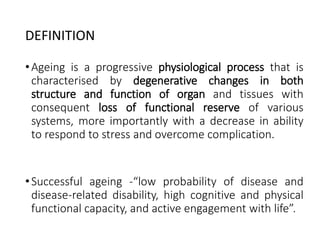
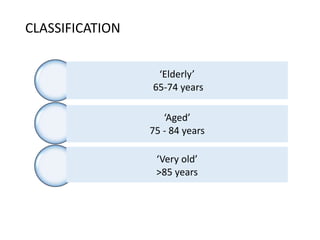
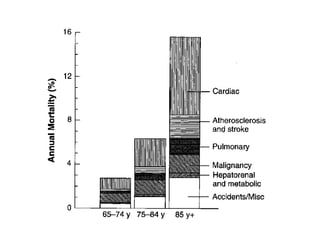
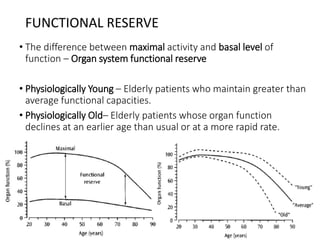
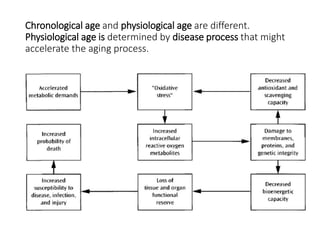
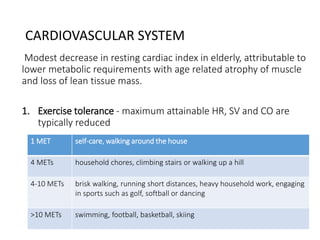
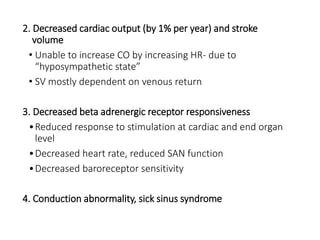
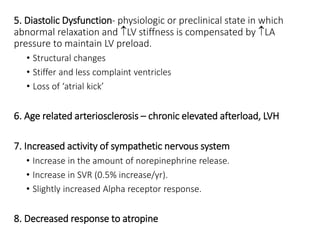
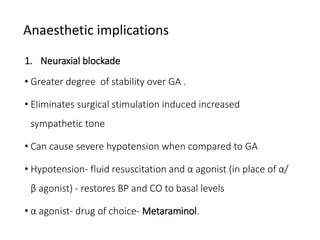
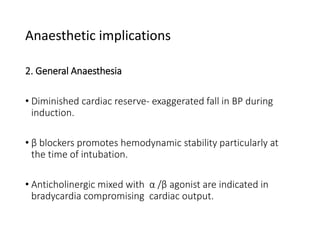
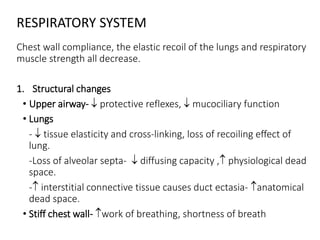
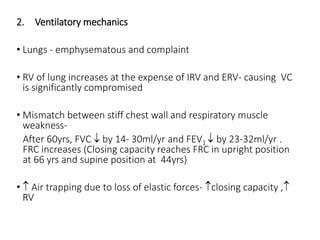
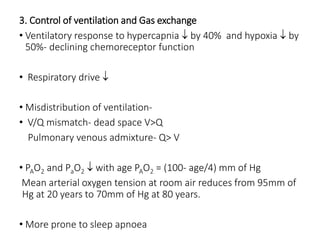
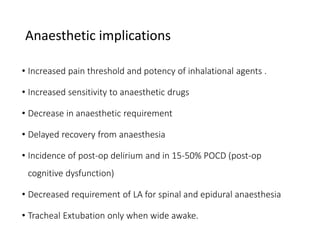
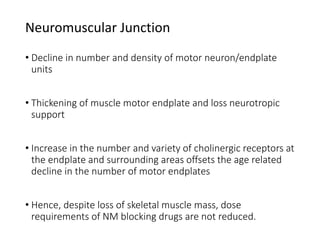
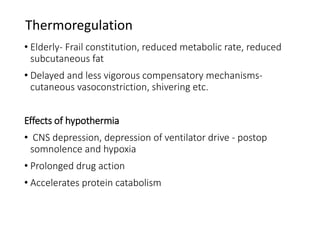
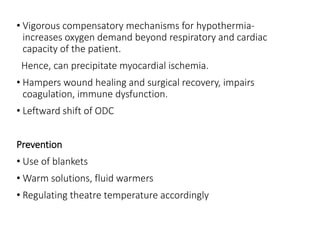
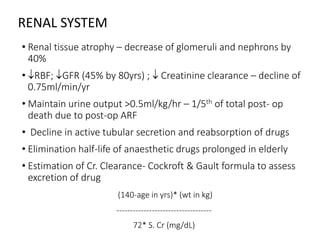
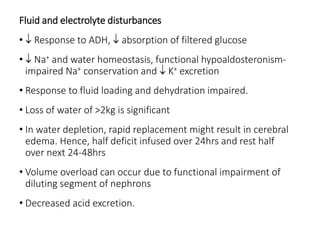
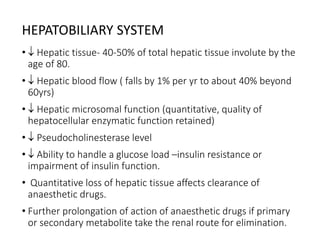
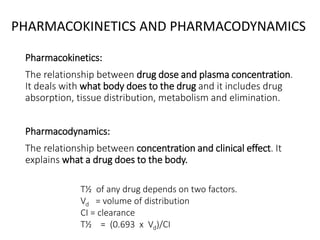
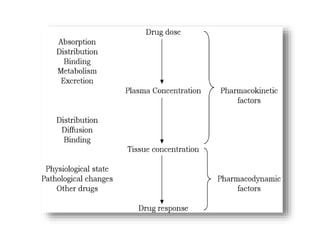
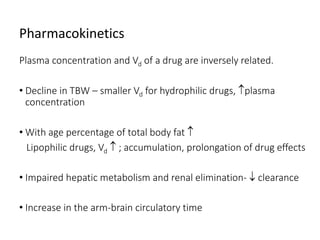
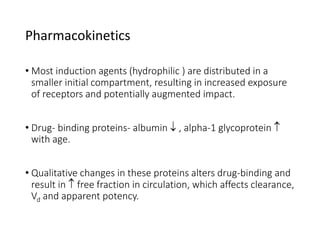
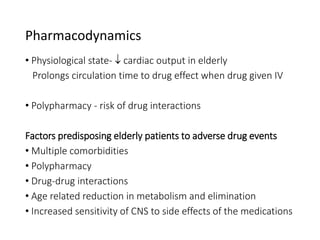
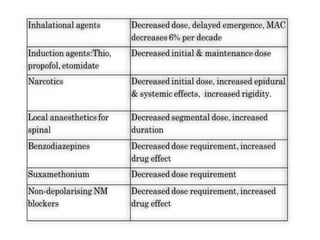
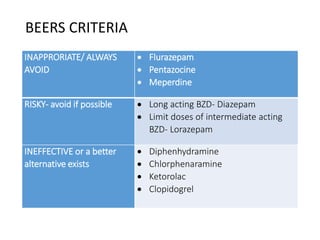
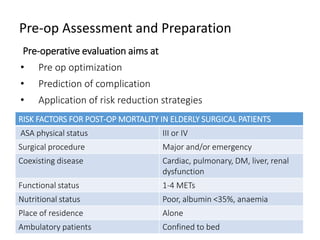
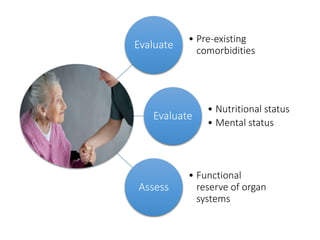
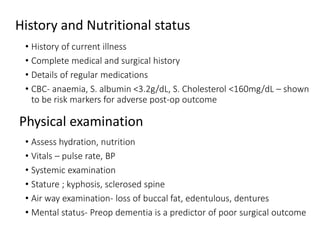
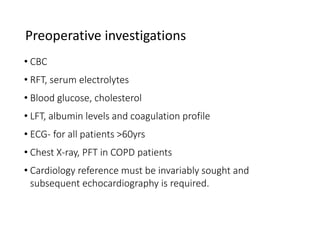
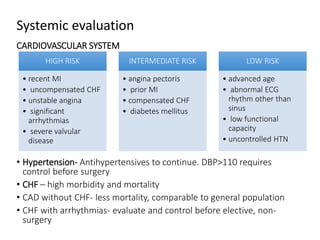
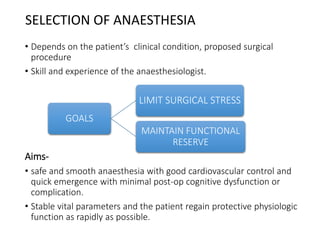
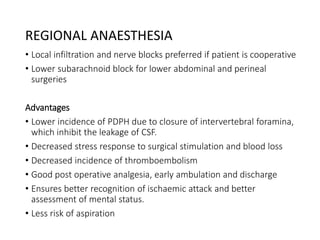
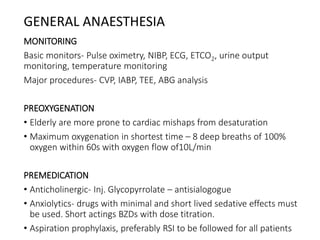
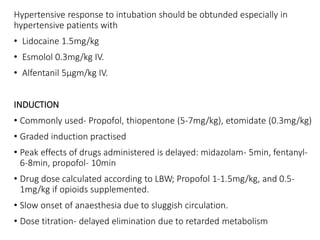
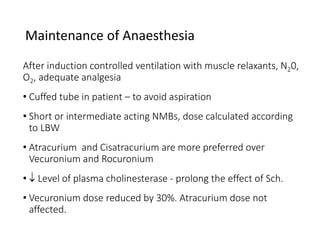
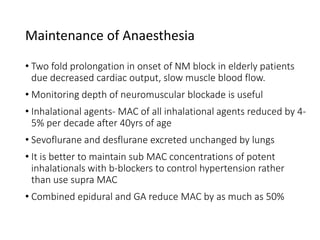
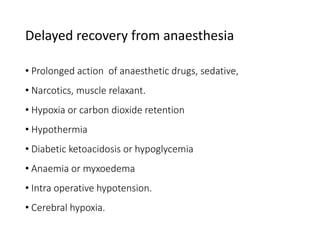
The document provides information on anaesthesia considerations in geriatric patients. It discusses how the aging process impacts various body systems including cardiovascular, respiratory, nervous and renal systems. Key points include decreased organ reserve, altered pharmacokinetics/dynamics requiring adjusted drug dosing, and increased risk of complications. A thorough pre-op assessment of patient health and functional status is important to reduce risks and optimize care for the elderly undergoing surgery.