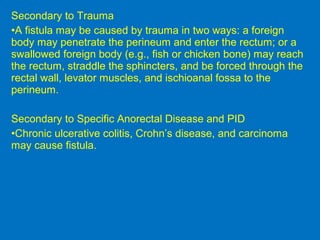
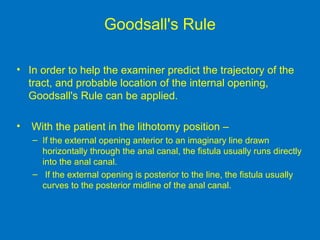
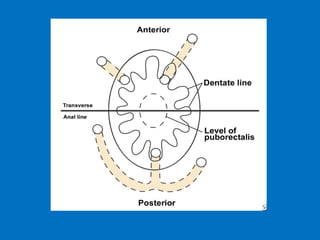
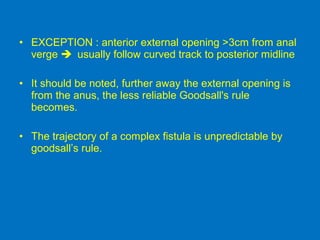
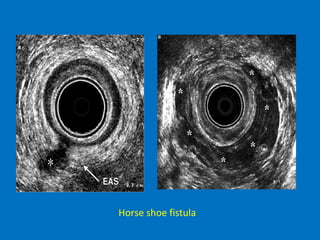
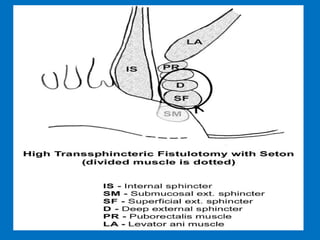
- It describes the anatomy of the anal canal and classifications of fistula types.
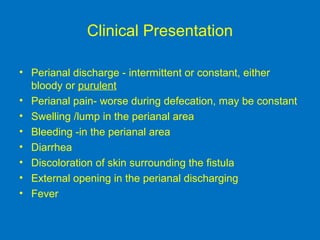
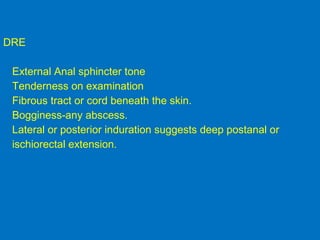
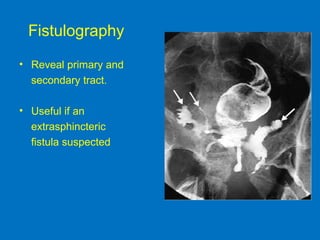
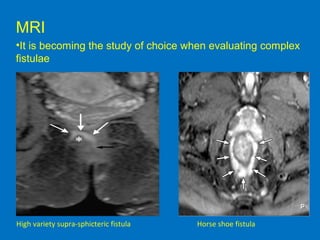
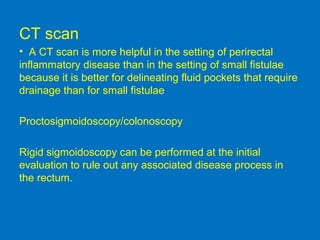
- Diagnosis involves physical exam, sometimes supplemented by imaging studies like MRI to better characterize complex fistulae.
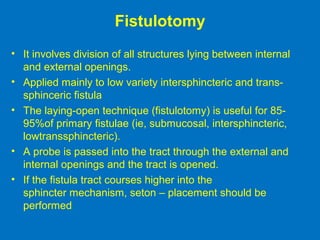
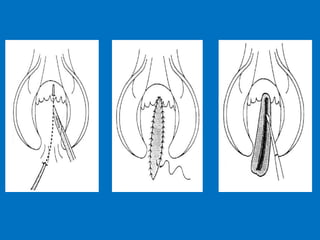
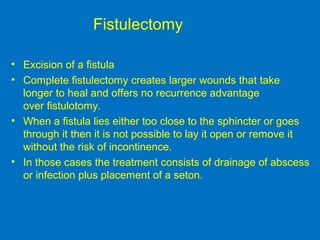
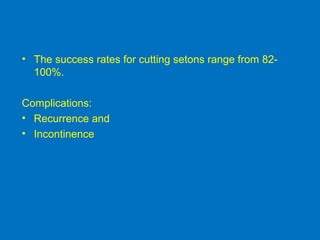
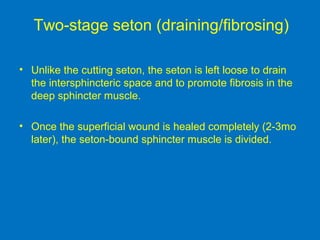
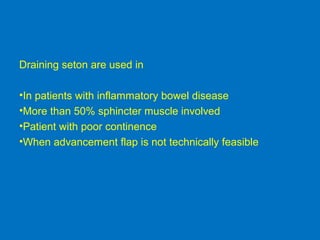
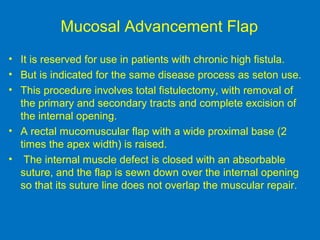
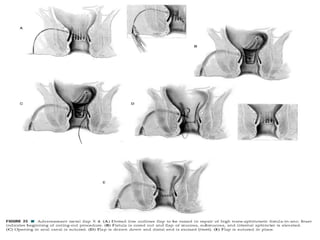
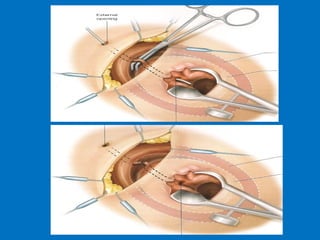
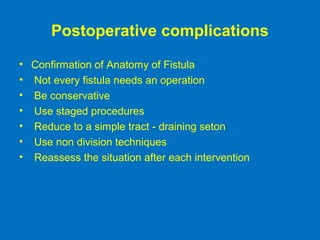
- Treatment depends on the fistula type but may include fistulotomy, seton placement, or drainage of abscesses.