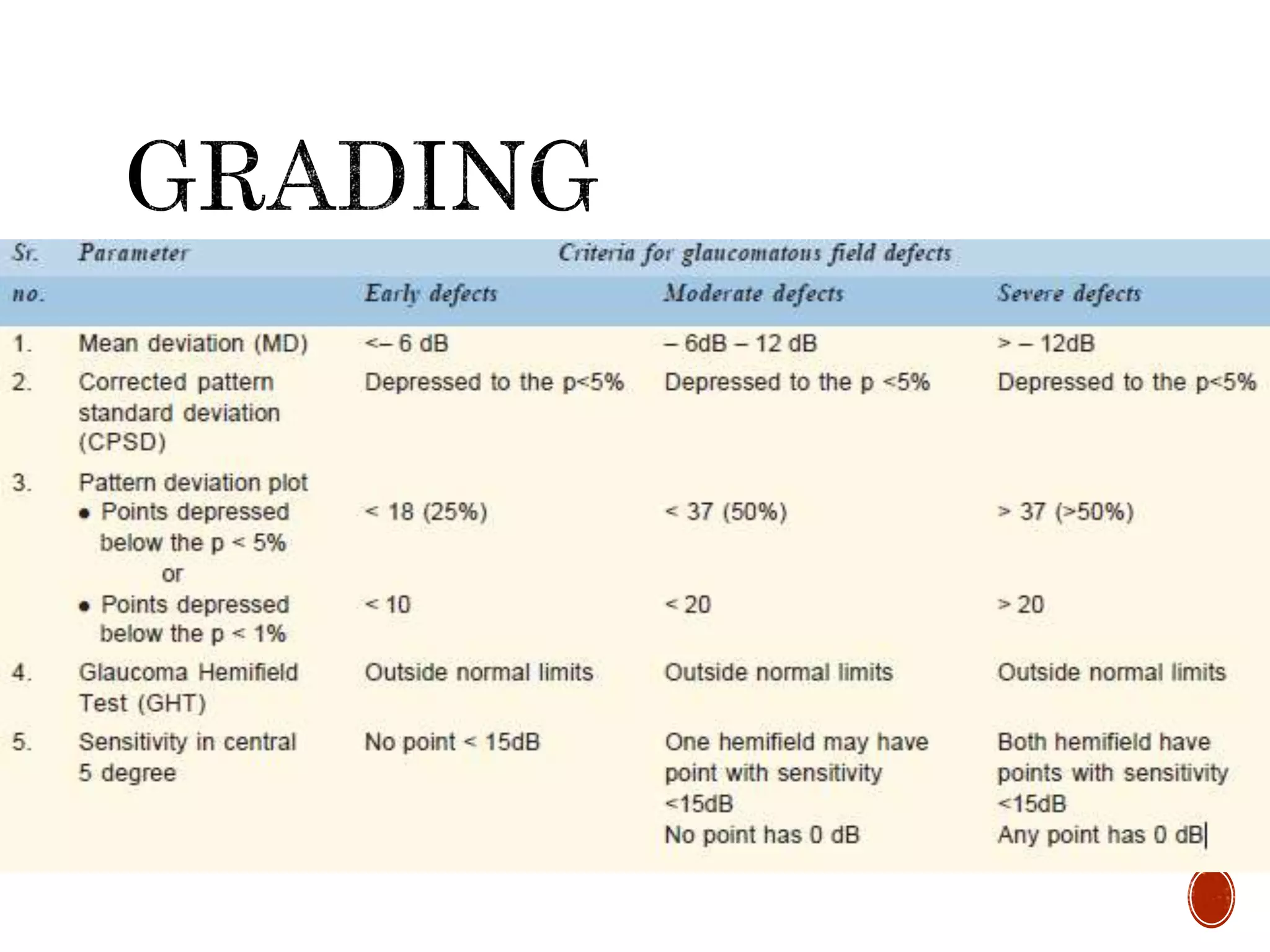
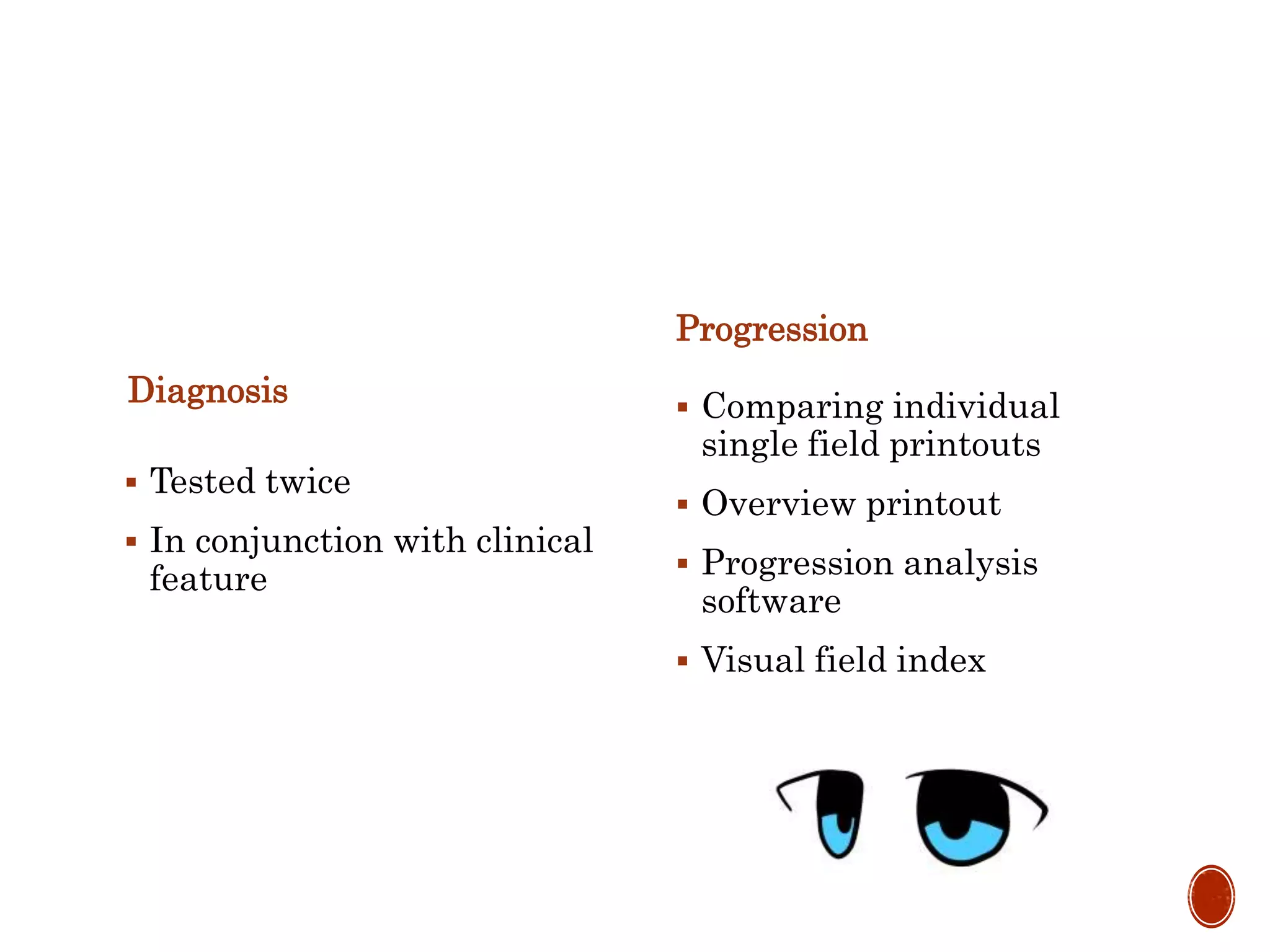
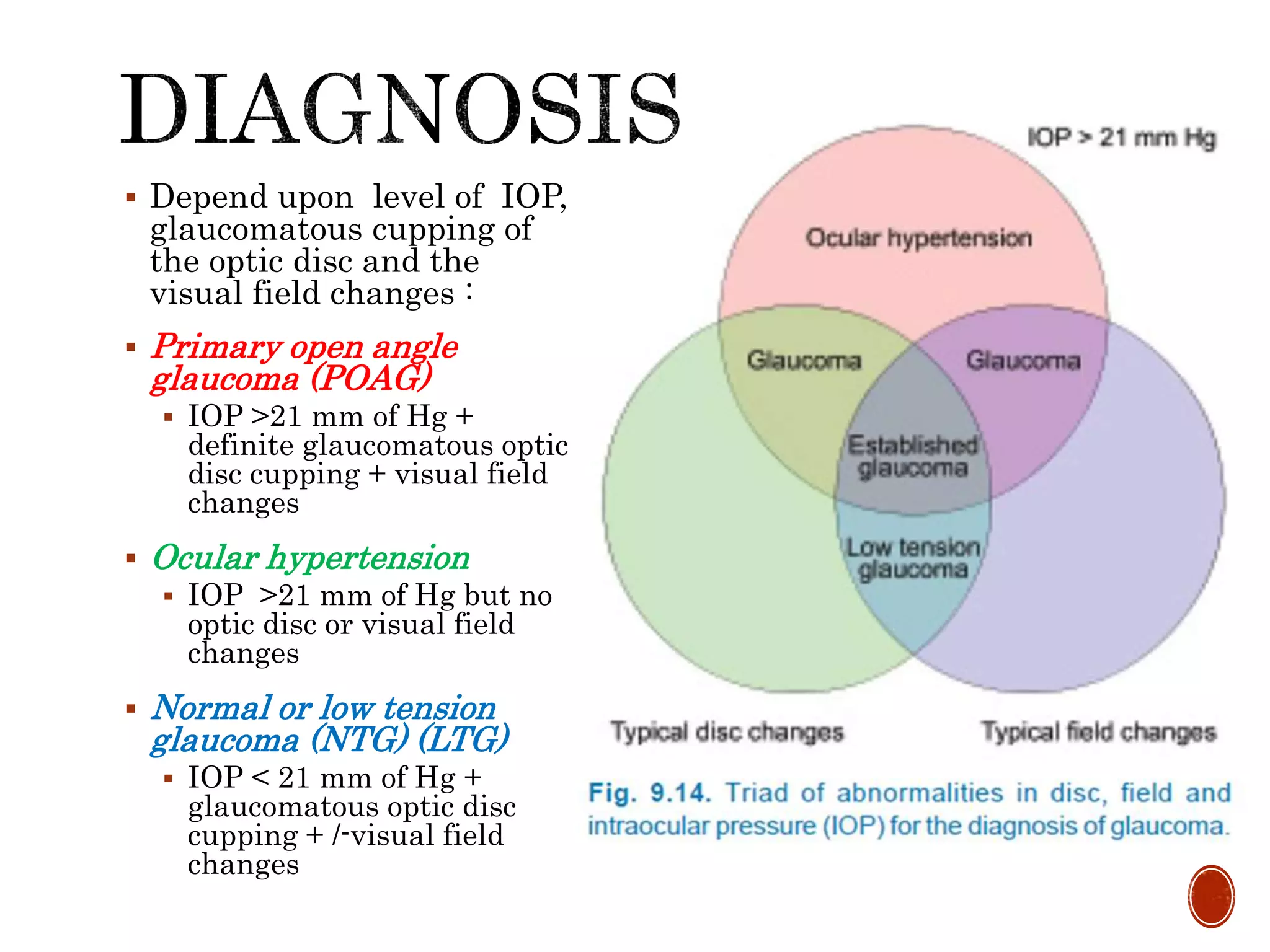
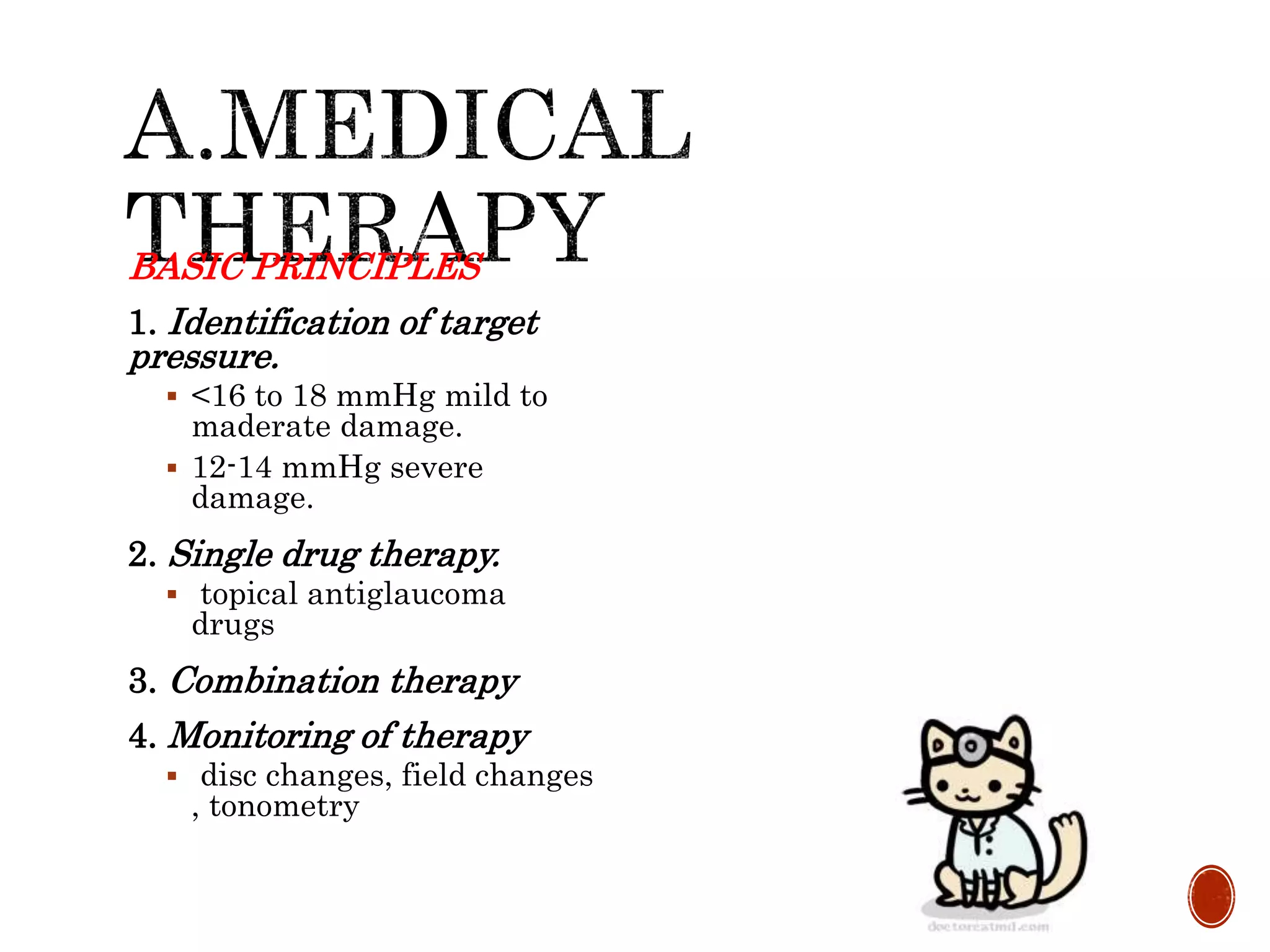
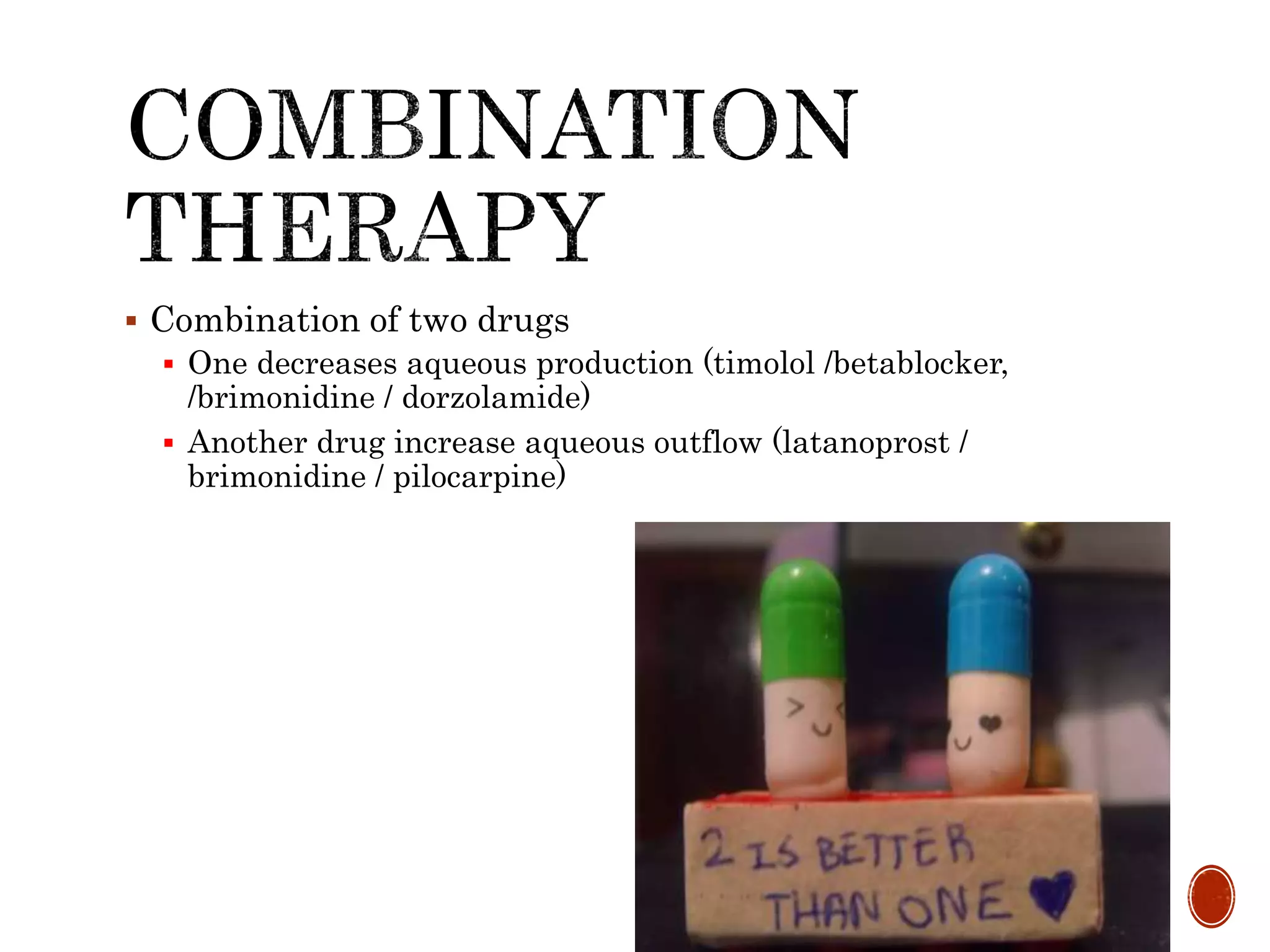
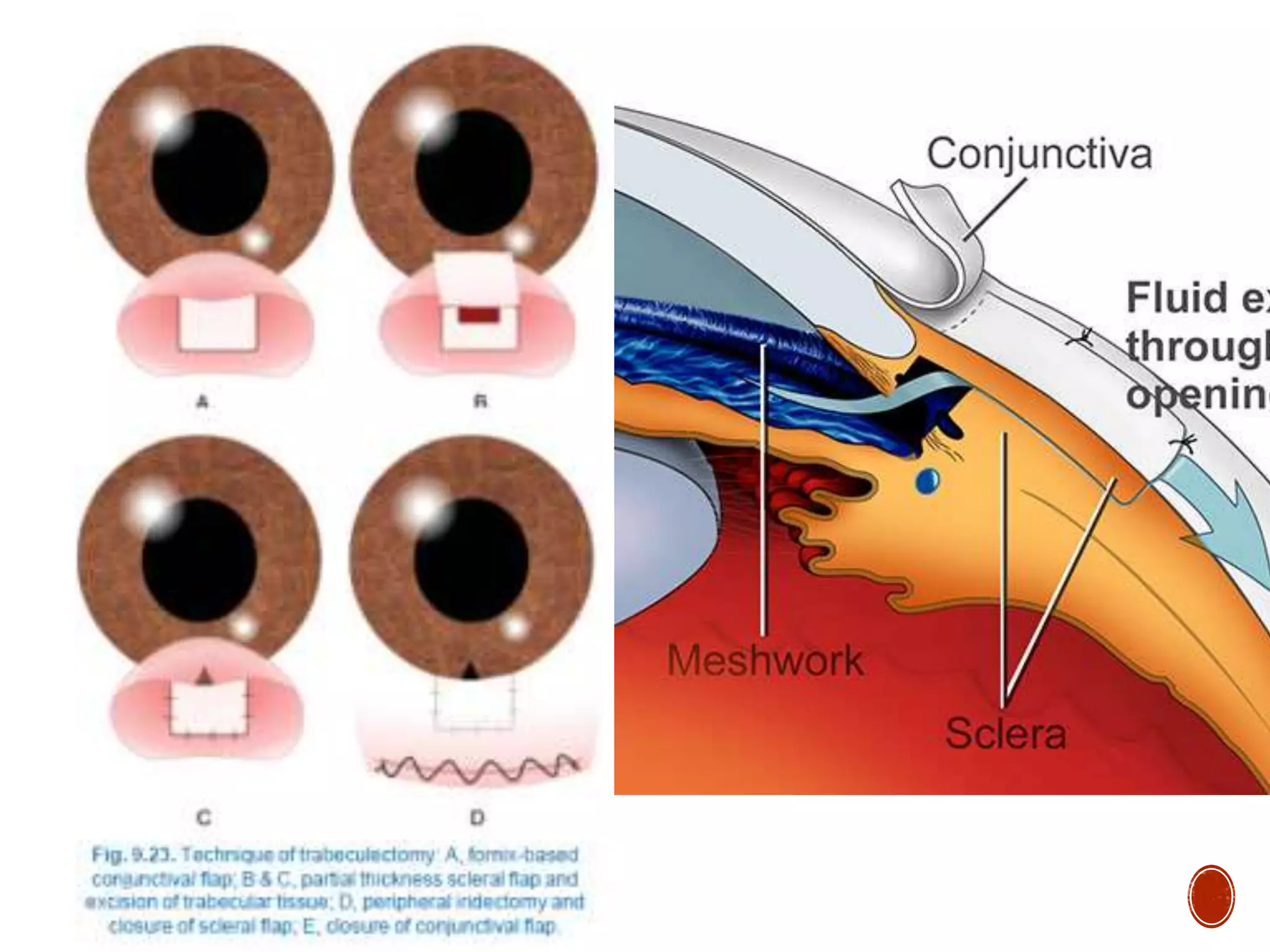
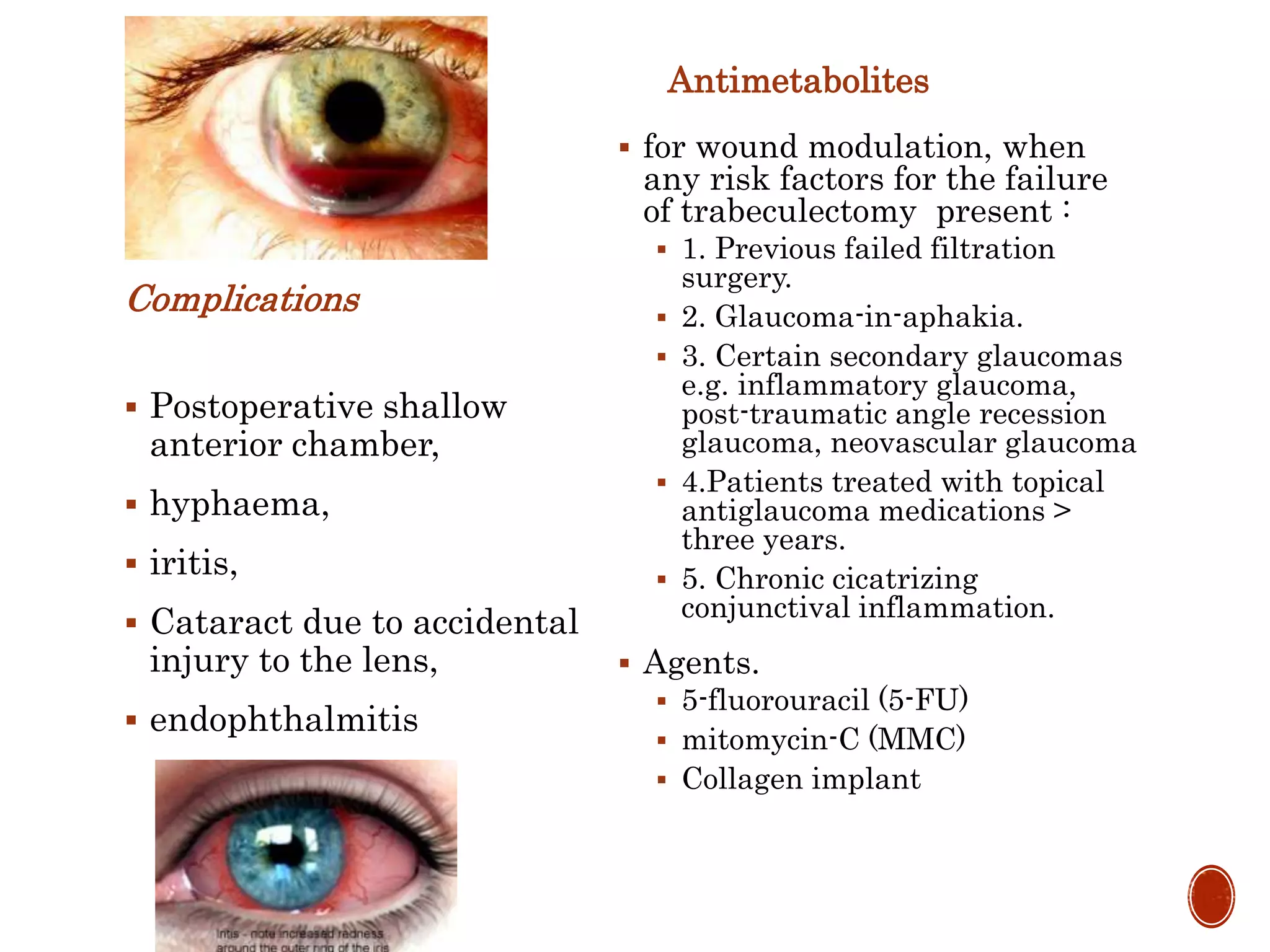
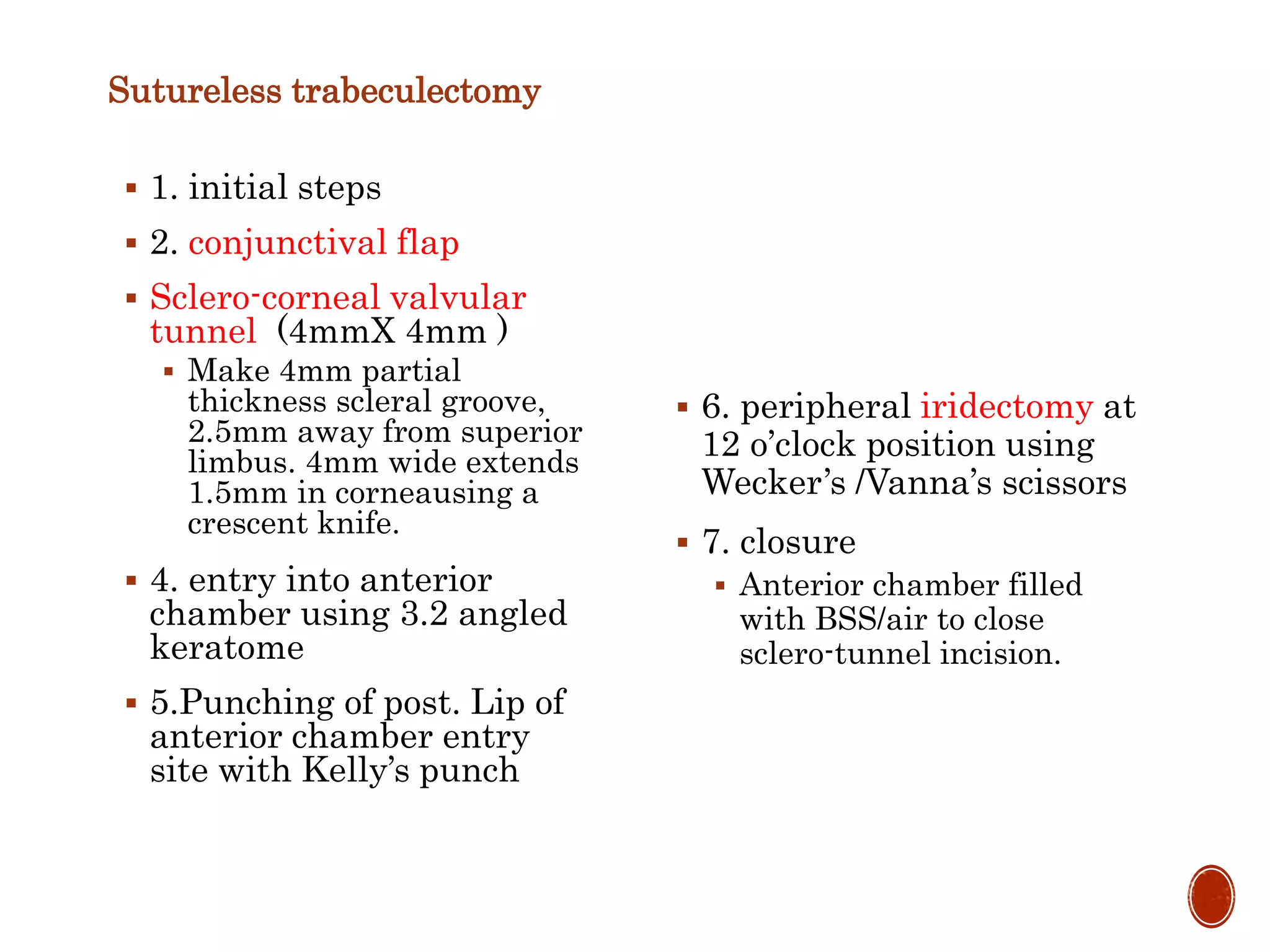
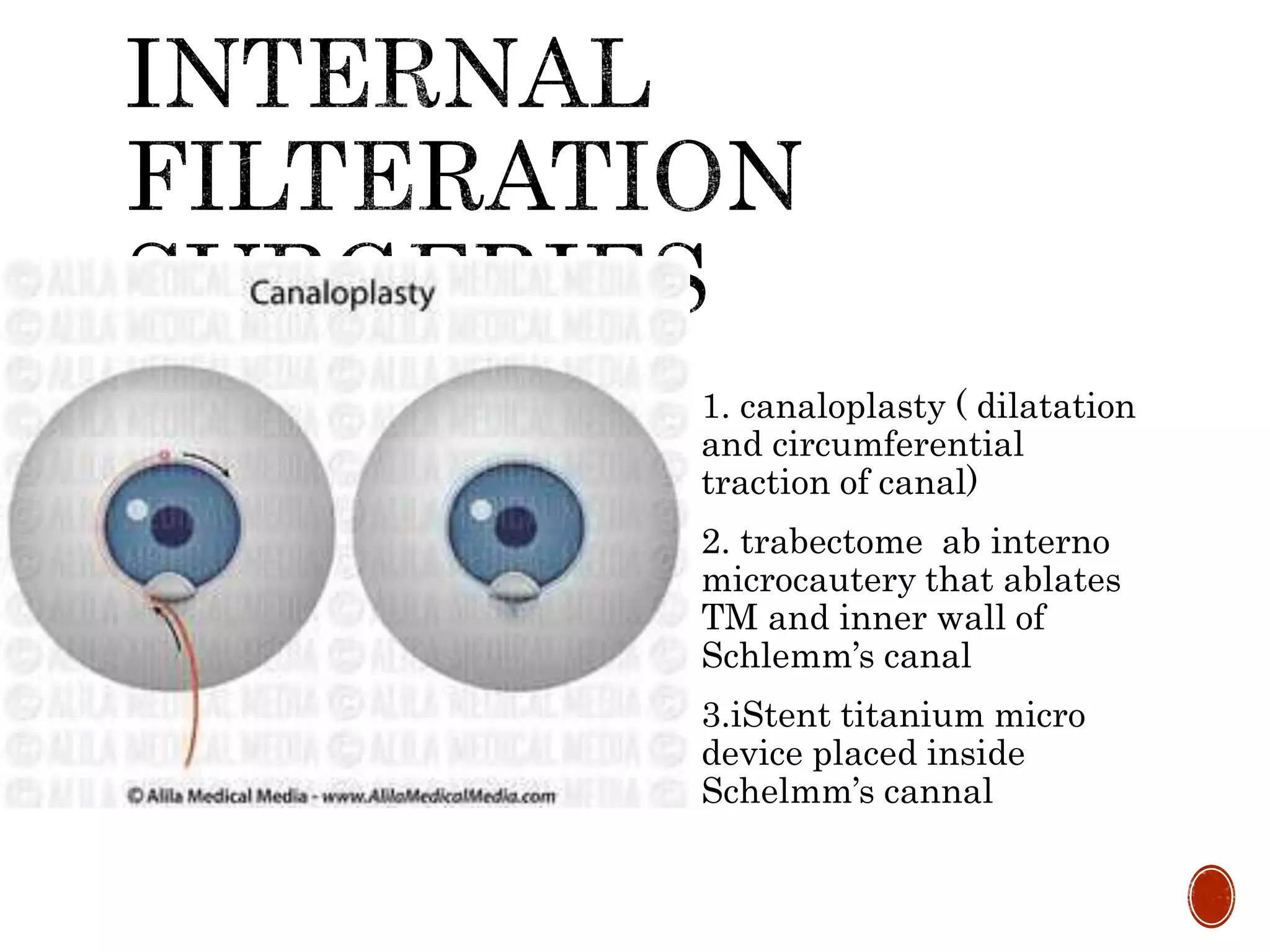
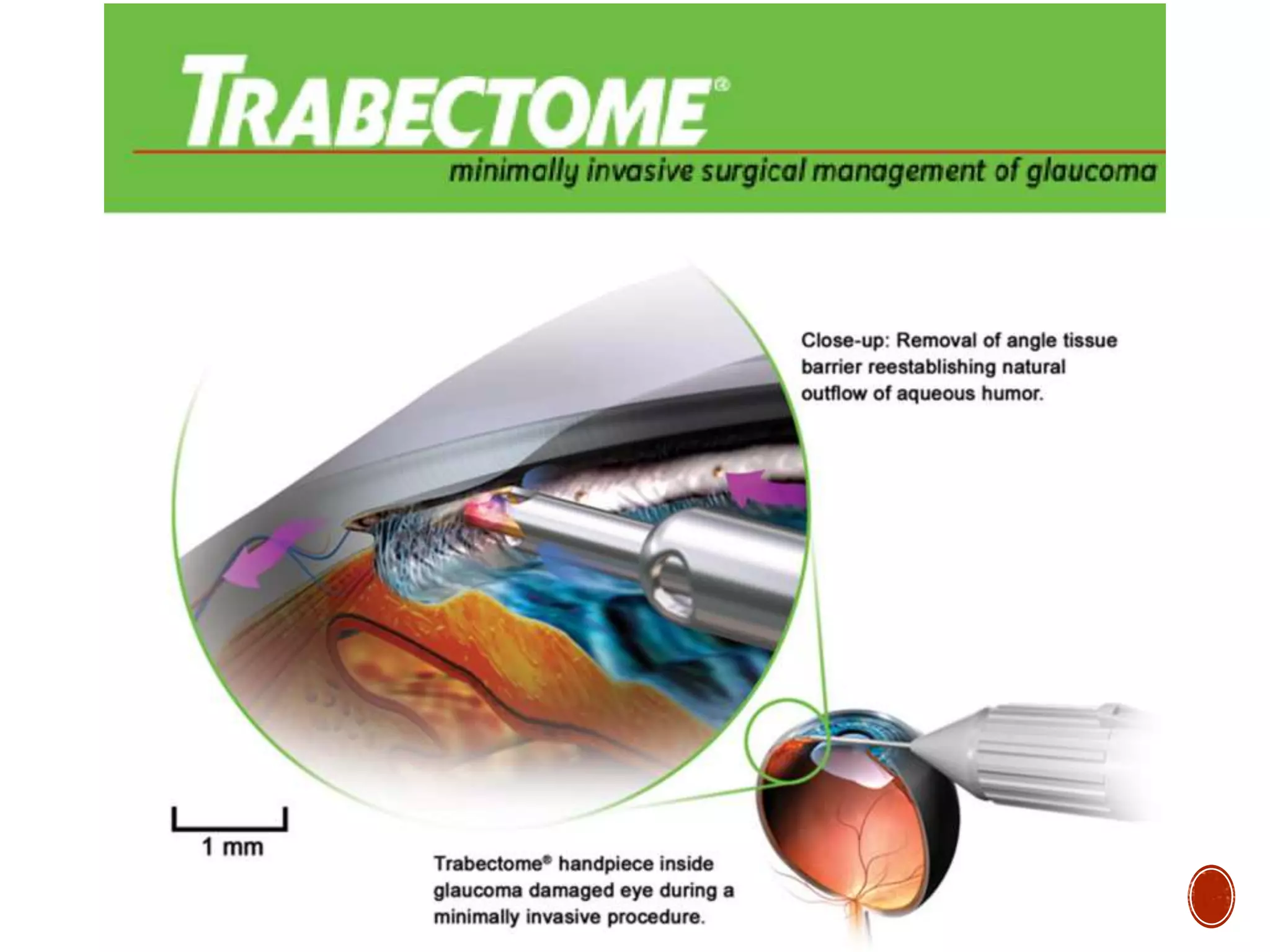
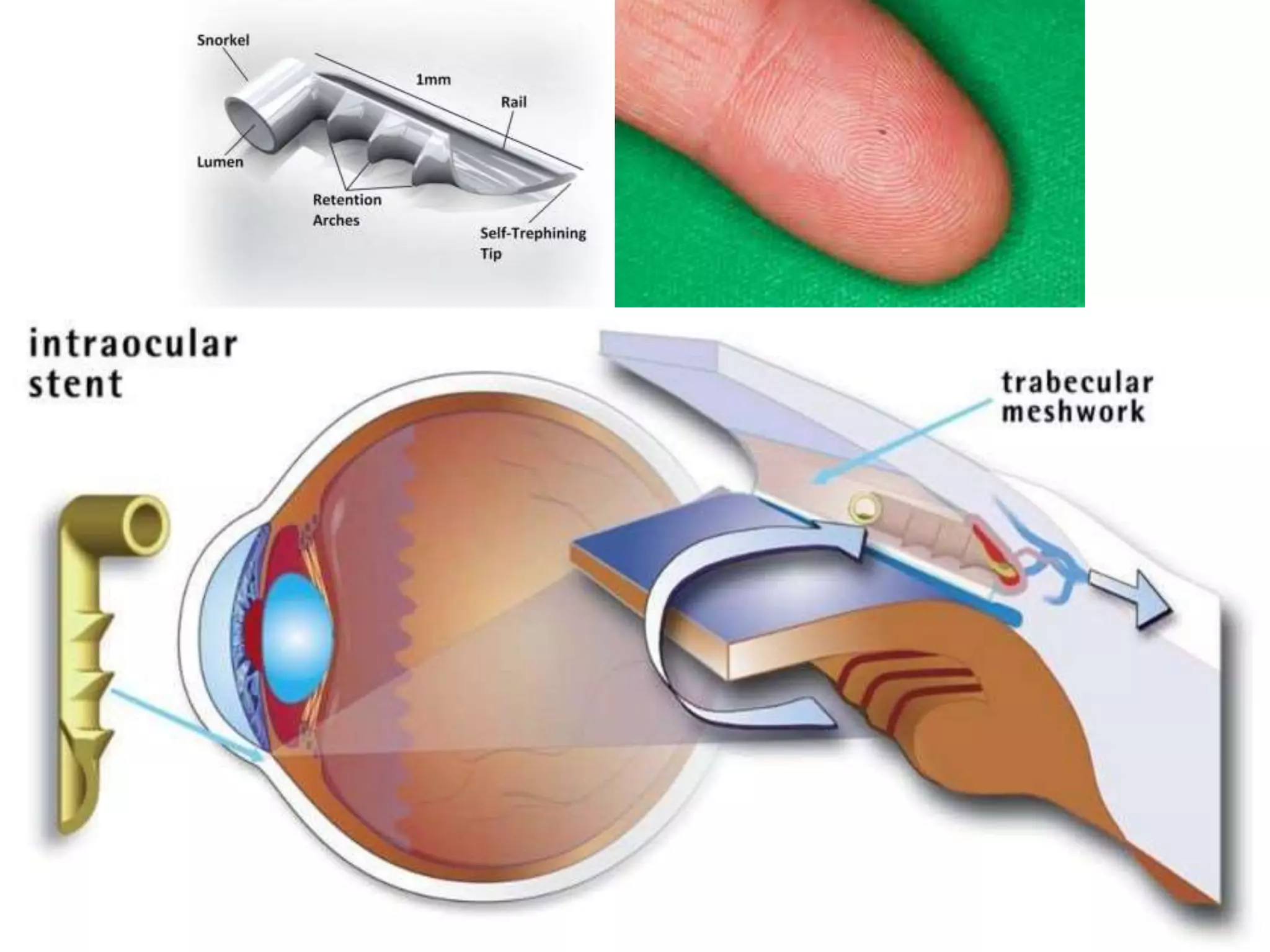
The document provides a comprehensive overview of glaucoma, including its types, symptoms, risk factors, and treatment options. It discusses primary and secondary glaucomas, their pathophysiology, diagnosis methods, and management strategies such as medical therapy, laser treatment, and surgery. Key facts include global prevalence rates, mechanisms of optic nerve damage, and specific treatment protocols involving various classes of medications and surgical techniques.

![A. CONGENITAL/
DEVELOPMENTAL
Primary congenital
glaucoma
Developmental glaucoma
B. PRIMARY ADULT
GLAUCOMA
Primary open angle
glaucoma [POAG]
Primary angle closure
glaucoma [PACG]
Primary mixed mechanism
glaucoma
C. SECONDARY
GLAUCOMA](https://image.slidesharecdn.com/mellss-yr4-opthalmology-glaucoma-primary-open-angle-160219174213/75/Mellss-yr4-opthalmology-glaucoma-primary-open-angle-6-2048.jpg)
![ GLAUCOMATOUS OCULAR DAMAGE
progressive optic neuropathy due to death of retinal
ganglion cells (RGCs) optic disc appearance and
specific visual field defects
RETINAL GANGLION CELL (RGC) DEATH
blocks the transport of growth factors (neurotrophins)
from the brain to the RGCs.
apoptosis engulfed by neighbouring cells, without
[inflammatory response]
loss of retinal nerve fibres. optic disc changes and
specific visual field defects](https://image.slidesharecdn.com/mellss-yr4-opthalmology-glaucoma-primary-open-angle-160219174213/75/Mellss-yr4-opthalmology-glaucoma-primary-open-angle-9-2048.jpg)
![A. Primary insults
Raised intraocular pressure [ mechanical theory]
Pressure independent factors [ vascular insufficiency
theory]
Failure of autoregulatory mechanism of blood flow
Vasospasm
Systemic hypotension
Other factors: acute blood loss, abnormal coagulation
B. Secondary insults [ excitotoxicity theory]
Glutamate, nitric oxide, oxygen- free radicals](https://image.slidesharecdn.com/mellss-yr4-opthalmology-glaucoma-primary-open-angle-160219174213/75/Mellss-yr4-opthalmology-glaucoma-primary-open-angle-10-2048.jpg)
![ Aka chronic simple glaucoma of adult onset
Characterised by:
Slowly progressive raised IOP [ >21mmHg on few occasions]
Open normal appearing anterior angle chamber
Optic disc cupping
Specific visual field defects](https://image.slidesharecdn.com/mellss-yr4-opthalmology-glaucoma-primary-open-angle-160219174213/75/Mellss-yr4-opthalmology-glaucoma-primary-open-angle-12-2048.jpg)
![ Not known exactly
PREDISPOSING AND
RISK FACTORS
Intraocular pressure
Hereditary [ Myocilin C ,
Optineurin, WD repeat
domain 36]
Age
Race
Myopes
Central corneal thickness
Diabetics
High blood pressure
Smoking
Thyrotoxicosis
Corticosteroid
responsiveness](https://image.slidesharecdn.com/mellss-yr4-opthalmology-glaucoma-primary-open-angle-160219174213/75/Mellss-yr4-opthalmology-glaucoma-primary-open-angle-13-2048.jpg)
![ Asymptomatic
Mild headache and eye ache
Scotoma [ defect in visual
field]
Increasing difficulty in
reading and close work
Delayed dark adaptation
Significant loss of vision ,
blindness](https://image.slidesharecdn.com/mellss-yr4-opthalmology-glaucoma-primary-open-angle-160219174213/75/Mellss-yr4-opthalmology-glaucoma-primary-open-angle-17-2048.jpg)
![ Slit lamp biomicroscopy : normal anterior segment
Sluggish pupil reflex
Slight hazy cornea
Low [ <555µm] CCT](https://image.slidesharecdn.com/mellss-yr4-opthalmology-glaucoma-primary-open-angle-160219174213/75/Mellss-yr4-opthalmology-glaucoma-primary-open-angle-19-2048.jpg)
![Initial:
Diurnal variation test [ 3-4 h/24h]
fall on evening
5mmHg : suspicious
>8mmHg : glaucoma
Later :
Permanent rise
30-45mmHg](https://image.slidesharecdn.com/mellss-yr4-opthalmology-glaucoma-primary-open-angle-160219174213/75/Mellss-yr4-opthalmology-glaucoma-primary-open-angle-20-2048.jpg)
![ Best examination technique:
stereoscopic view with contact or non-contact lens on slit lamp
biomicroscopic examination
Recording and documentation :
serial hand drawings, photography, photogrammetry, confocal
scanning laser topography [ CSLT], Heidelberg retinal
tomography [ HRT],coherence tomography [CT], nerve fibre
analyser [ NFA]](https://image.slidesharecdn.com/mellss-yr4-opthalmology-glaucoma-primary-open-angle-160219174213/75/Mellss-yr4-opthalmology-glaucoma-primary-open-angle-21-2048.jpg)
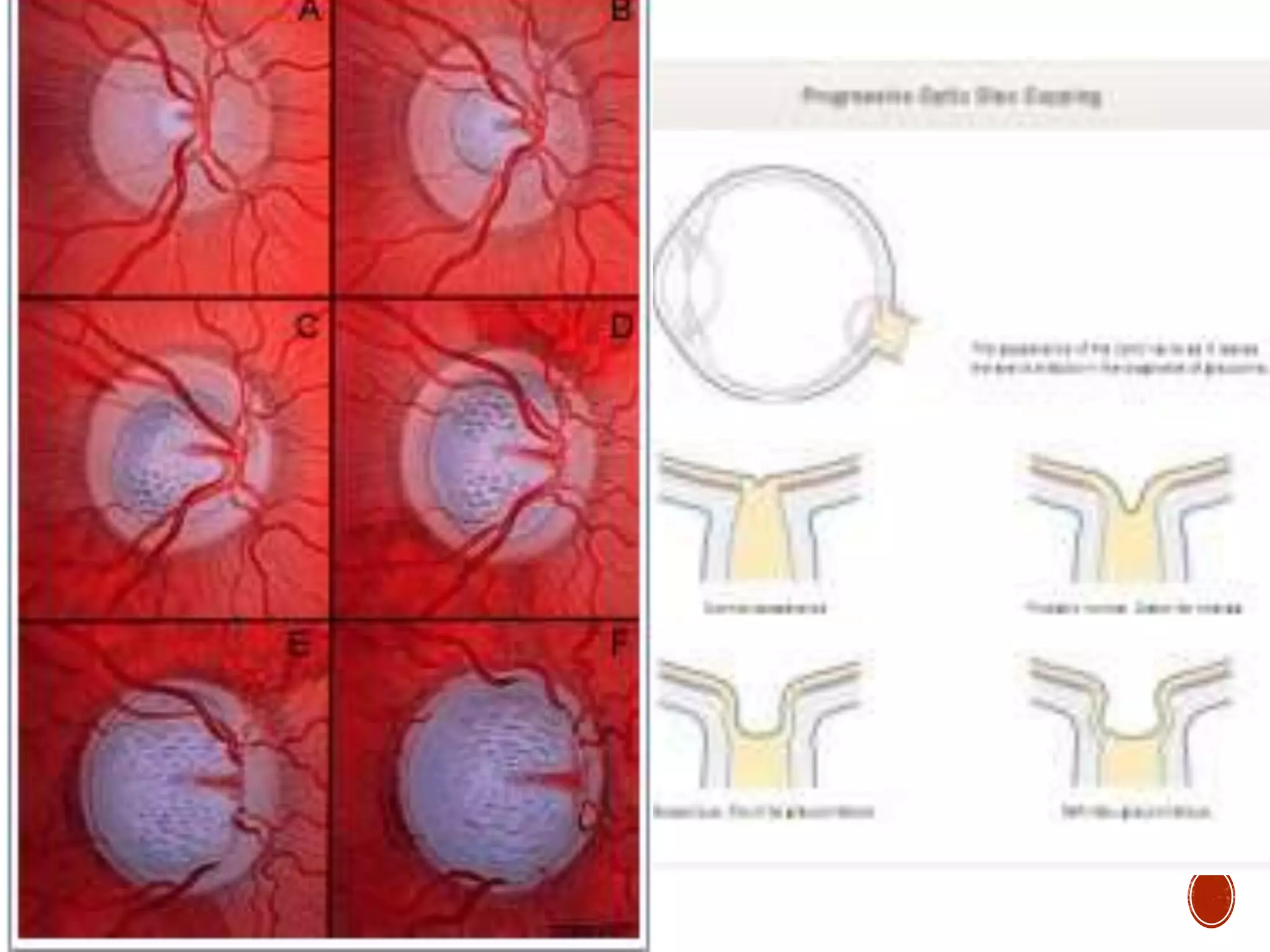
![a. Early changes
Vertically oval cup
Cups symmetry between
eyes [>0.2]
Large cup [ >0.6]
Splinter hemorrhages
Pallor areas on disc
Retinal nerve fibre atrophy
[ red free light]](https://image.slidesharecdn.com/mellss-yr4-opthalmology-glaucoma-primary-open-angle-160219174213/75/Mellss-yr4-opthalmology-glaucoma-primary-open-angle-22-2048.jpg)

![b. Advanced changes
Marked cupping [ 0.7-0.9]
Thinning of neuroretinal rim ( crescentic shadow)
[ISNT rule]
Nasal shift of retinal vessels [ Bayonetting sign]
Retinal arterioles pulsation
Lamellar dot sign](https://image.slidesharecdn.com/mellss-yr4-opthalmology-glaucoma-primary-open-angle-160219174213/75/Mellss-yr4-opthalmology-glaucoma-primary-open-angle-24-2048.jpg)
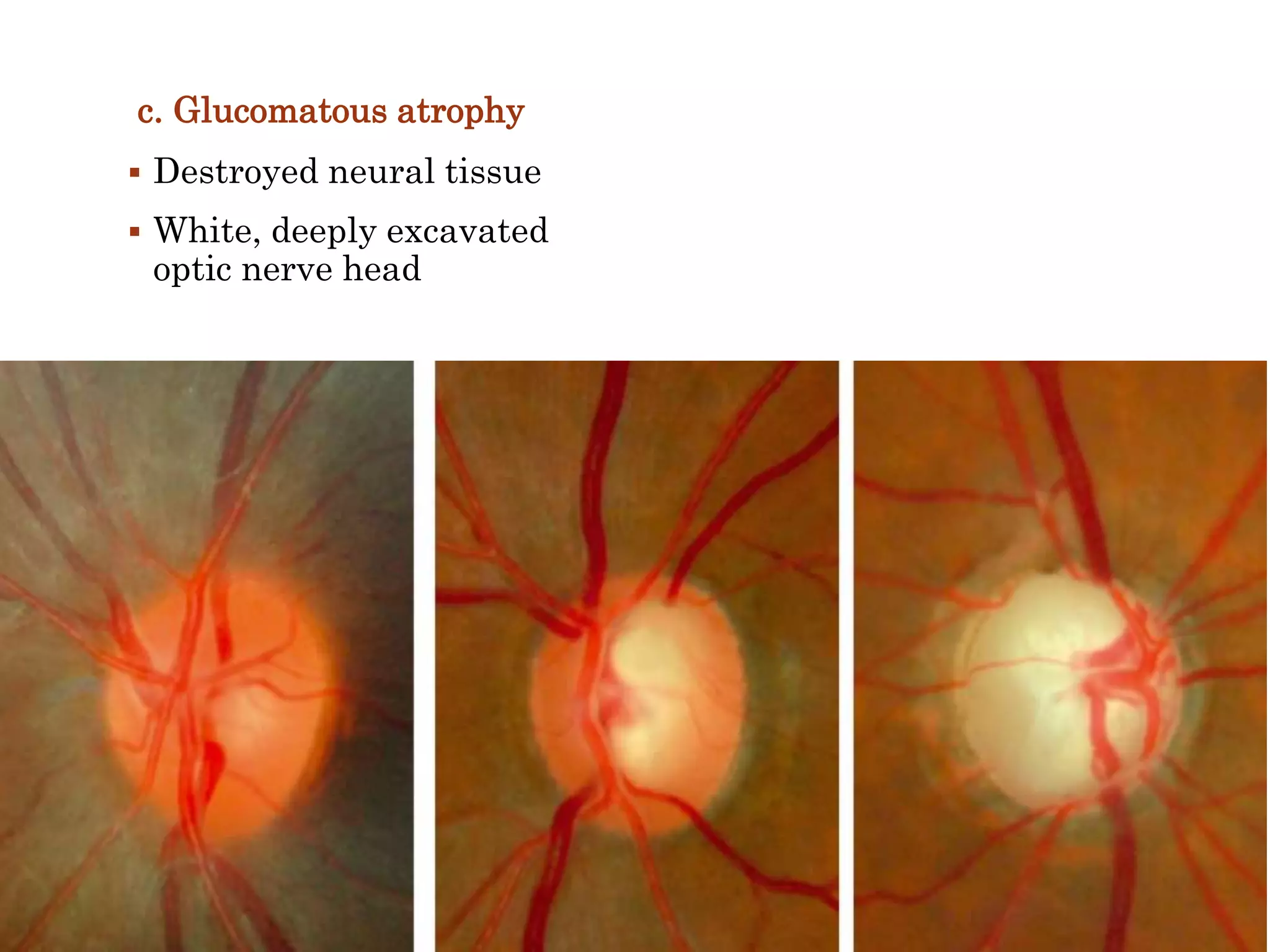
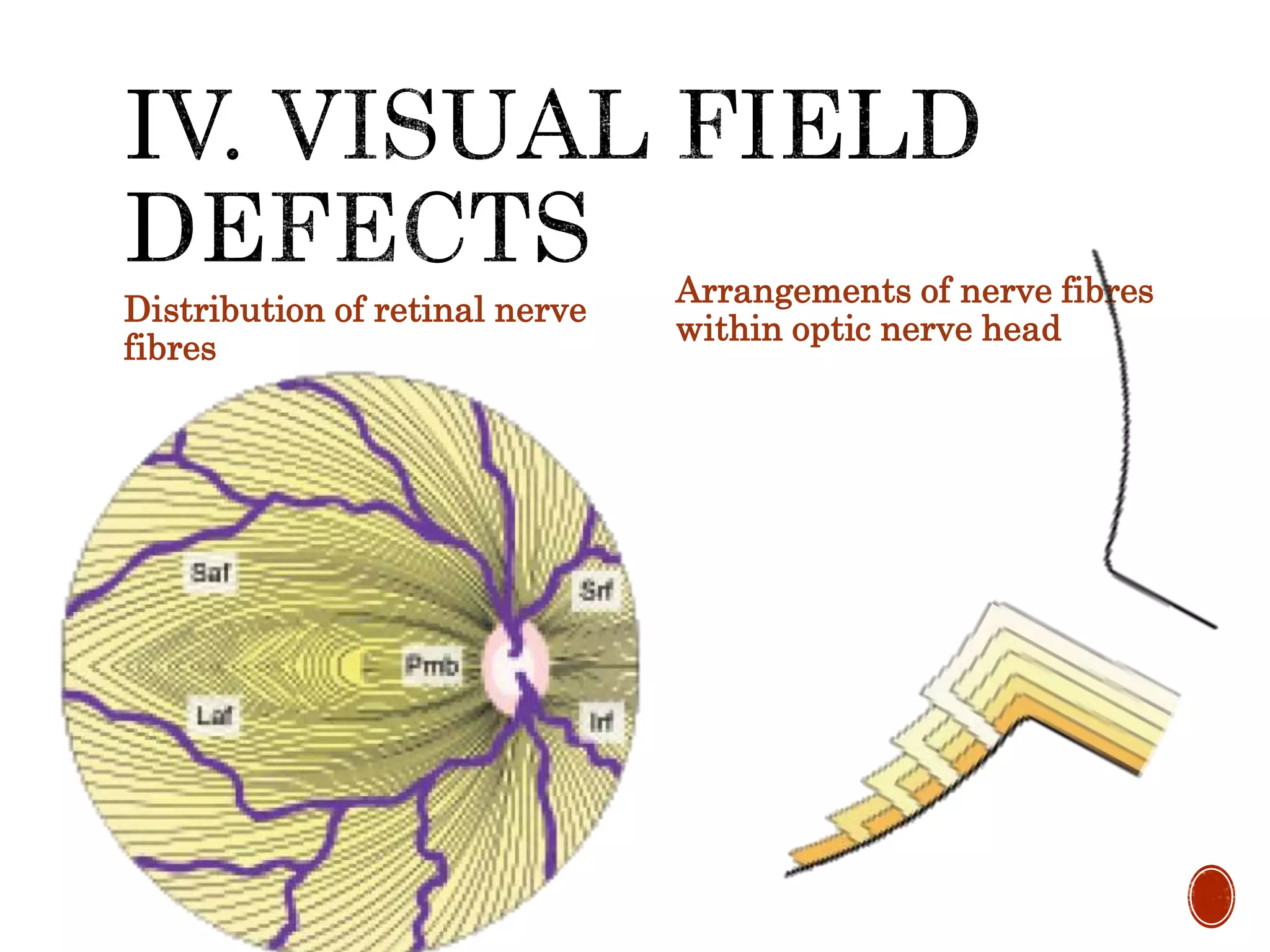
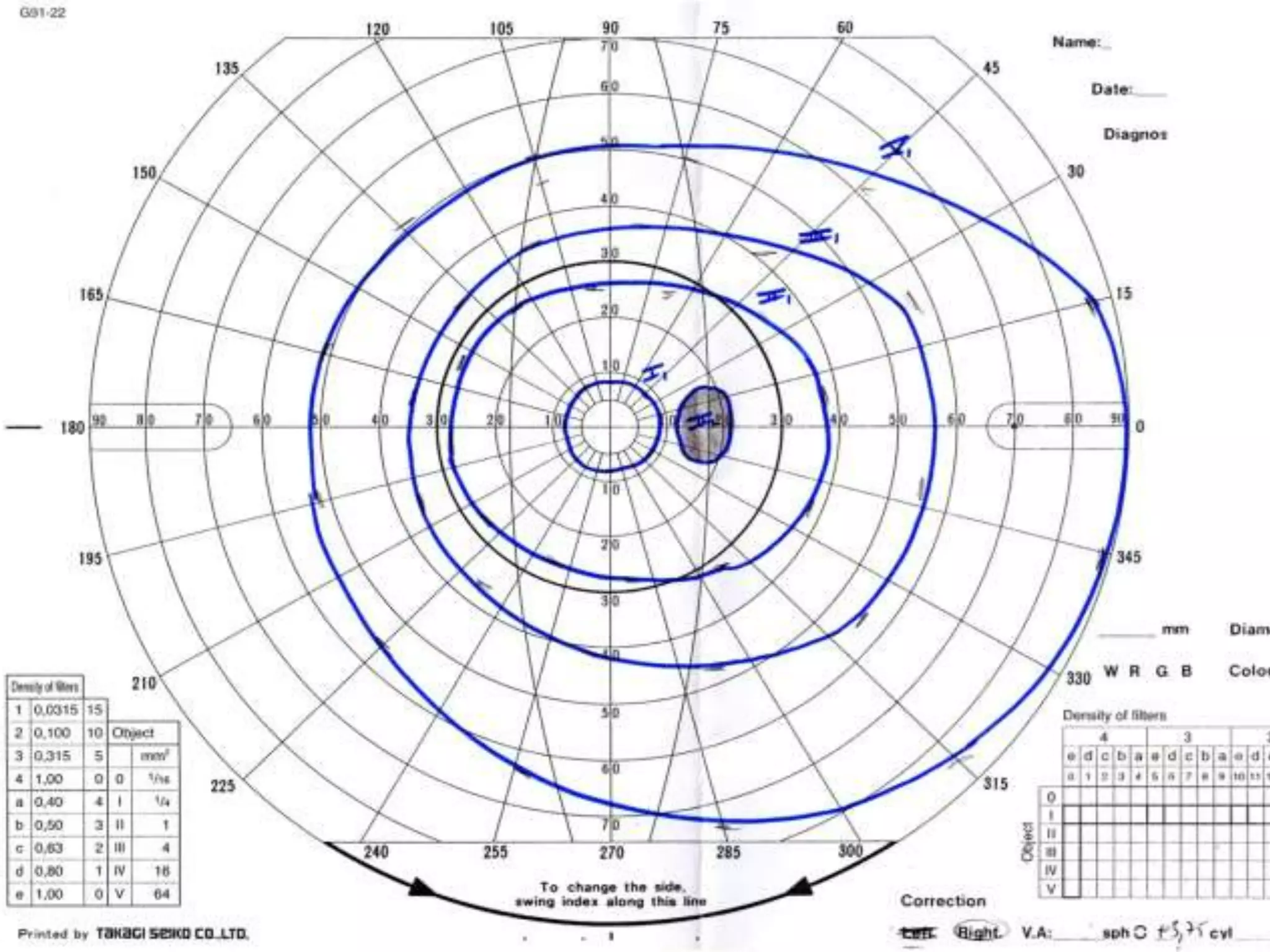
![ Initially observed in Bjerrum area
[ 10-25 degree from fixation]
1) Isopter contracture
2) Baring of blind spot
3) Small wing- shaped paracentral
scotoma
4) Seidel’s scotoma
5) Bjerrum’s scotoma /Arcuate
6) Ring/ Double arcuate scotoma
7) Roenne’s central nasal step
8) Peripheral field defects
9) Advanced glaucomatous field
defects [ tubular vision,
temporal island]](https://image.slidesharecdn.com/mellss-yr4-opthalmology-glaucoma-primary-open-angle-160219174213/75/Mellss-yr4-opthalmology-glaucoma-primary-open-angle-29-2048.jpg)
![1) Tonometry. Applanation tonometry
2) Central corneal thickness [ corrected
readings in < 545 and > 600 microns]
3) Diurnal variation test [ early cases ]
4) Gonioscopy [ rule out other forms of
glaucoma]
5) Documentation of optic disc changes](https://image.slidesharecdn.com/mellss-yr4-opthalmology-glaucoma-primary-open-angle-160219174213/75/Mellss-yr4-opthalmology-glaucoma-primary-open-angle-33-2048.jpg)
![1) Slit-lamp examination [rule out
causes of secondary open angle
glaucoma]
2) Perimetry to detect the visual
field defects.
3) Nerve fibre layer analyzer
(NFLA) detect glaucomatous
damage to retinal nerve fibre
before visual changes
4) Provocative tests [border-line
case]
Water drinking test, bulbar
pressure test, prescoline test,
caffeine test](https://image.slidesharecdn.com/mellss-yr4-opthalmology-glaucoma-primary-open-angle-160219174213/75/Mellss-yr4-opthalmology-glaucoma-primary-open-angle-34-2048.jpg)
![Class Used in Mechanism of
action
Prostaglandin analogues
• Latanoprost 0.005
• Travoprost 0.004
• Bimatoprost 0.003
• Unoprostone 0.15
• First choice
• Good adjunctive drug
• Incease uveo-
scleral outflow
Topical beta-blockers
• Timolol maleate ( 0.25,
0.5% )
• Betaxolol (0.25% )
• Levobunolol (0.25, 0.5%)
• Carteolol (1%)
First choice in poor
• initial therapy, not in
bronchial asthma /heart
blocks.
• Cardiopulmonary problems.
• Once a day use
• hyperlipidemias
/atherosclerotic
cardiovascular disease.
• Reduces
aqueous
secretion [beta -
receptors in the
ciliary
processes].](https://image.slidesharecdn.com/mellss-yr4-opthalmology-glaucoma-primary-open-angle-160219174213/75/Mellss-yr4-opthalmology-glaucoma-primary-open-angle-39-2048.jpg)
![Class Used in Mechanism of action
Adrenergic drugs.
Epinephrine
hydrochloride (0.5, 1, 2%)
Dipivefrine hydrochloride
(0.1%)
• Combination therapy:
failure of filtration
[glaucoma surgery,
• allergy]
increasing aqueous
outflow by stimulating
beta
recepters in the aqueous
outflow system
Brimonidine (0.2%) • second drug of choice ,
combination therapy
• [allergy and
tachyphylaxis]
lowers IOP by
decreasing aqueous
production
Dorzolamide
(2%: 2-3 times/day)
• second line of drug
adjunct drug.
decreasing aqueous
secretion by altering ion
transport along ciliary
epithelium
Pilocarpine
(1, 2, 4%: 3-4 times/day).
• adjunctive therapy
• second choice (poor
patient)
• [accommodation and
miosis spasm in young ]
mechanically
increasing aqueous
outflow](https://image.slidesharecdn.com/mellss-yr4-opthalmology-glaucoma-primary-open-angle-160219174213/75/Mellss-yr4-opthalmology-glaucoma-primary-open-angle-40-2048.jpg)
![Non- penetrating filteration surgeries
anterior chamber not
entered. [reduce post-
operative endophthalmitis,
overfiltration and
hypotony]
disadvantage : less IOP
control
1. Deep sclerectomy.
partial thickness scleral
flap, a second deep partial
thickness scleral flap is
fashioned and excised
leaving very thin sclera,
trabeculum and
Descemet’s membrane
superficial scleral flap is
loosly approximated and
conjunctival incision
closed.
2. Viscocanalostomy.
similar to deep
sclerectomy, except that
after excising the deeper
scleral flap, high viscosity
viscoelastic substance is
injected into the
Schlemm's canal with a
special cannula.](https://image.slidesharecdn.com/mellss-yr4-opthalmology-glaucoma-primary-open-angle-160219174213/75/Mellss-yr4-opthalmology-glaucoma-primary-open-angle-54-2048.jpg)
![High risk factors :
Ocular hypertension study
[ OHTS] & European
Glaucoma Prevention
Study [ EGPS]
IOP> 30mmHg
CCT > 550µm
Vertical cup :disc > 0.7
Increased age
Increased pattern
standard deviation (PSD)
on Humphrey visual field
test
Disc haemmorrhages
Other risk factors :
Family history
Fellow eye of unilateral
POAG
Ocular condition: myopia,
steroid responder , positive
diurnal variation
Systemic: DM , sleep
apnea, hypertension,
hypothyroidism,
migranous headaches and
vasospasm](https://image.slidesharecdn.com/mellss-yr4-opthalmology-glaucoma-primary-open-angle-160219174213/75/Mellss-yr4-opthalmology-glaucoma-primary-open-angle-60-2048.jpg)
![ 1.Medical treatment
lower IOP by 30% [12-14 mm
of Hg]
Betaxolol ,drug of choice
[lowering IOP , increases
optic nerve blood flow]
Avoid other beta blockers
and adrenergic drugs
(nocturnal systemic
hypotension )
Neuroprotective effect –
brimonidine
Prostaglandin analogues,
e.g., latanoprost [greater
ocular hypotensive effect in
eyes with normal IOP]
2. Trabeculectomy
progressive field loss
3. Systemic calcium channel
blockers (e.g., nifedipine)
patients with peripheral
vasospasm.
4. Monitoring of systemic
blood pressure should
bedone for 24 hours. avoid
night dose of anti-
hypertensive.](https://image.slidesharecdn.com/mellss-yr4-opthalmology-glaucoma-primary-open-angle-160219174213/75/Mellss-yr4-opthalmology-glaucoma-primary-open-angle-65-2048.jpg)