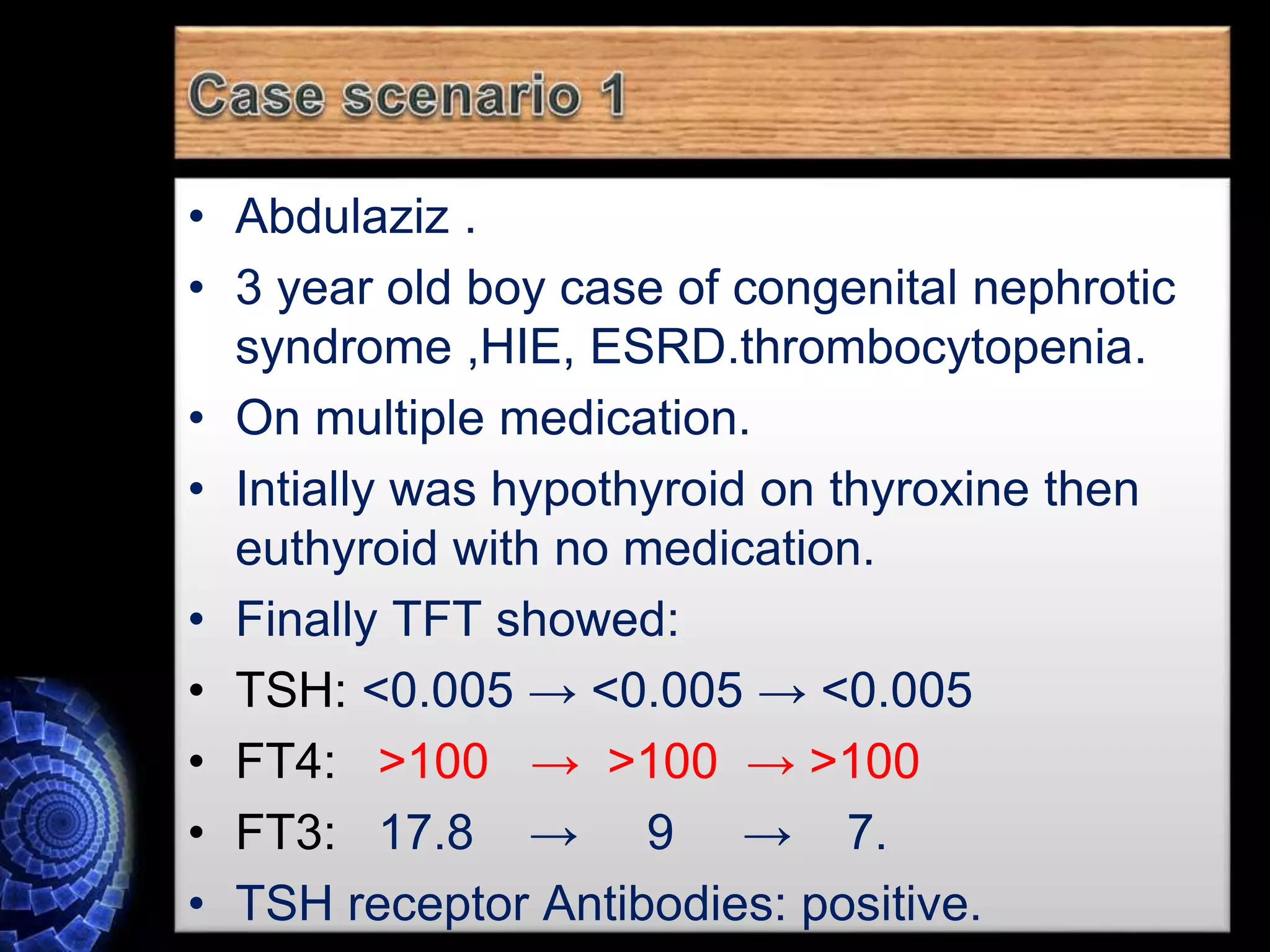
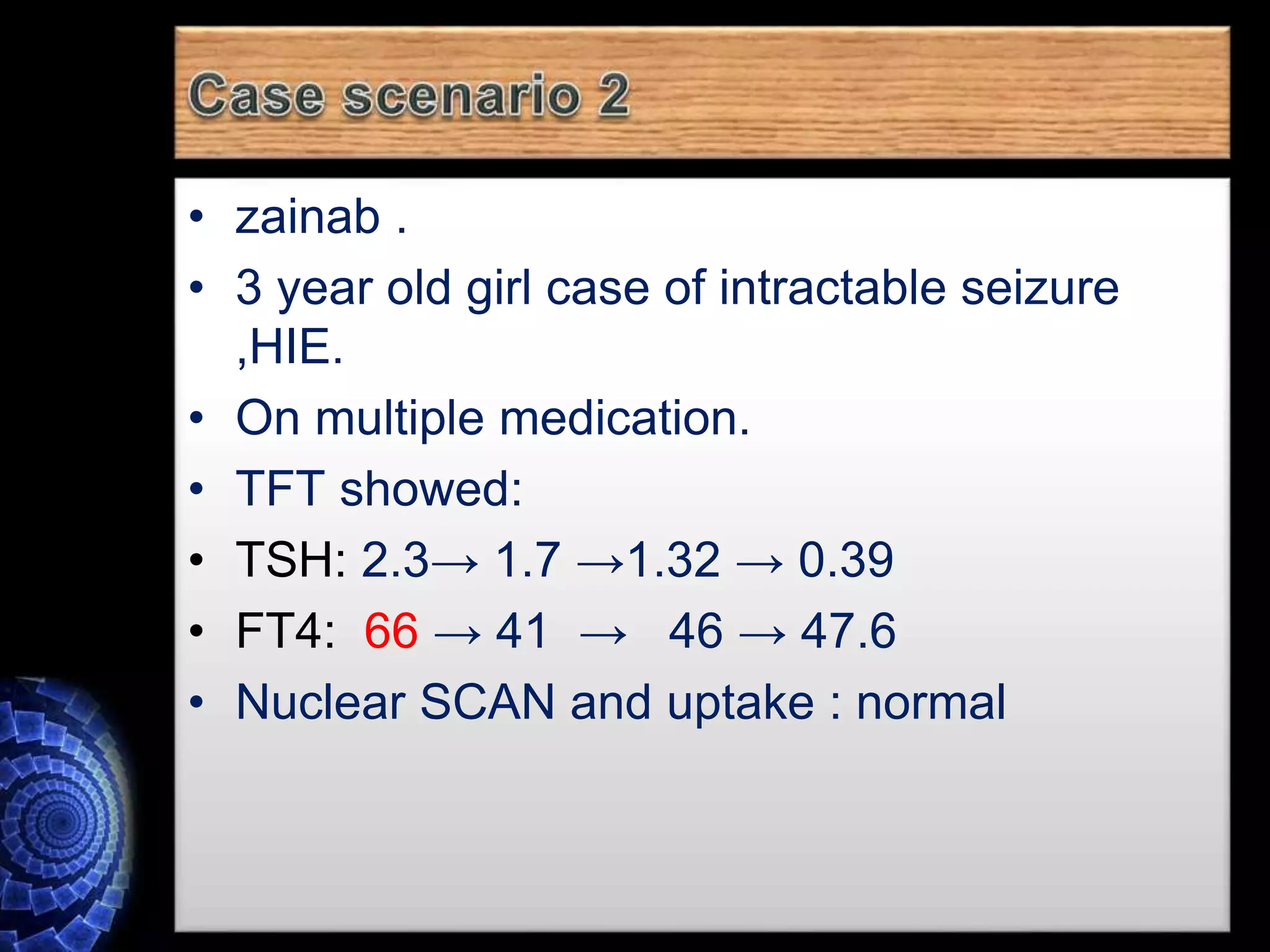
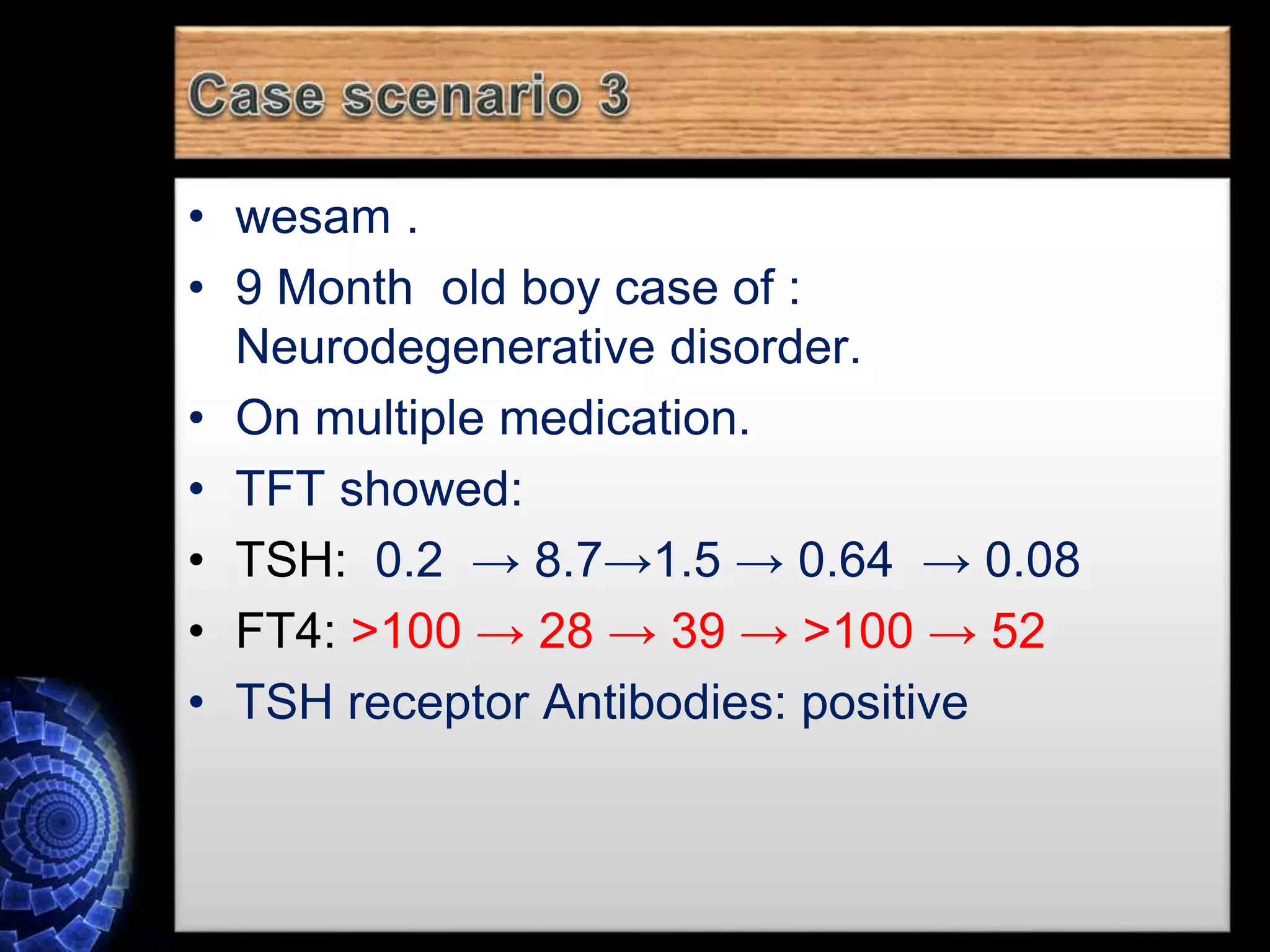
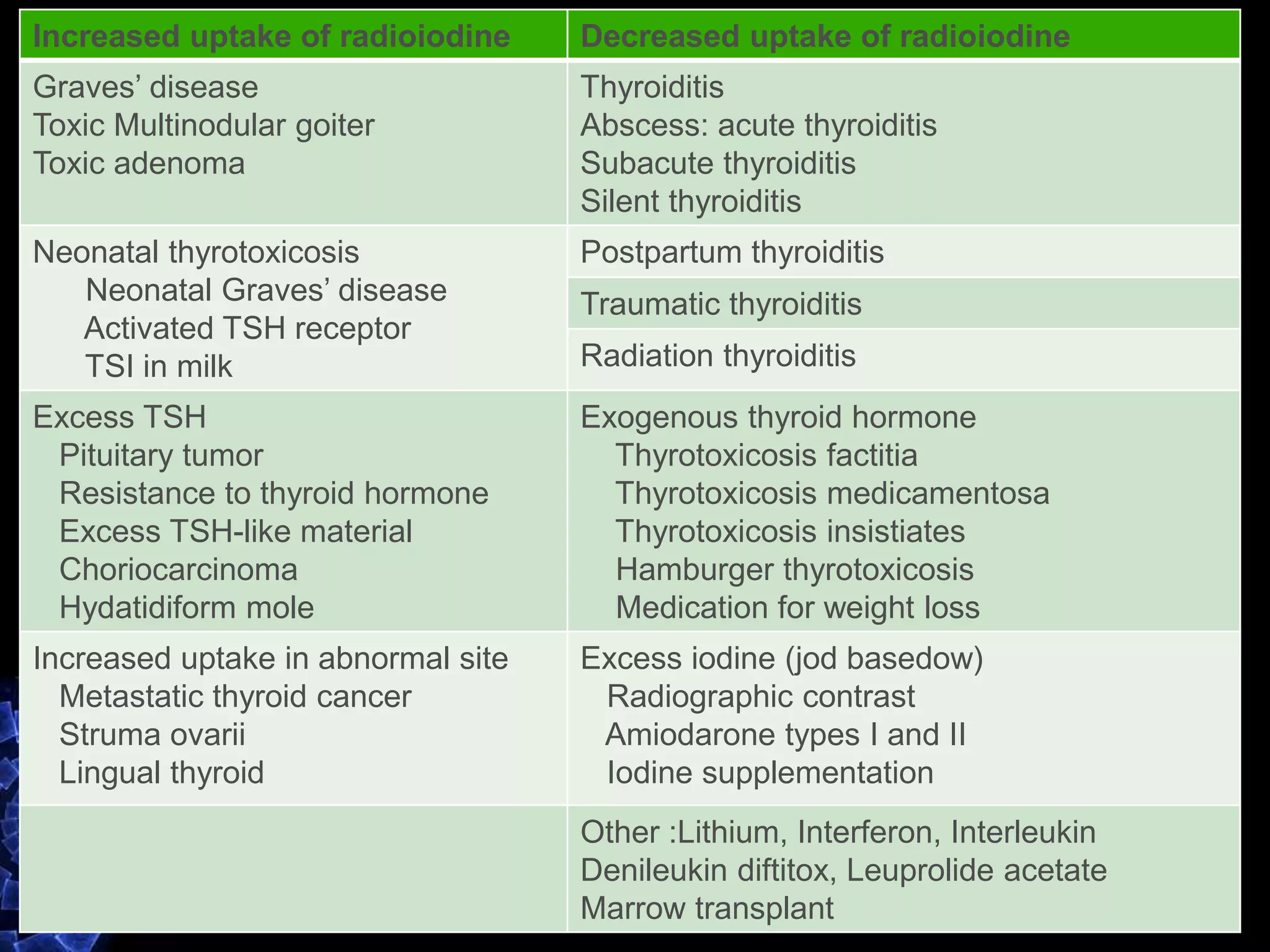
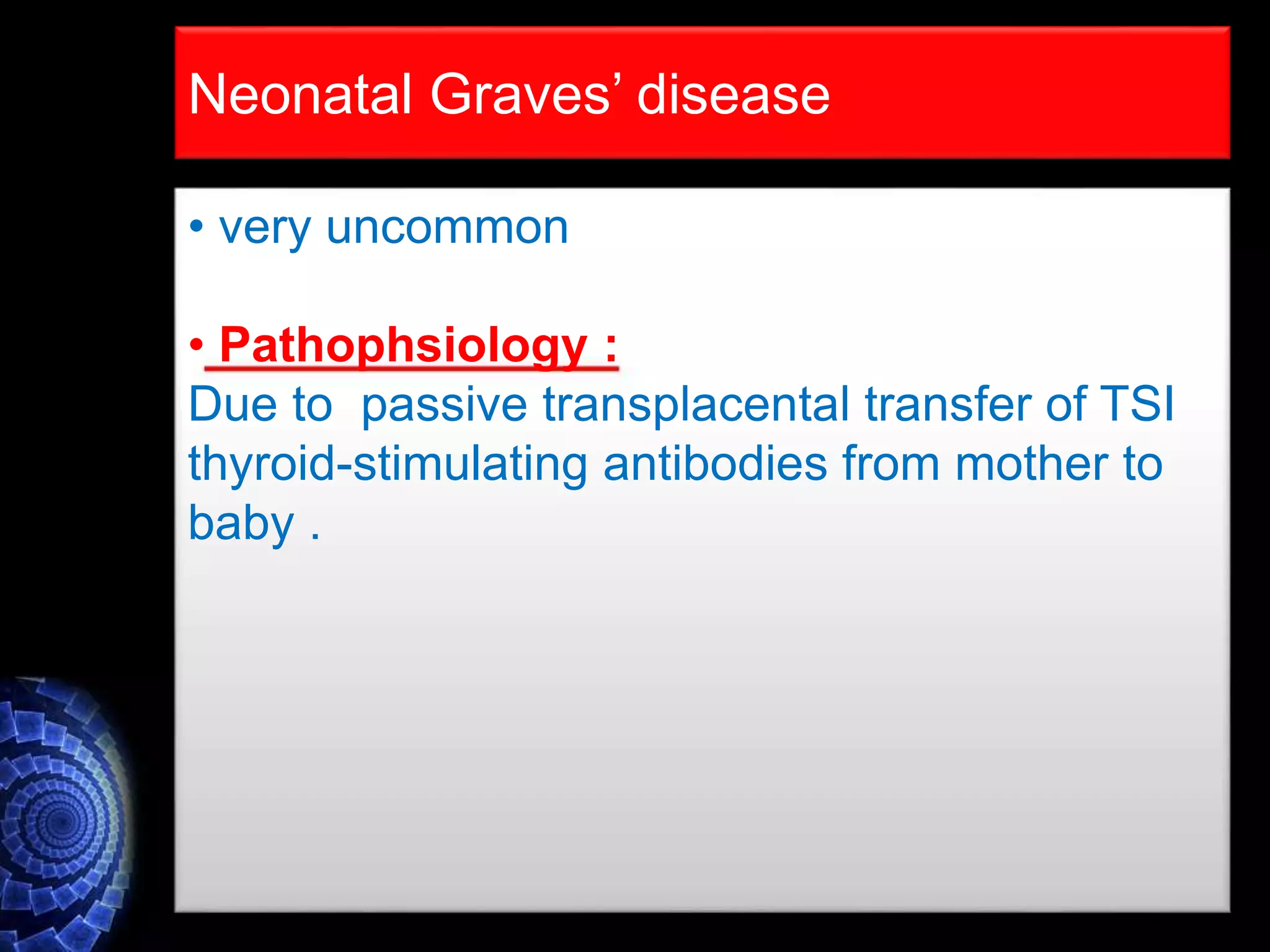
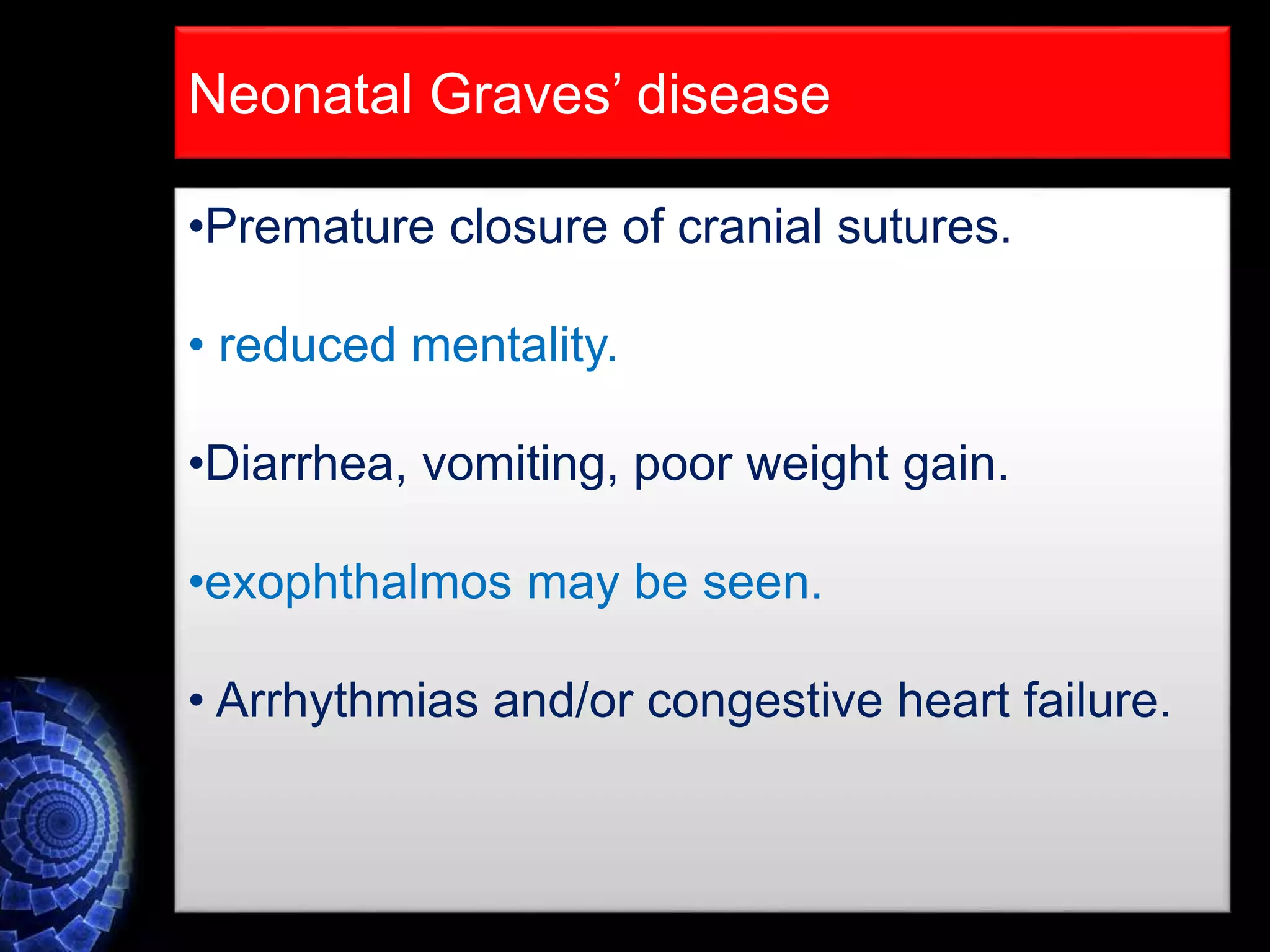
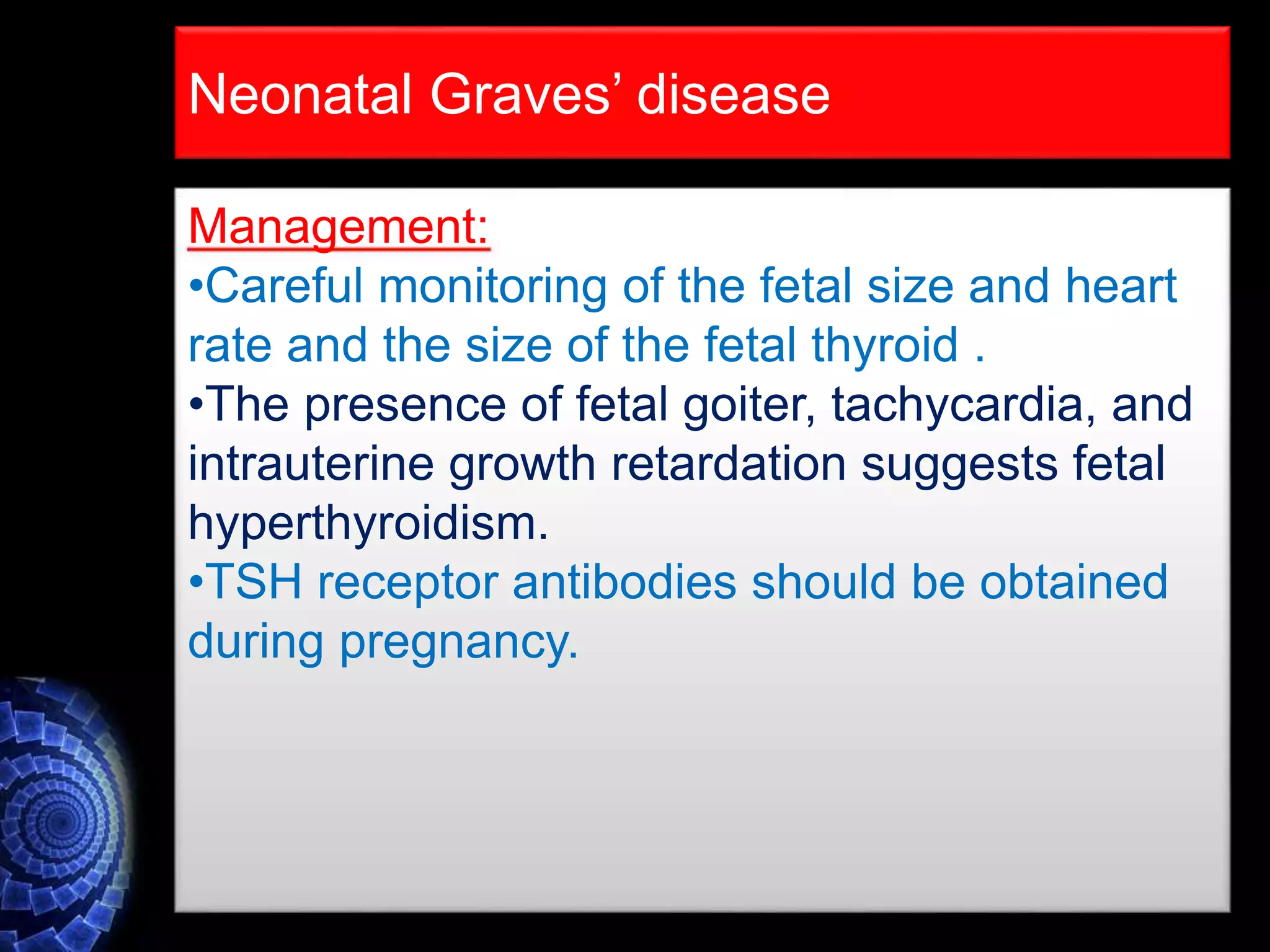
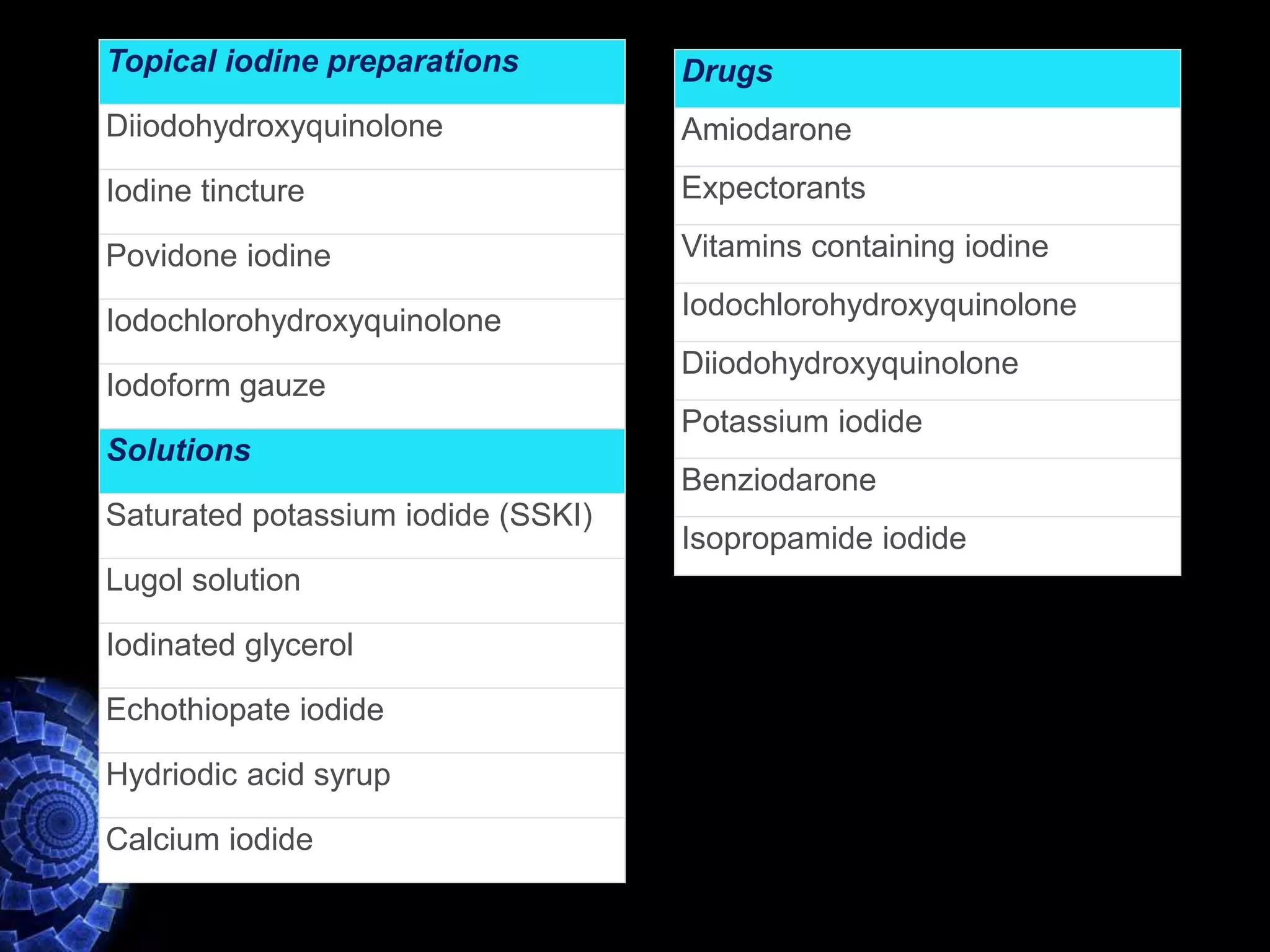
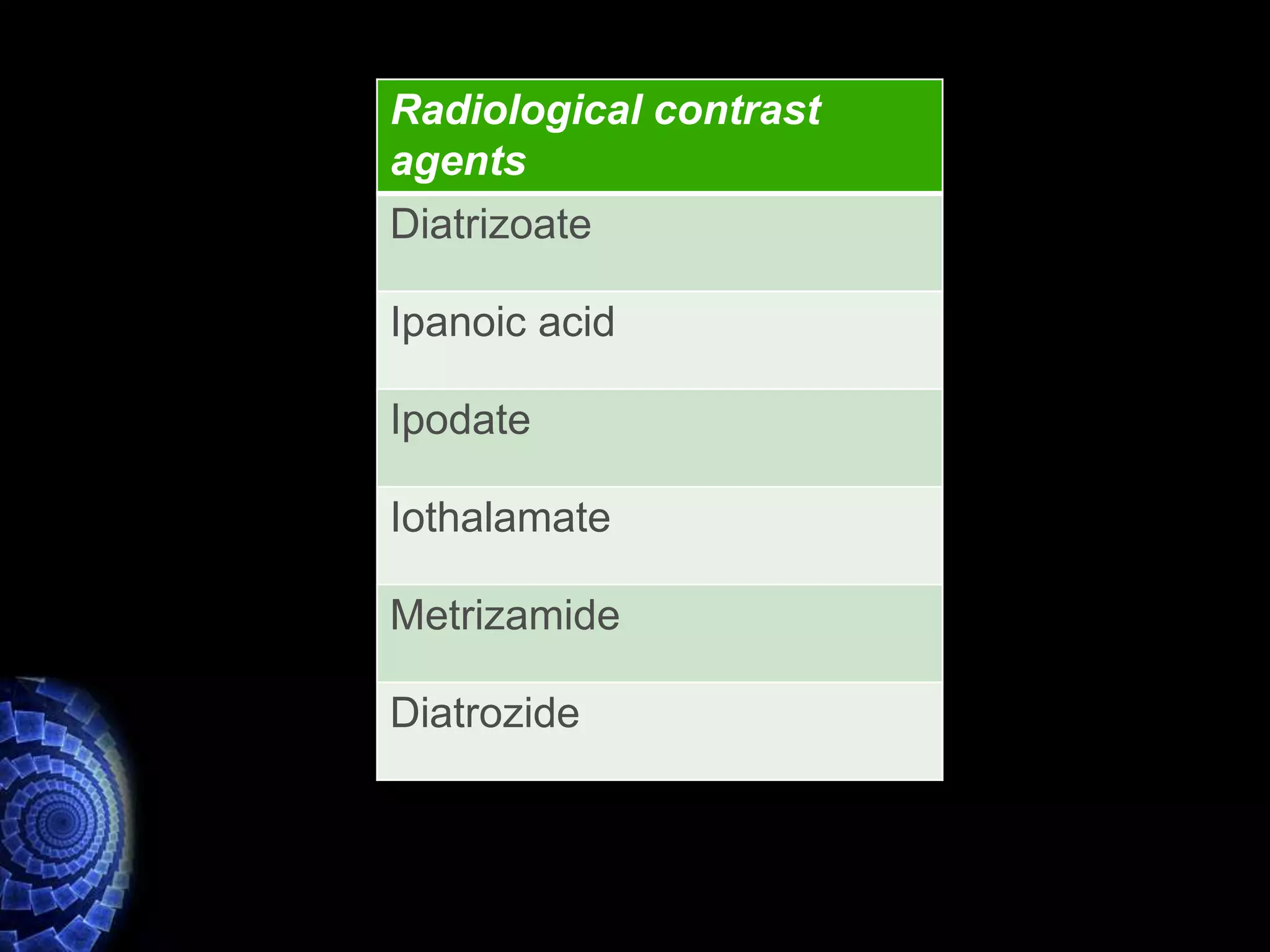
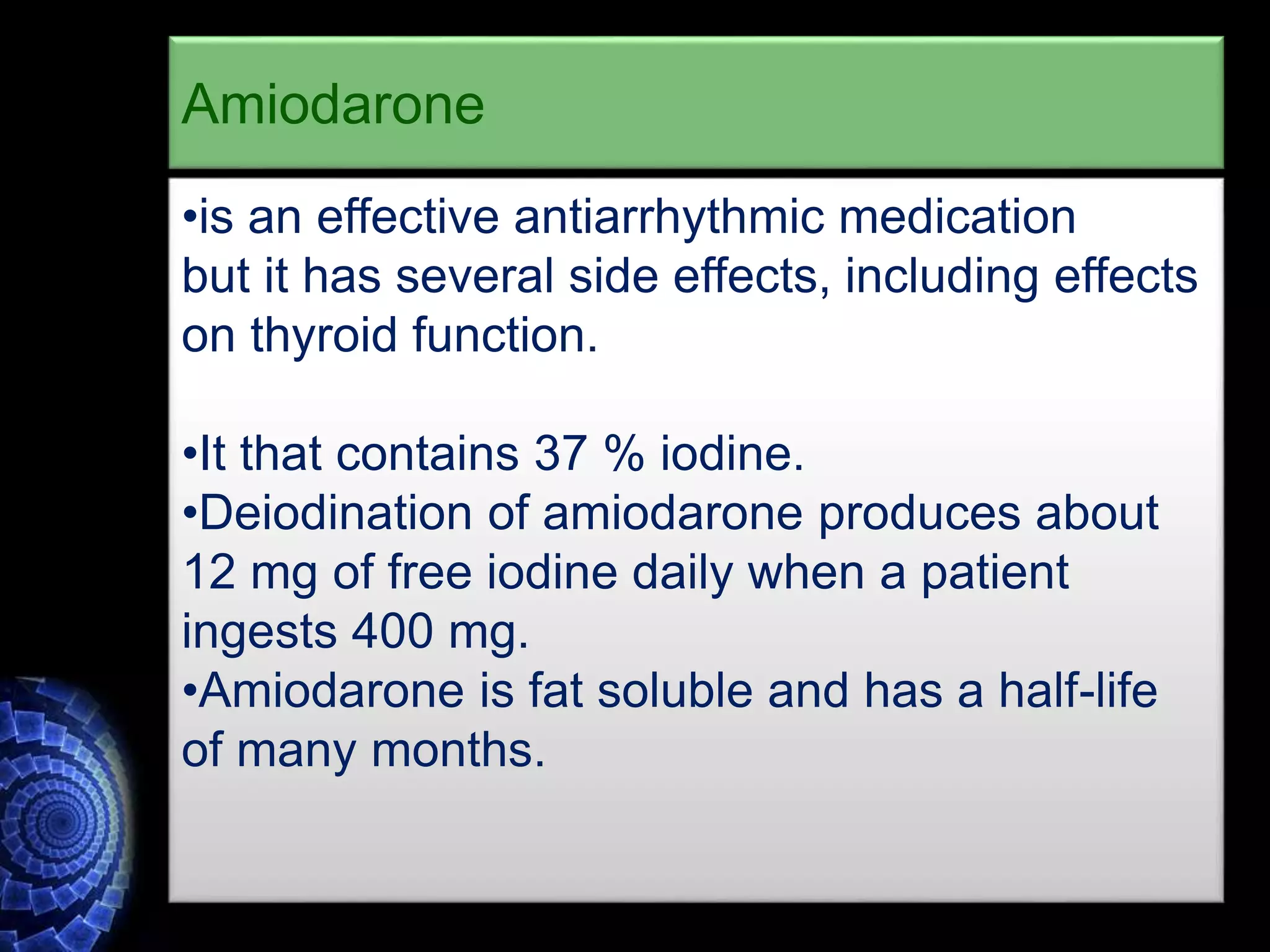
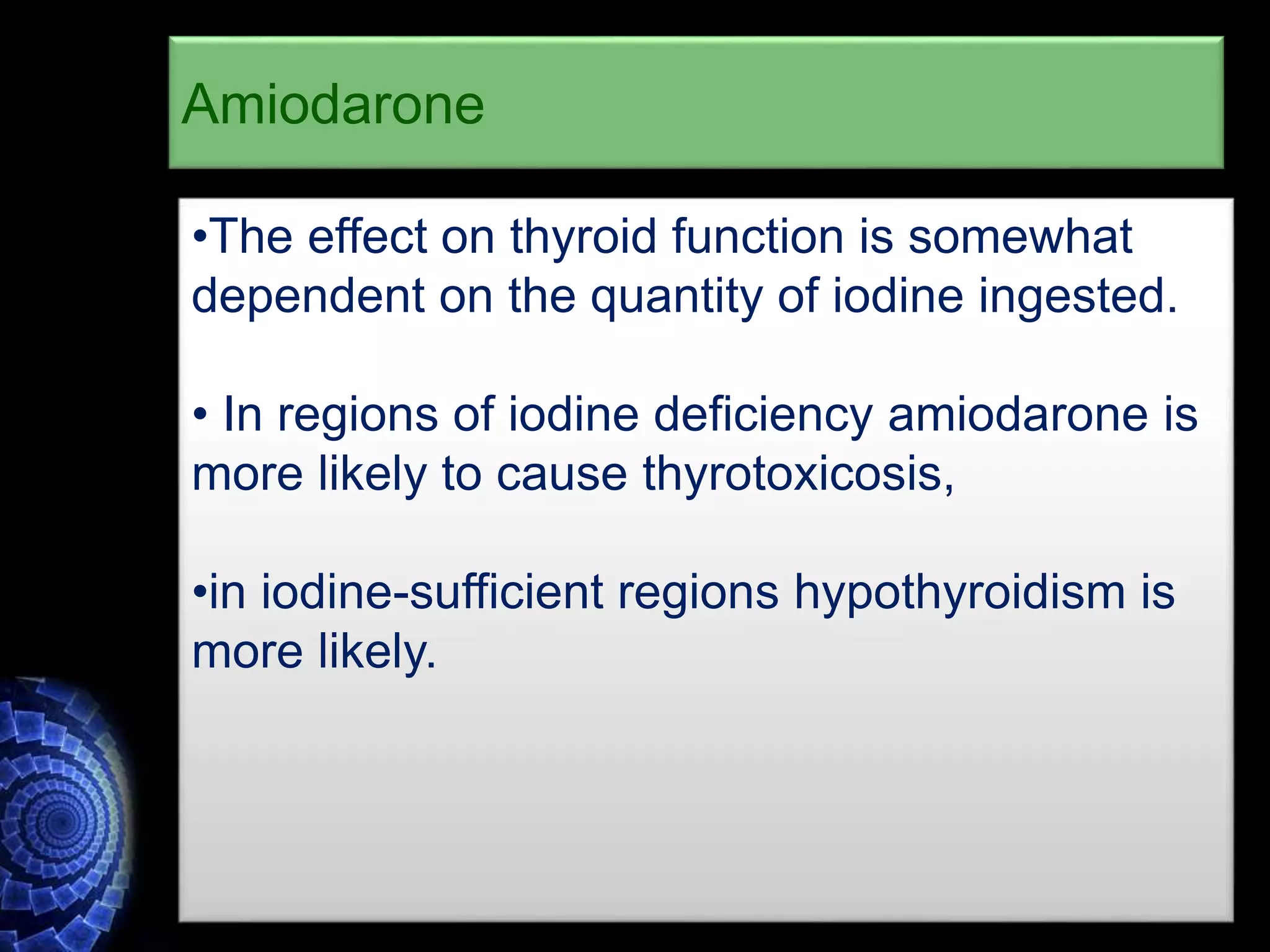
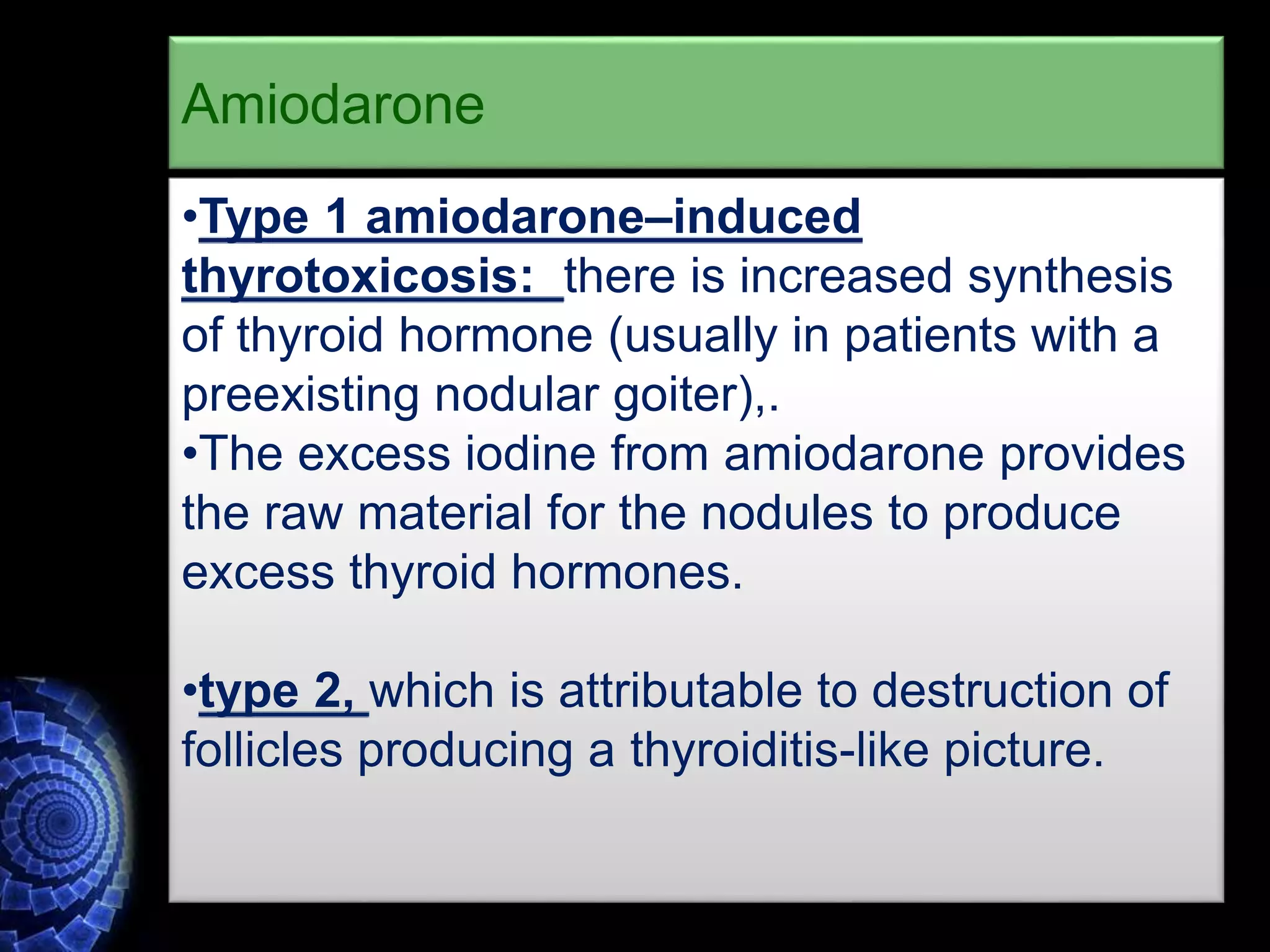
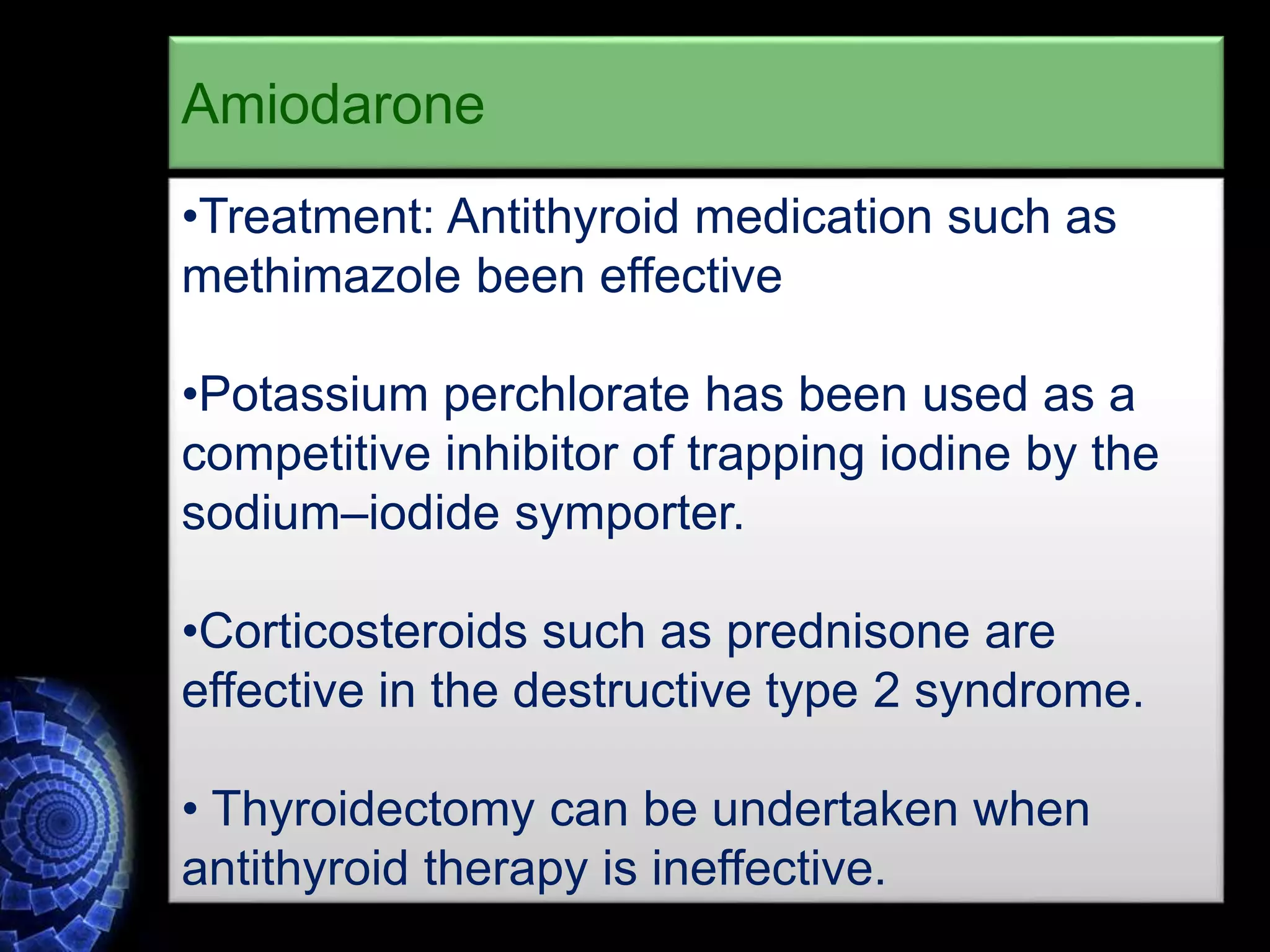
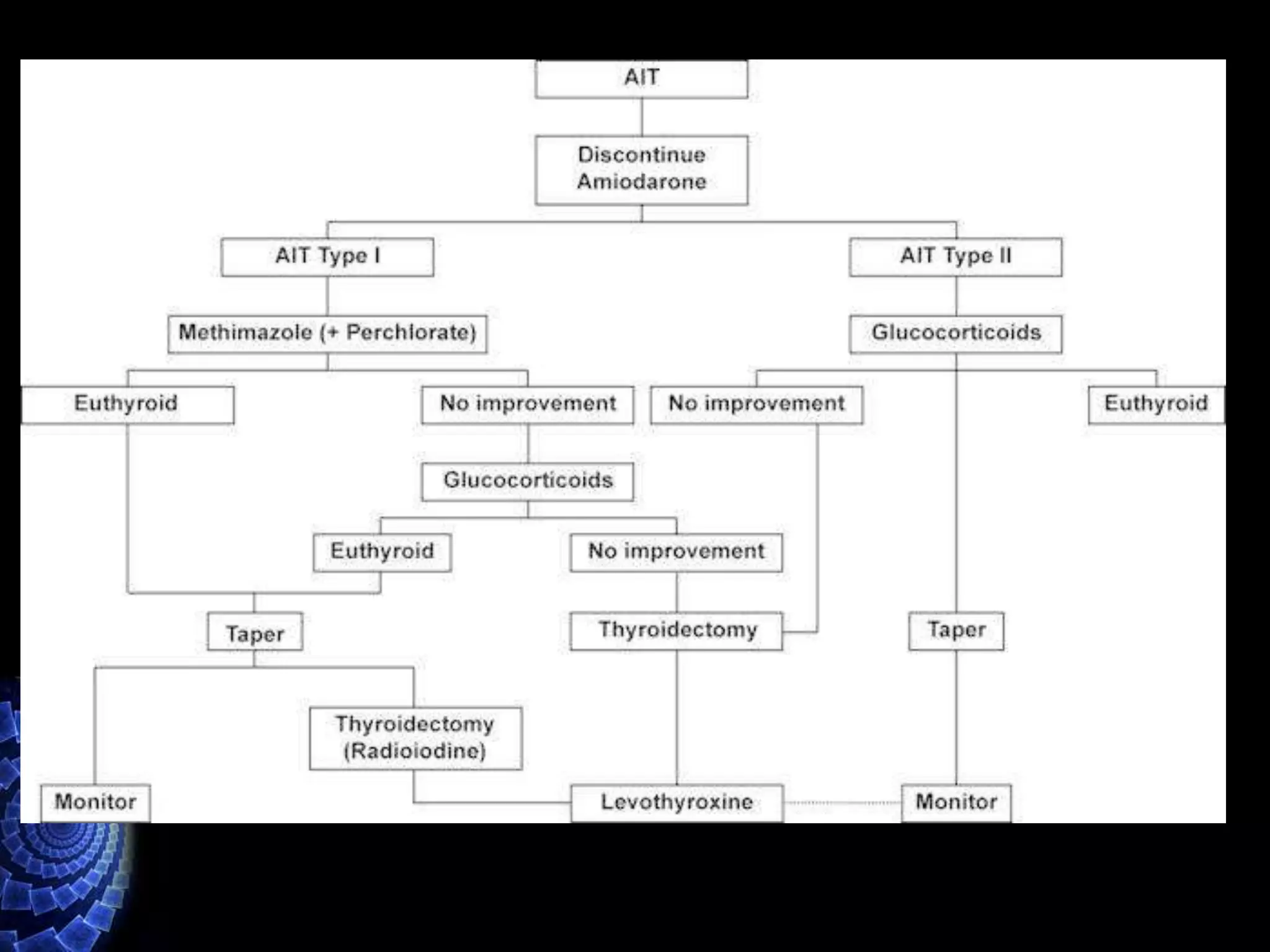
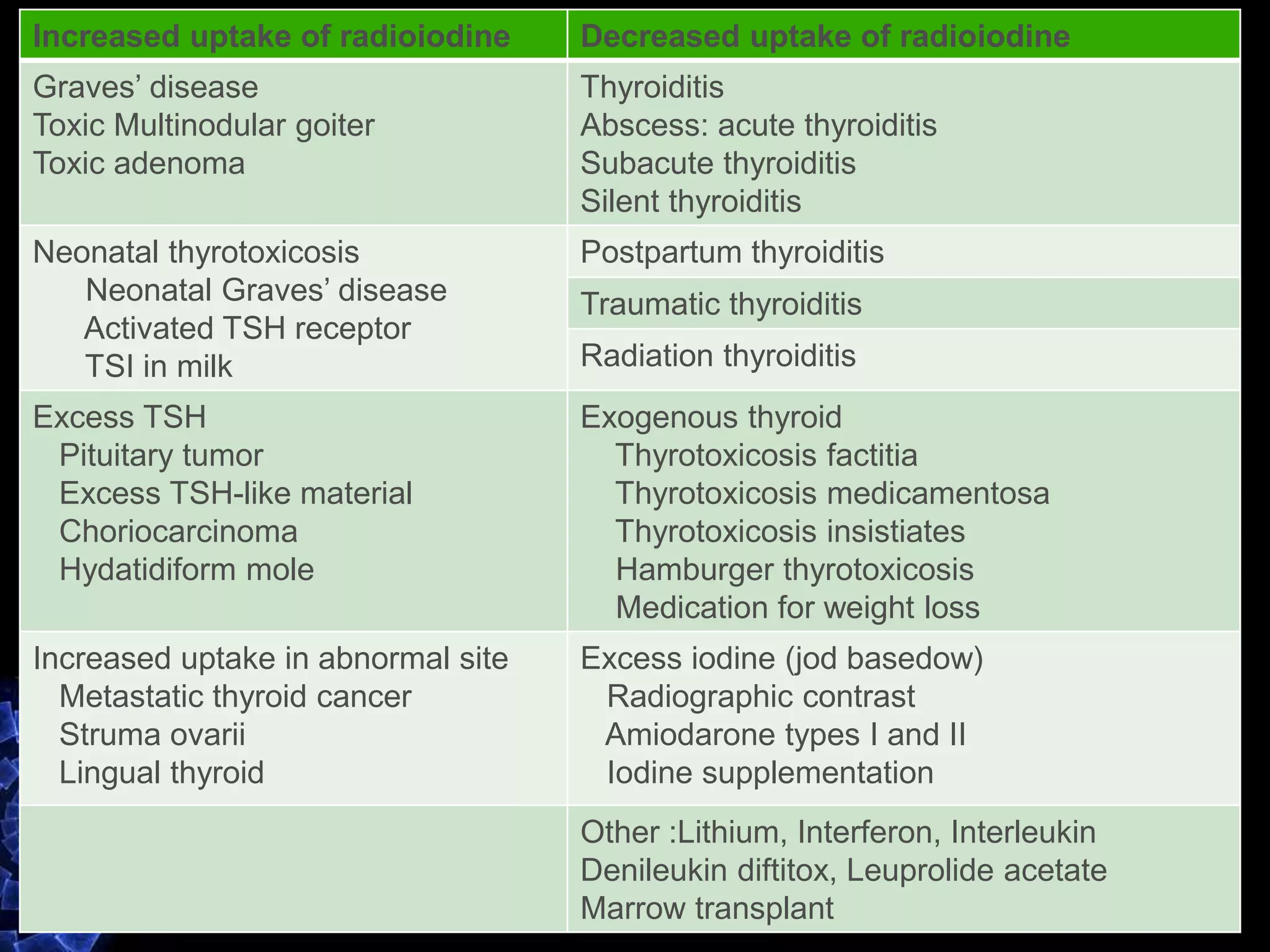
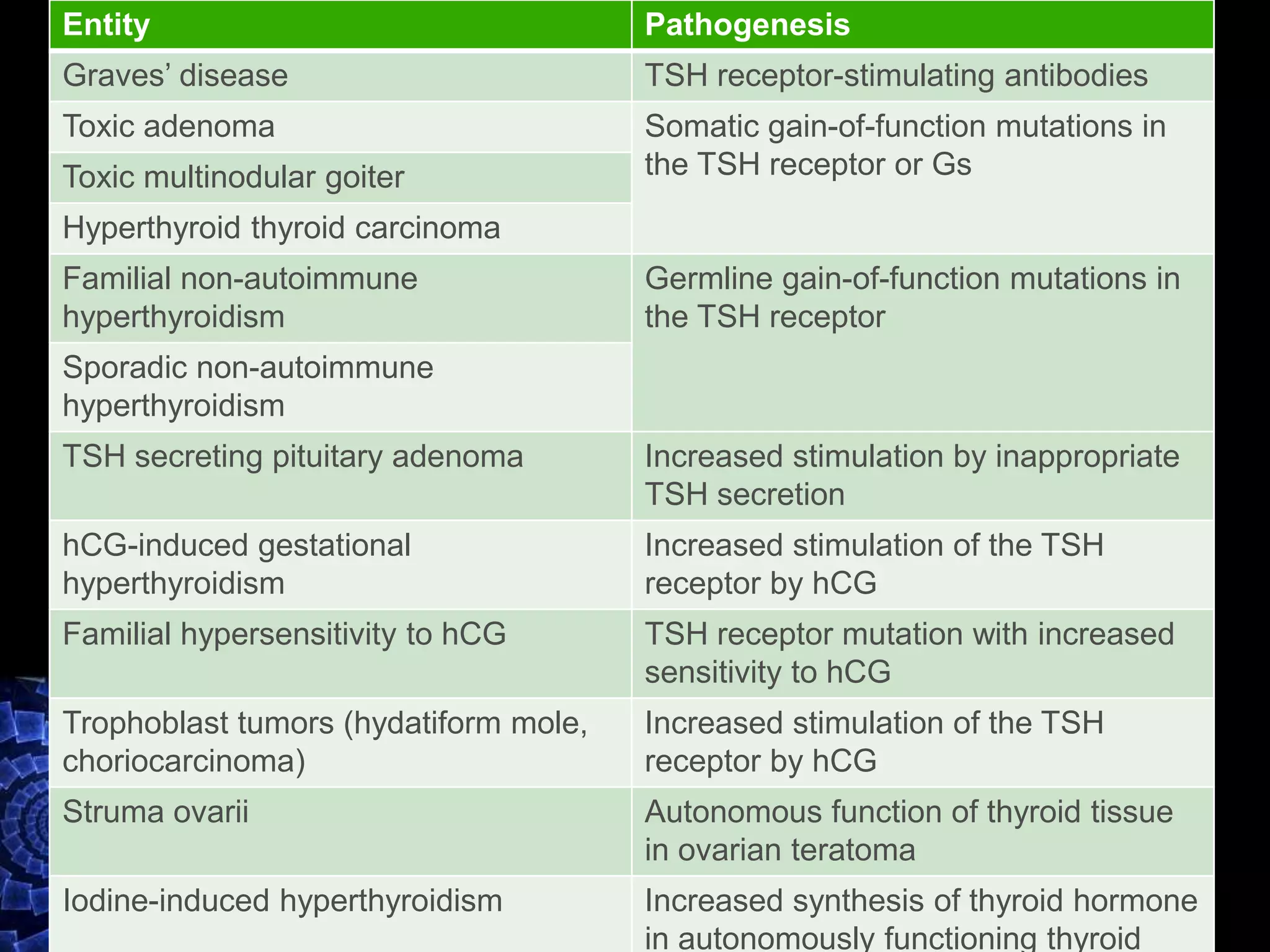
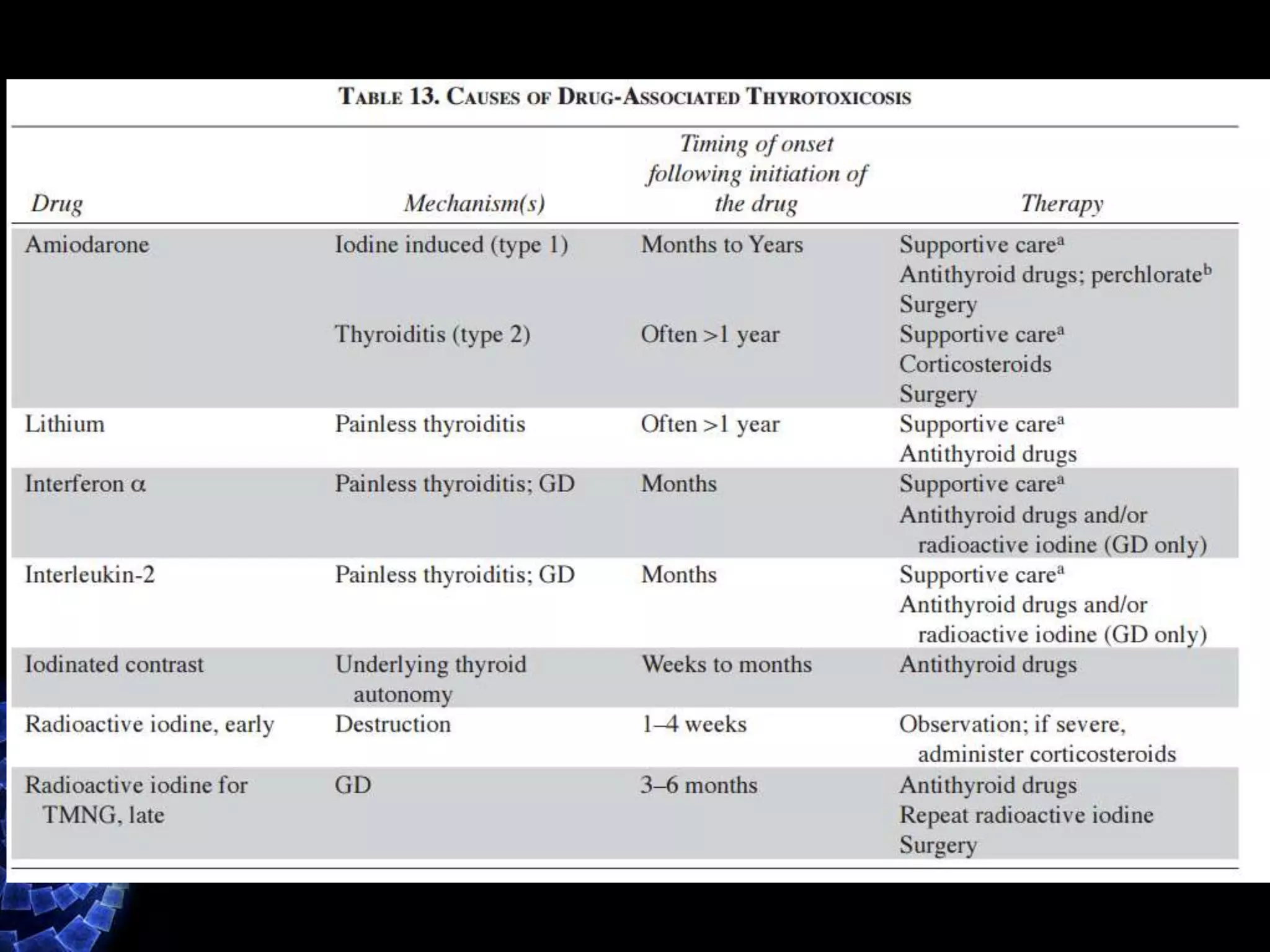
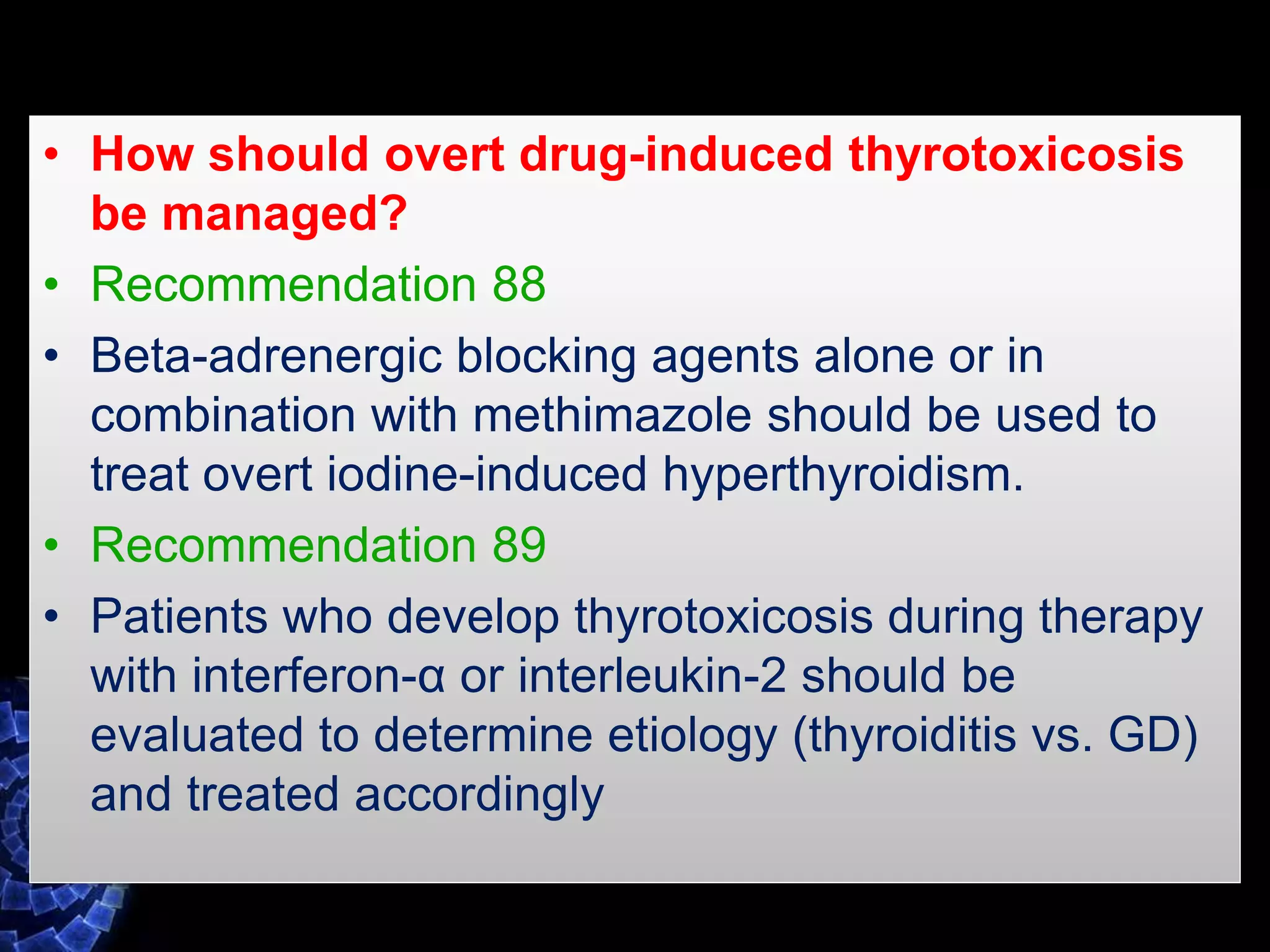
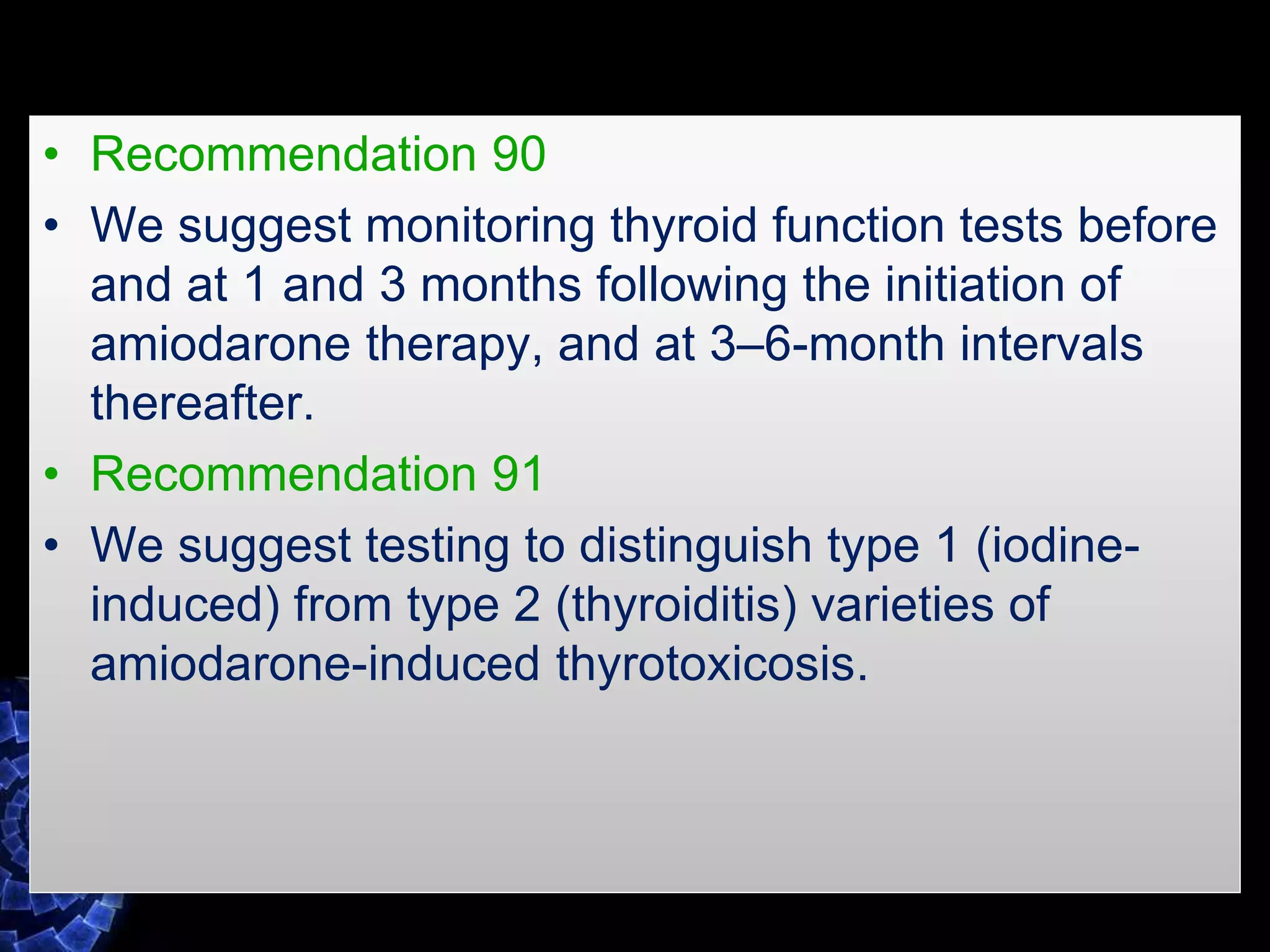
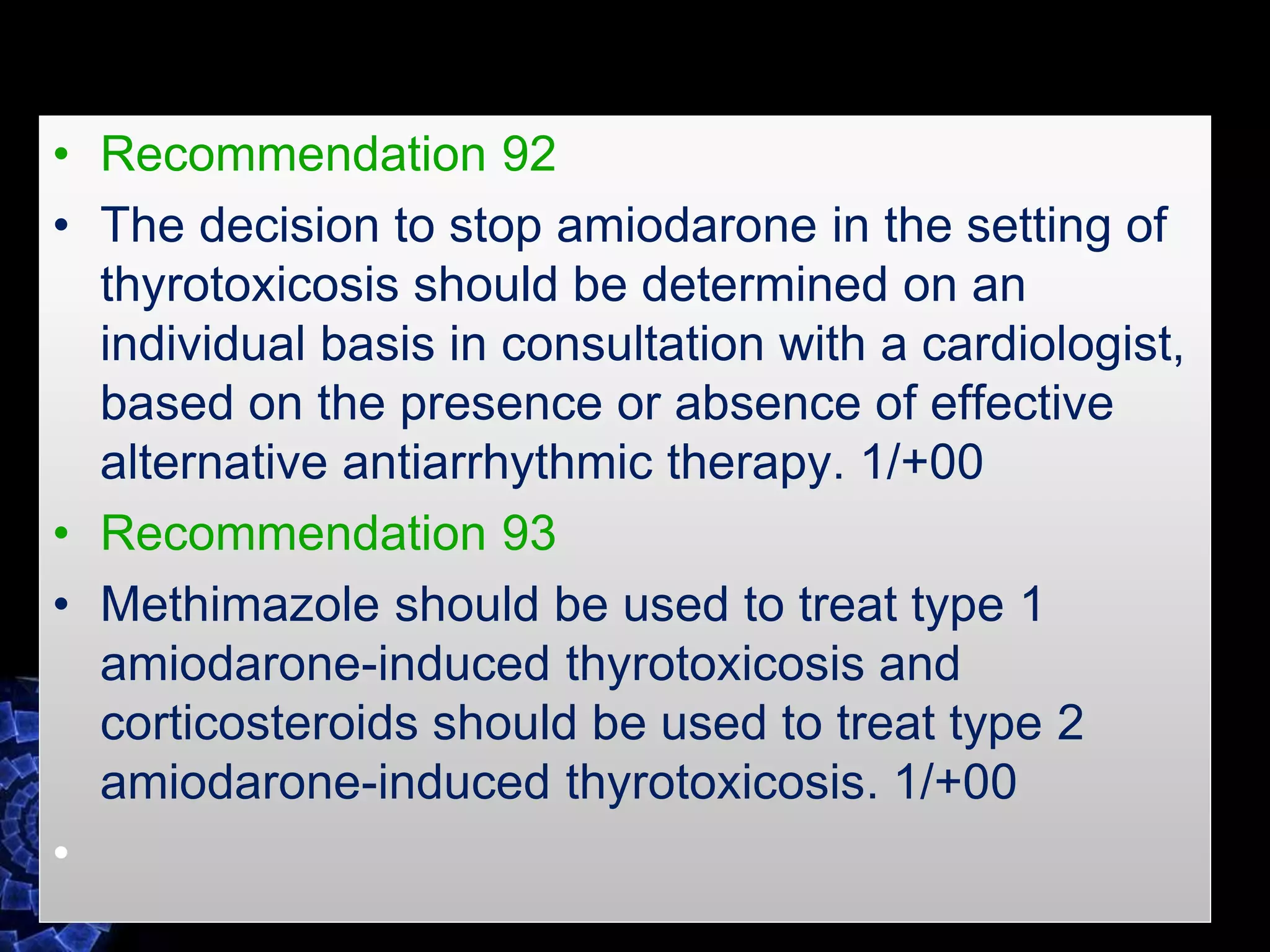
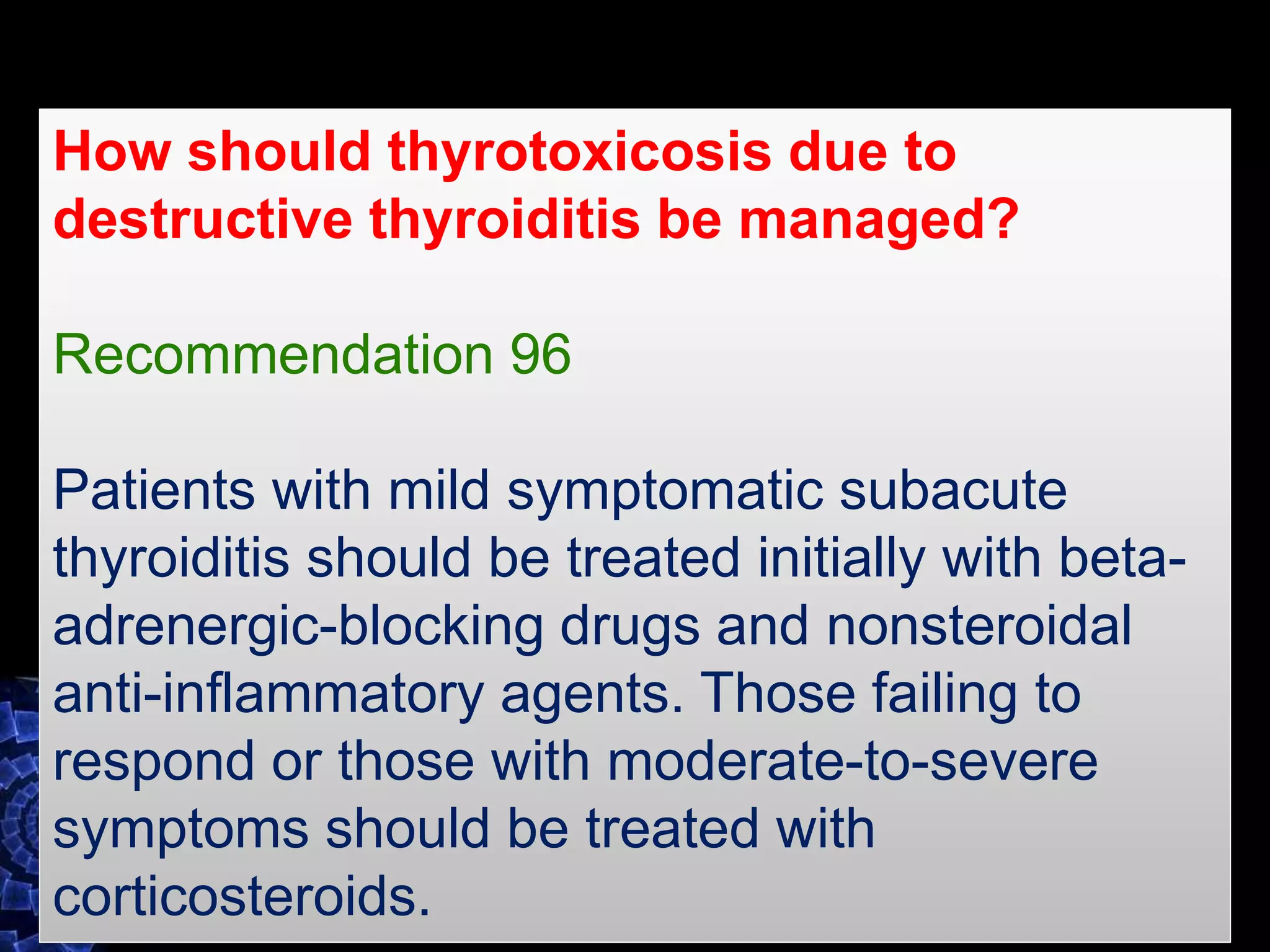
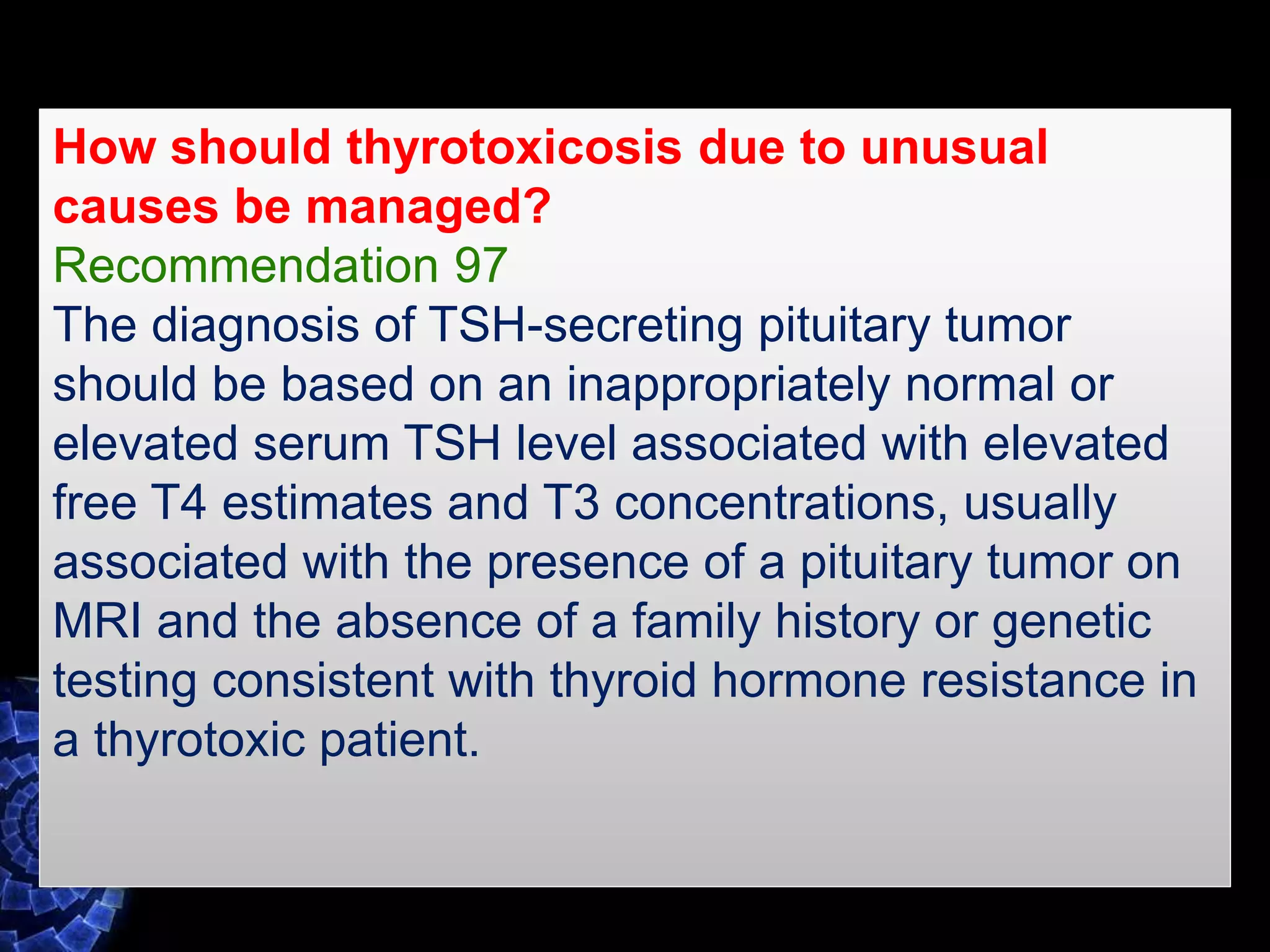
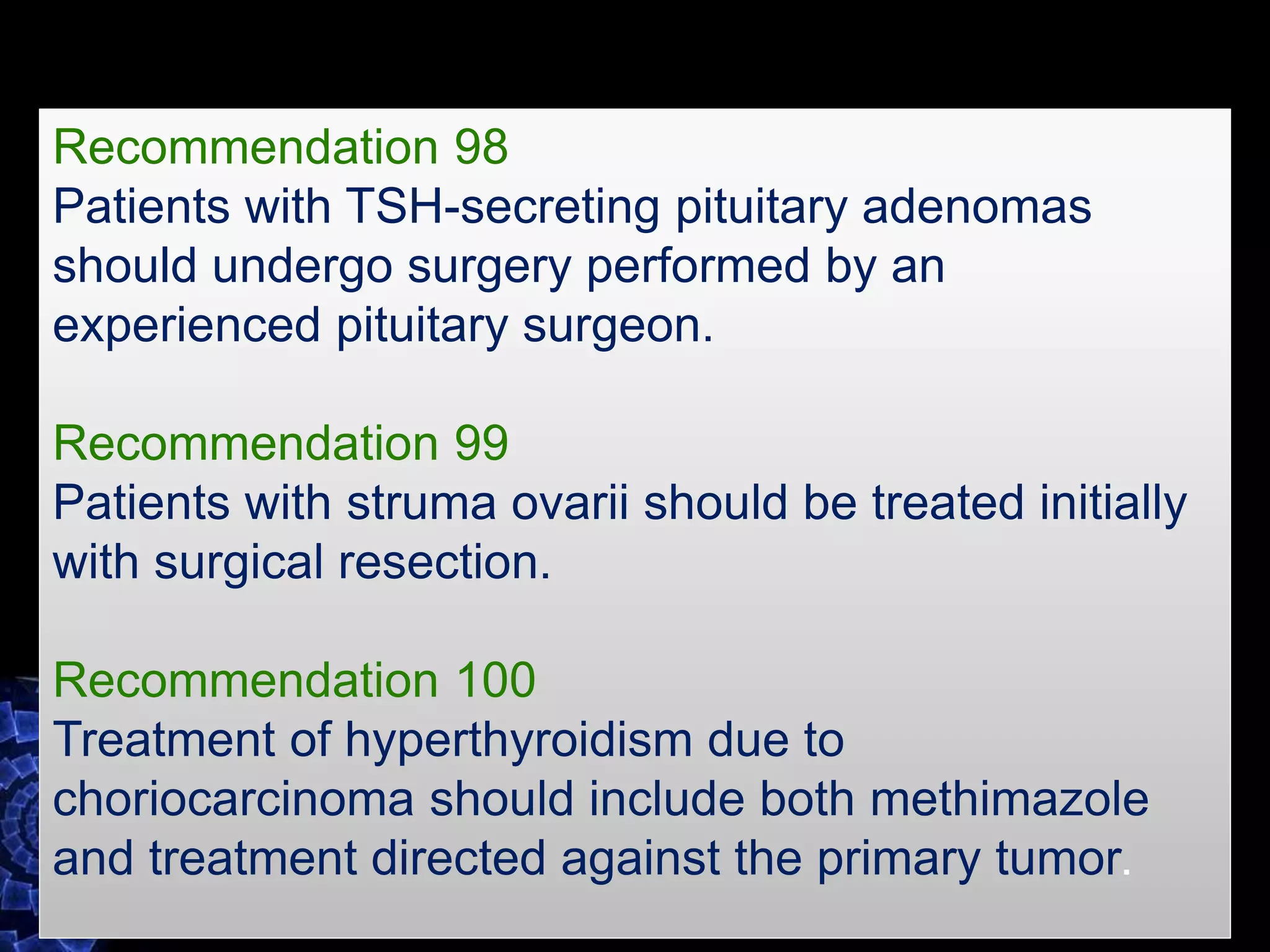
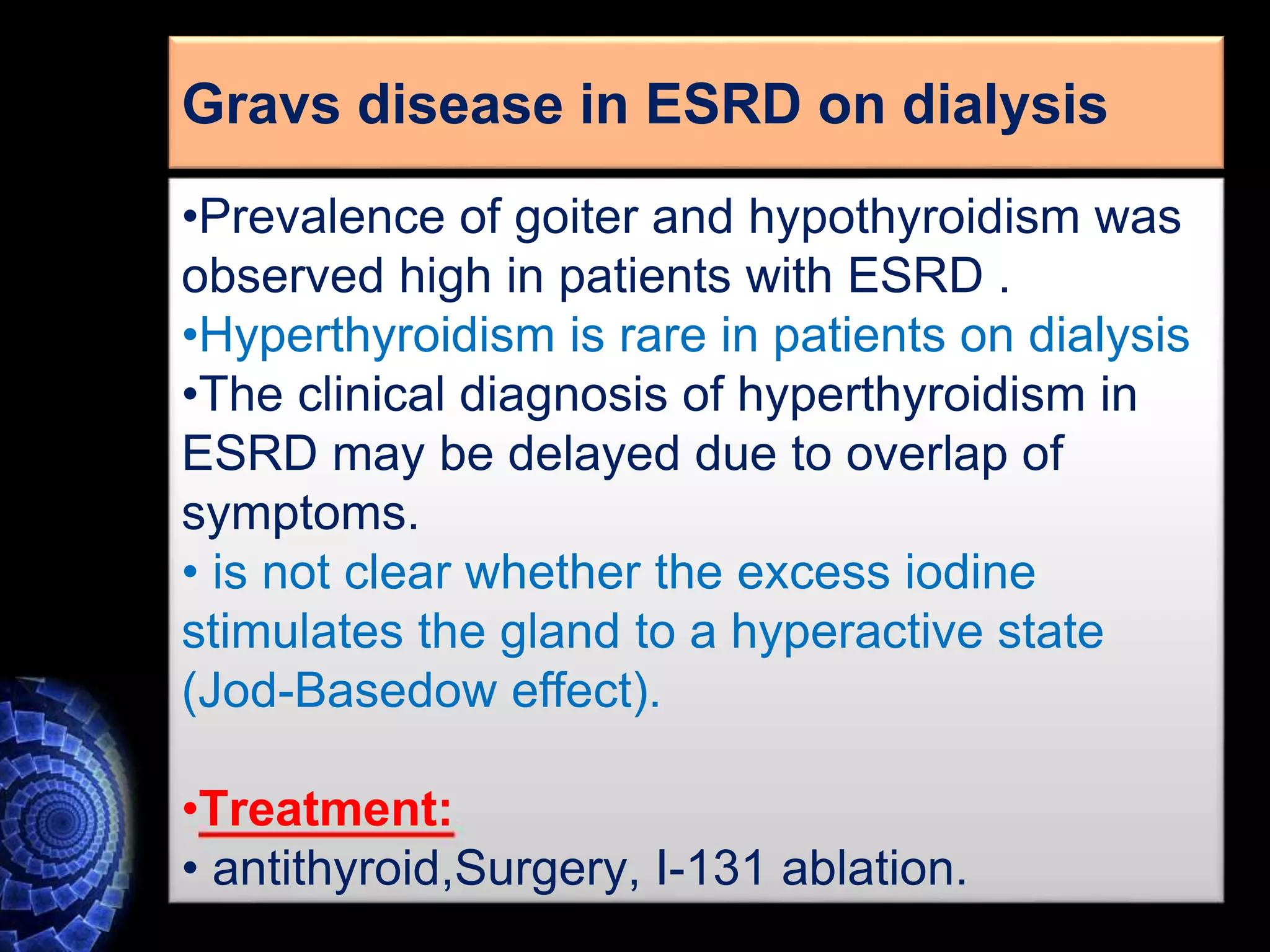
The document describes several cases of thyrotoxicosis and discusses potential causes. It outlines cases of three patients, two children and one infant, who presented with thyrotoxicosis. The potential causes discussed include Graves' disease, toxic multinodular goiter, toxic adenoma, neonatal Graves' disease, activated TSH receptor, excess TSH, thyroiditis, and thyrotoxicosis resulting from excess iodine or medications like amiodarone.