This document provides information about obesity, including definitions, classifications, causes, comorbidities, and treatments. It discusses:
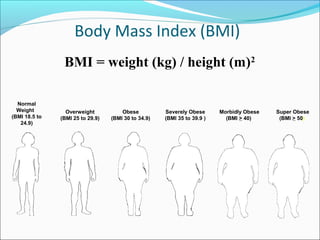
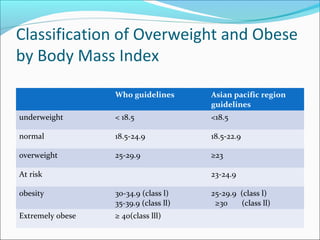
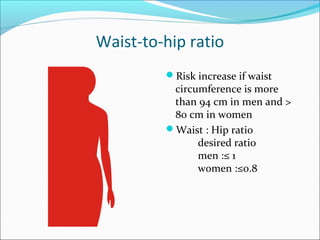
- Definitions of obesity based on body mass index (BMI) and classifications of overweight and obesity.
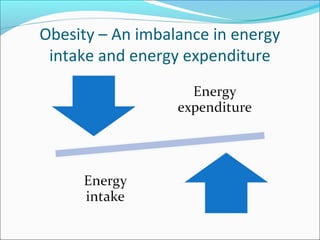
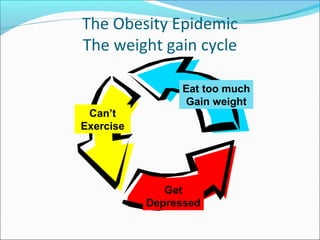
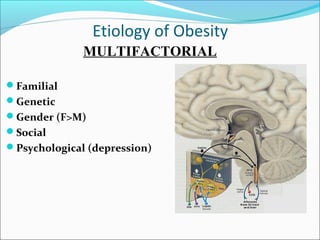
- Causes of obesity including genetic, hormonal, environmental, and behavioral factors.
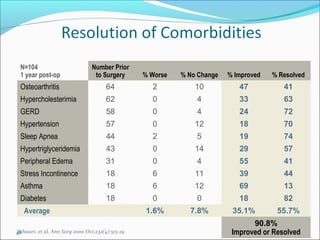
- Common obesity-related health conditions or comorbidities such as diabetes, heart disease, sleep apnea, cancer, and arthritis.
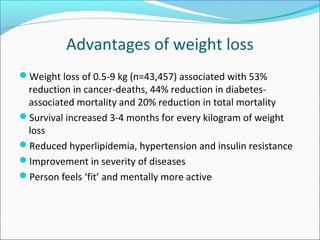
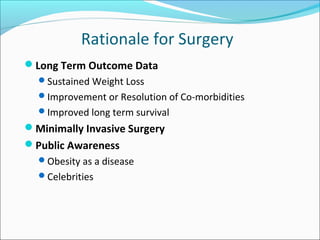
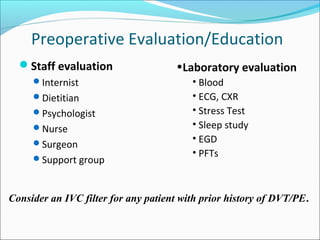
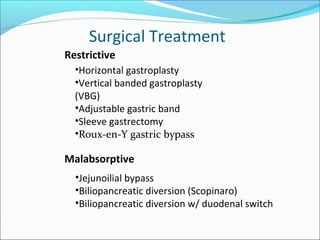
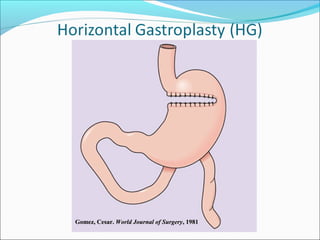
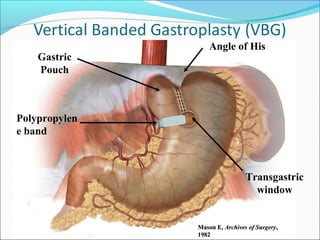
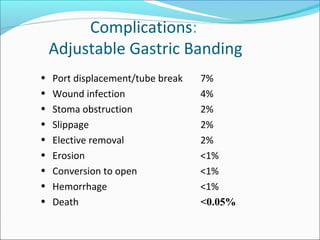
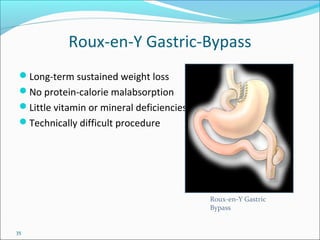
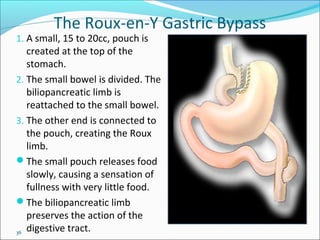
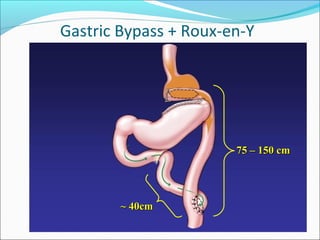
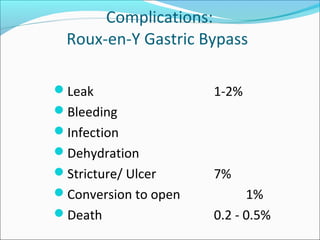
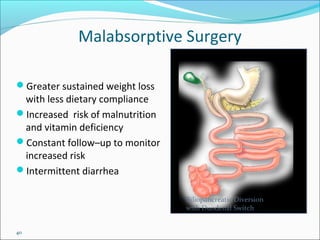
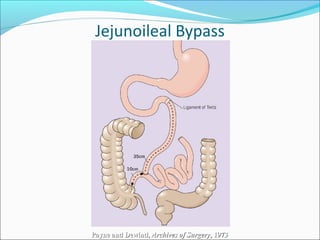
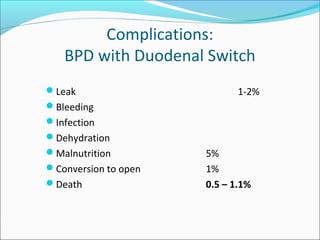
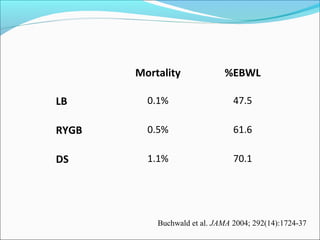
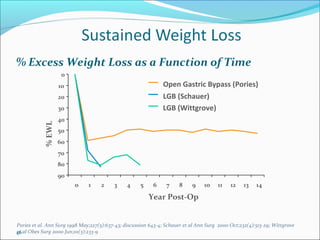
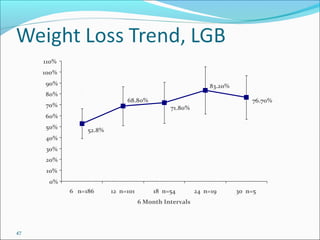
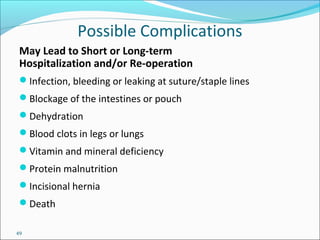
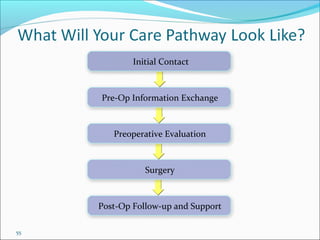
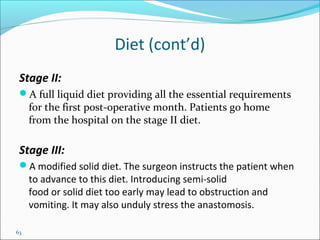
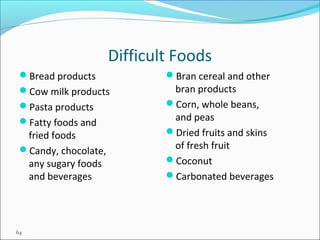
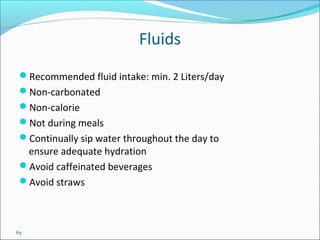
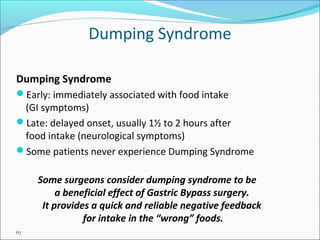
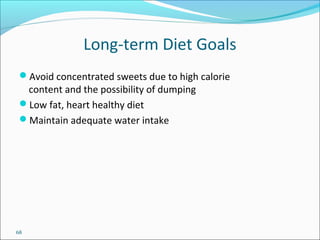
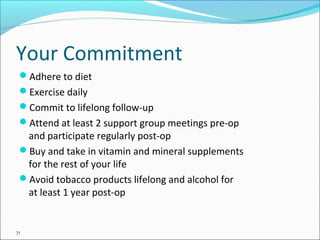
- Treatment options for obesity including lifestyle changes, medications, bariatric surgery procedures like gastric bypass and banding, and their risks and effectiveness. Bariatric surgery can result in significant and long-term weight loss and improvement of comorbidities.