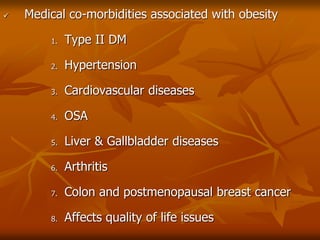
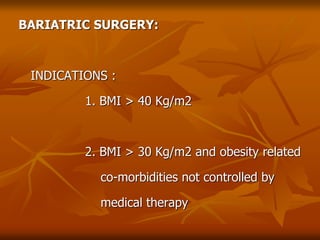
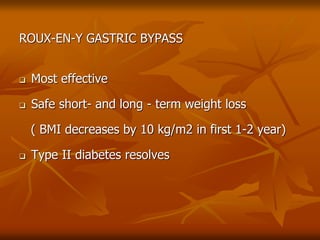
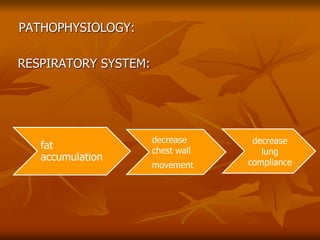
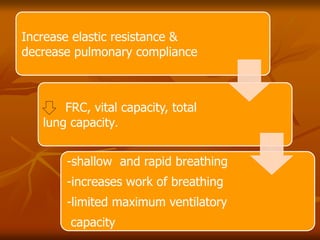
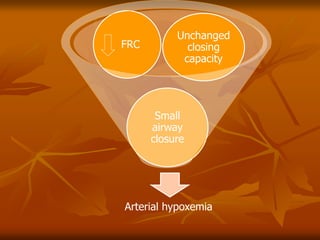
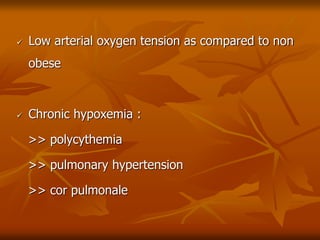
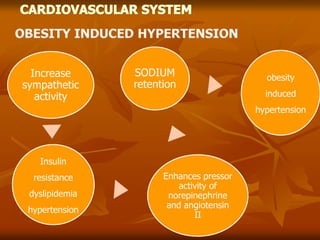
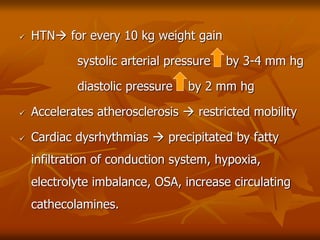
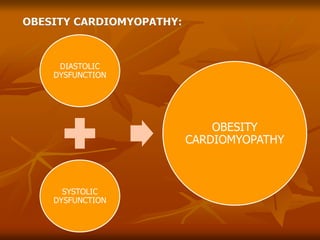
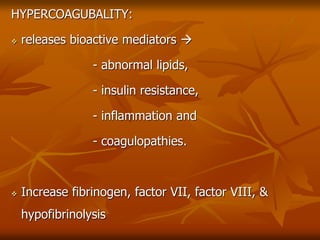
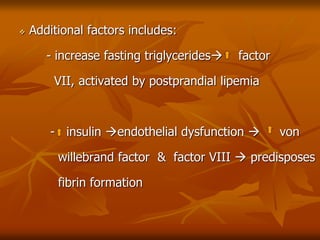
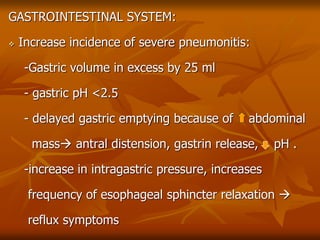
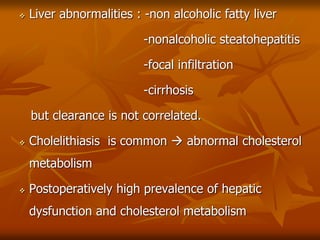
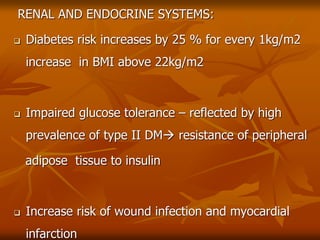
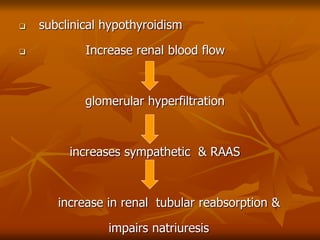
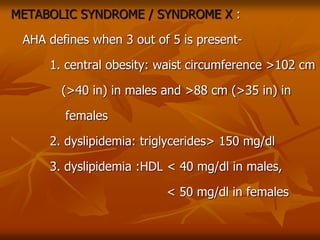
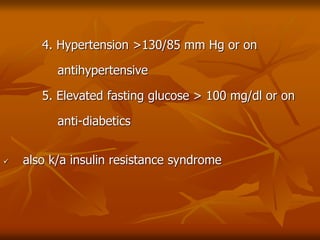
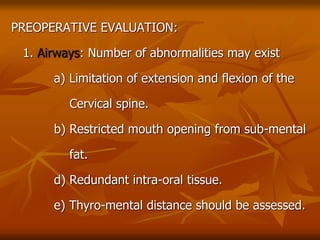
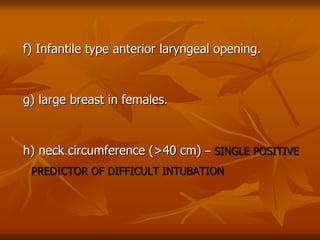
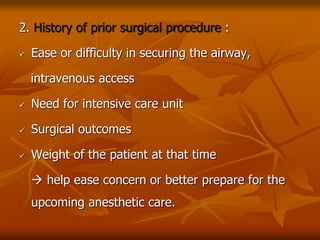
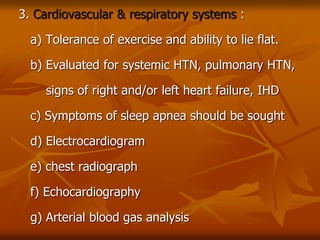
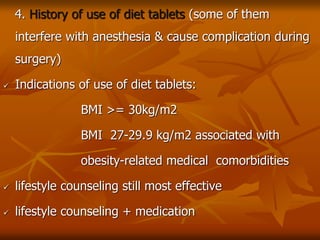
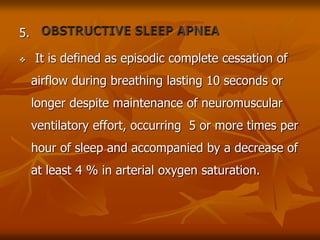
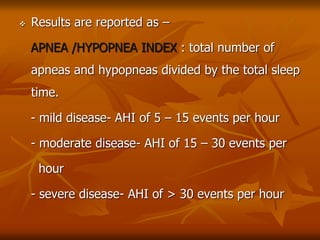
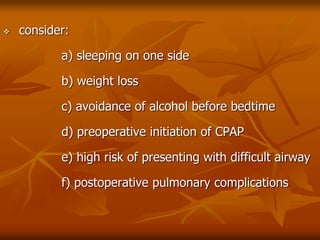
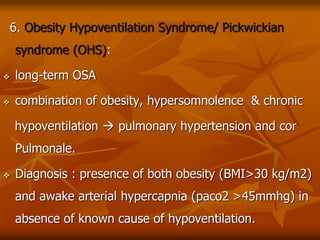
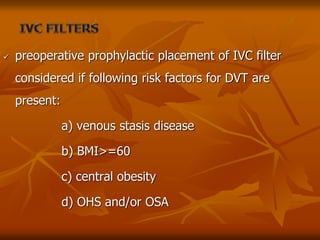
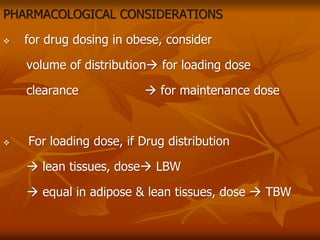
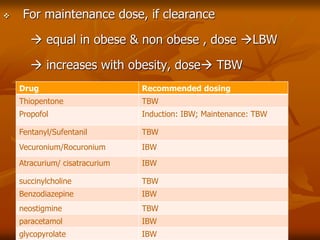
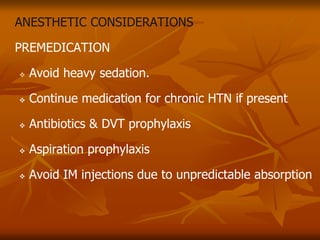
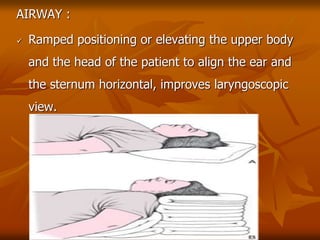
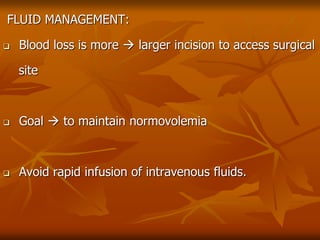
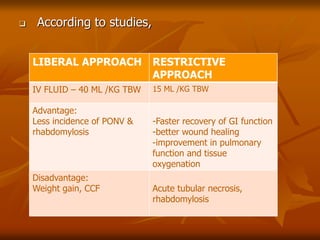
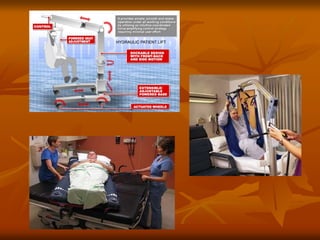
The document discusses anesthesia considerations for bariatric surgery. It notes that obesity is associated with various comorbidities affecting the respiratory, cardiovascular, gastrointestinal and other body systems. The anesthesia plan involves a thorough preoperative evaluation of the patient's airway, cardiac function, respiratory status, risk of venous thromboembolism, and metabolic/nutritional abnormalities. Careful dosing of anesthetic drugs based on lean or total body weight is also required. The goal of anesthesia is to safely induce and maintain anesthesia for bariatric surgery while addressing the unique health risks faced by obese patients.