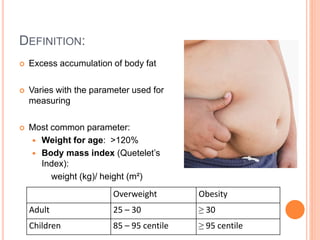
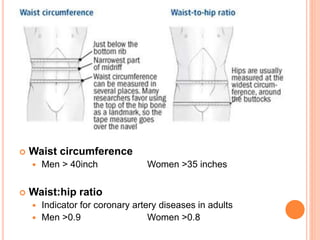
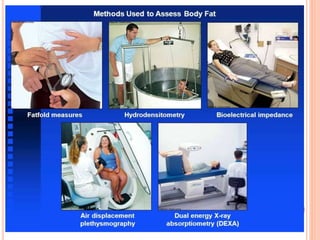
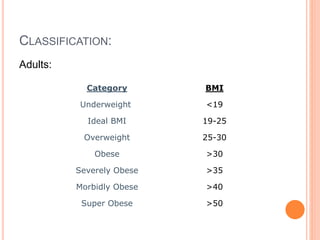
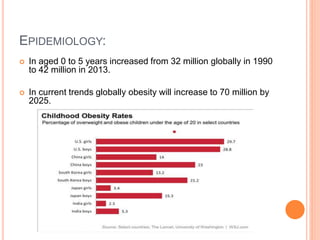
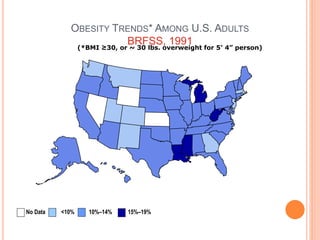
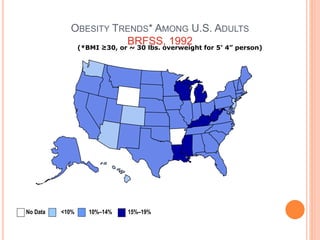
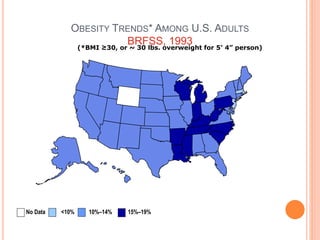
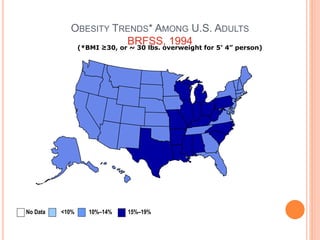
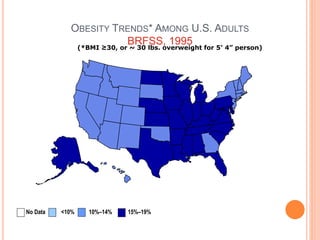
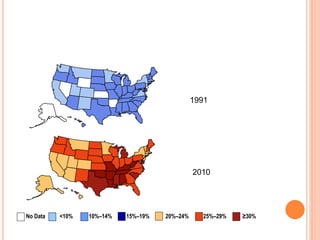
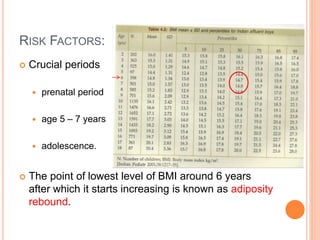
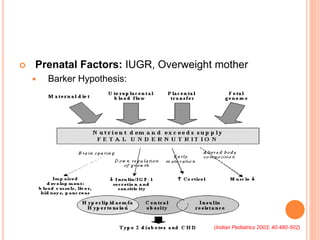
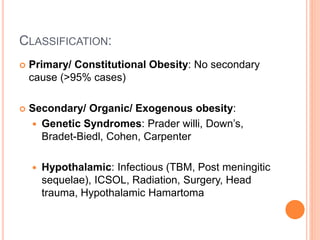
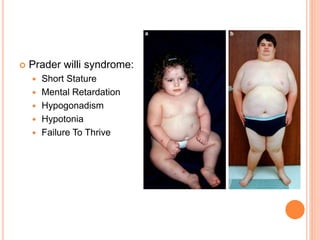
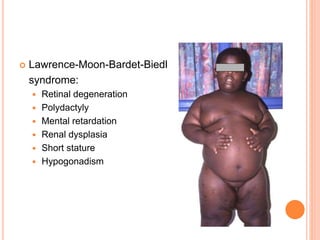
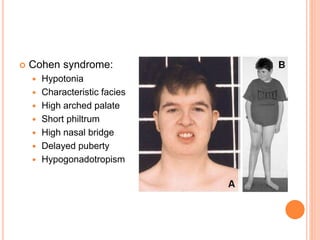
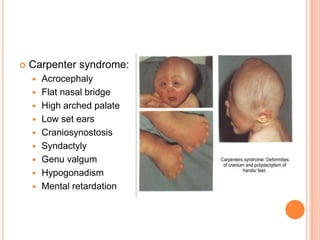
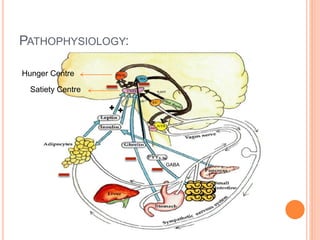
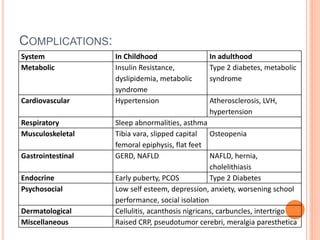
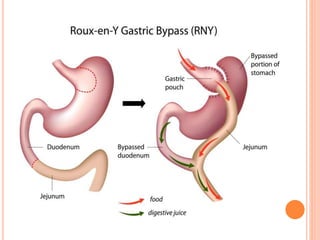
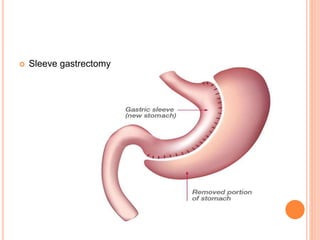
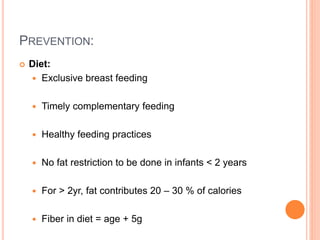
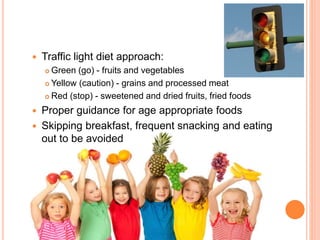
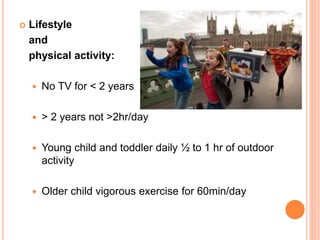
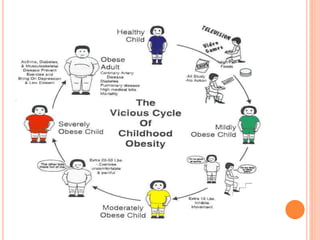
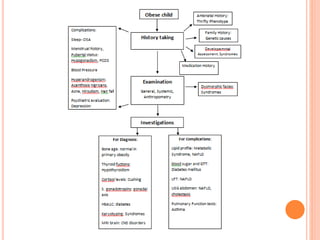
The document discusses childhood obesity, its definitions, and classification, highlighting that obesity rates in children globally have risen significantly, particularly in developing countries like India. It outlines epidemiology, risk factors, pathophysiology, evaluations, management strategies, and prevention techniques, while also referencing the WHO's initiative to address the issue. The need for multidisciplinary approaches, including dietary changes, physical activity, and potential pharmacological or surgical interventions, is emphasized to combat this growing health concern.