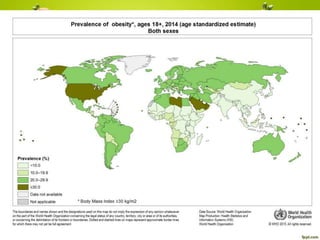
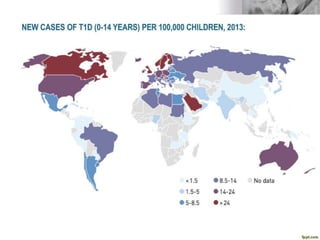
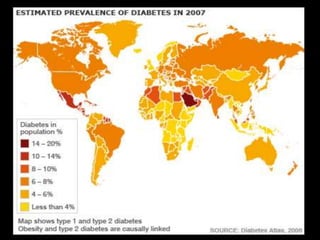
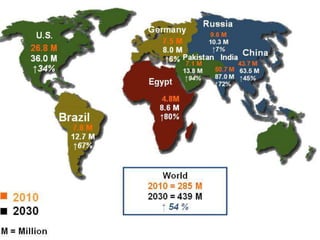
This document discusses childhood obesity including its definition, epidemiology, risk factors, causes, evaluation, treatment, and management. Some key points include:
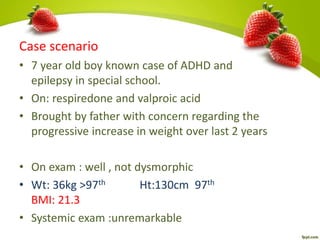
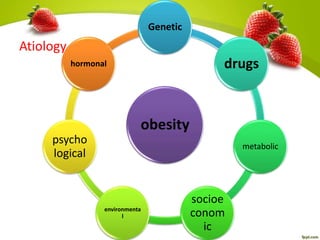
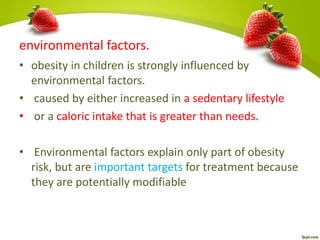
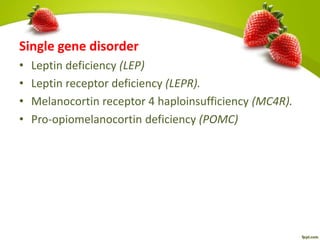
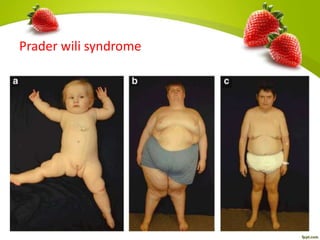
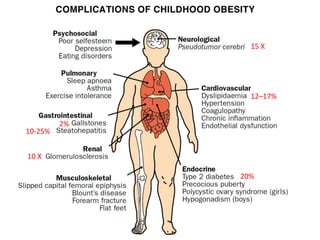
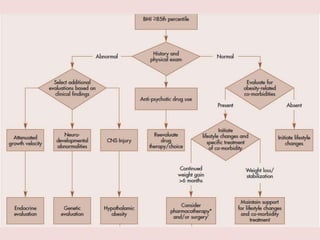
- Childhood obesity is defined as a BMI at or above the 95th percentile for age and sex. It can be caused by genetic and environmental factors.
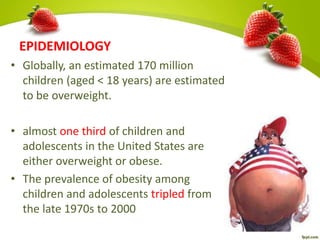
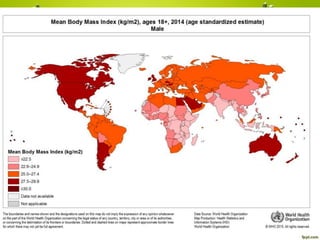
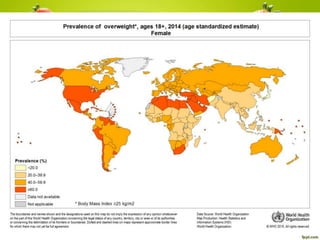
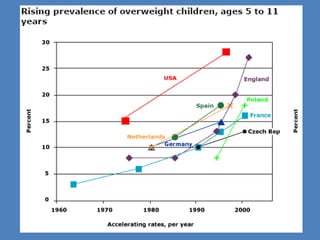
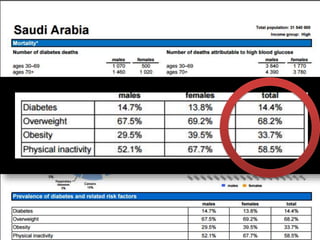
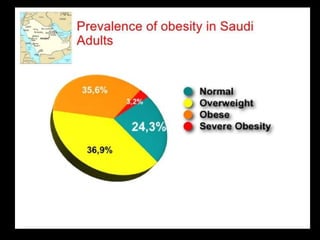
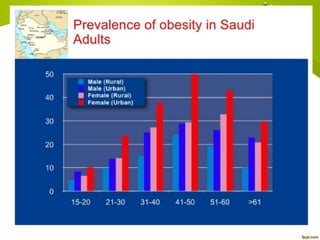
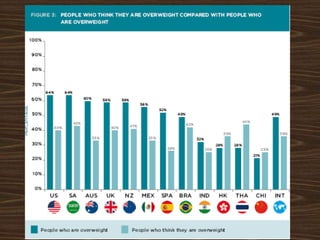
- Rates of childhood obesity have tripled since the 1970s globally and in countries like the US and KSA. Risk factors include family history, low income, and lack of physical activity.
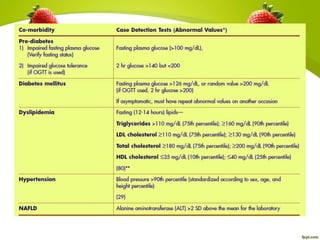
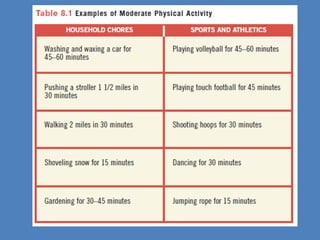
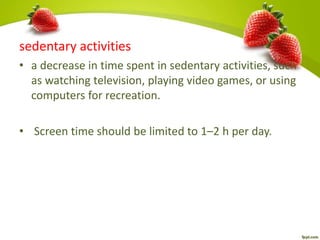
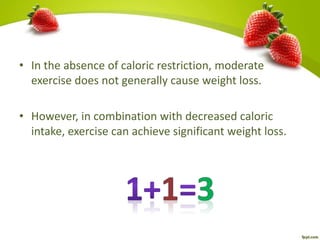
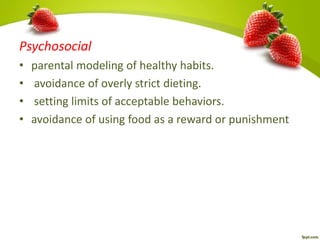
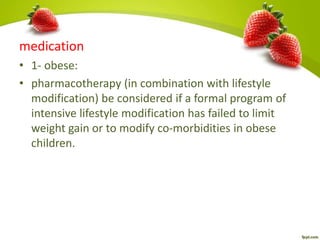
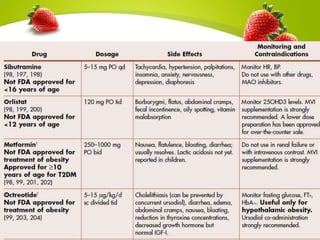
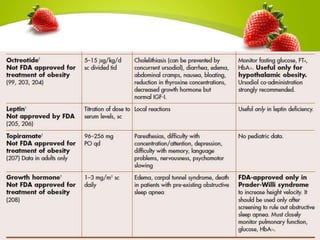
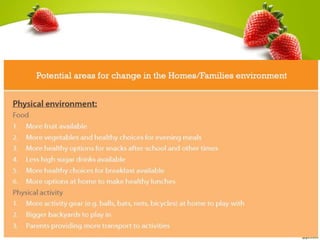
- Evaluation of an obese child includes medical history, exam, and tests to check for underlying causes and comorbidities. Treatment focuses on lifestyle changes like diet, exercise, and behavior modification for the whole