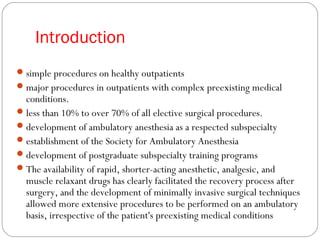
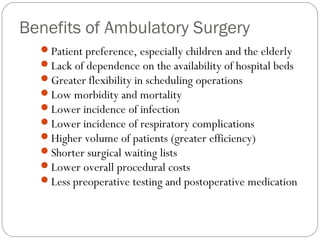
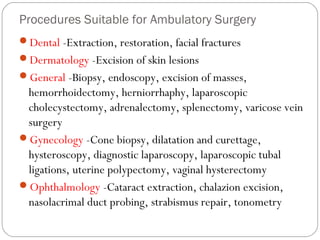
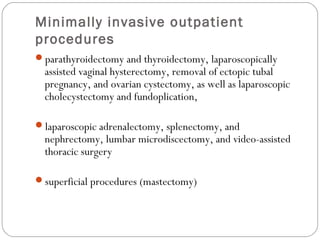
This document discusses ambulatory and fast track anesthesia. It covers topics such as the benefits of ambulatory surgery including lower costs and greater efficiency. It describes different facility designs for ambulatory surgery and lists many common procedures that can be done on an outpatient basis. The document outlines considerations for patient selection and preoperative preparation including pharmacologic and non-pharmacologic techniques. It also discusses various anesthetic techniques for ambulatory surgery like general anesthesia, regional anesthesia, and monitored anesthesia care. Fast tracking approaches to minimize side effects like PONV are also summarized.
































![FAST TRACKING
Bypassing the PACU has been termed “fast-tracking” after
ambulatory surgery.
In addition, fast-tracking can be accomplished directly from
the PACU (“PACU fast-tracking”) by creating a specialized
area within an existing PACU where recovery procedures
are organized along the lines of a step-down unit.
This approach represents a key component of the “total
care” package for ambulatory surgery.[463]](https://image.slidesharecdn.com/ambulatoryanaesthesia-150602065309-lva1-app6892/85/Ambulatory-anaesthesia-37-320.jpg)

![Fast-Tracking
Multimodal Approaches to Minimize Side
Effects
PONV- droperidol 0.625-1.25 mg IV, dexamethasone 4-8 mg IV,
ondansetron 4-8 mg IV, long-acting 5-HT3 antagonist-
palonosetron 75 µg IV, and NK-1 antagonist - aprepitant, a
transdermal scopolamine patch, or an acu-stimulation
device - SeaBand, Relief Band
Non-opioid analgesics -NSAIDs, cyclooxygenase-2 [COX-
2] inhibitors, acetaminophen, 2-agonists,α
glucocorticoids, ketamine, and local anesthetics](https://image.slidesharecdn.com/ambulatoryanaesthesia-150602065309-lva1-app6892/85/Ambulatory-anaesthesia-39-320.jpg)








