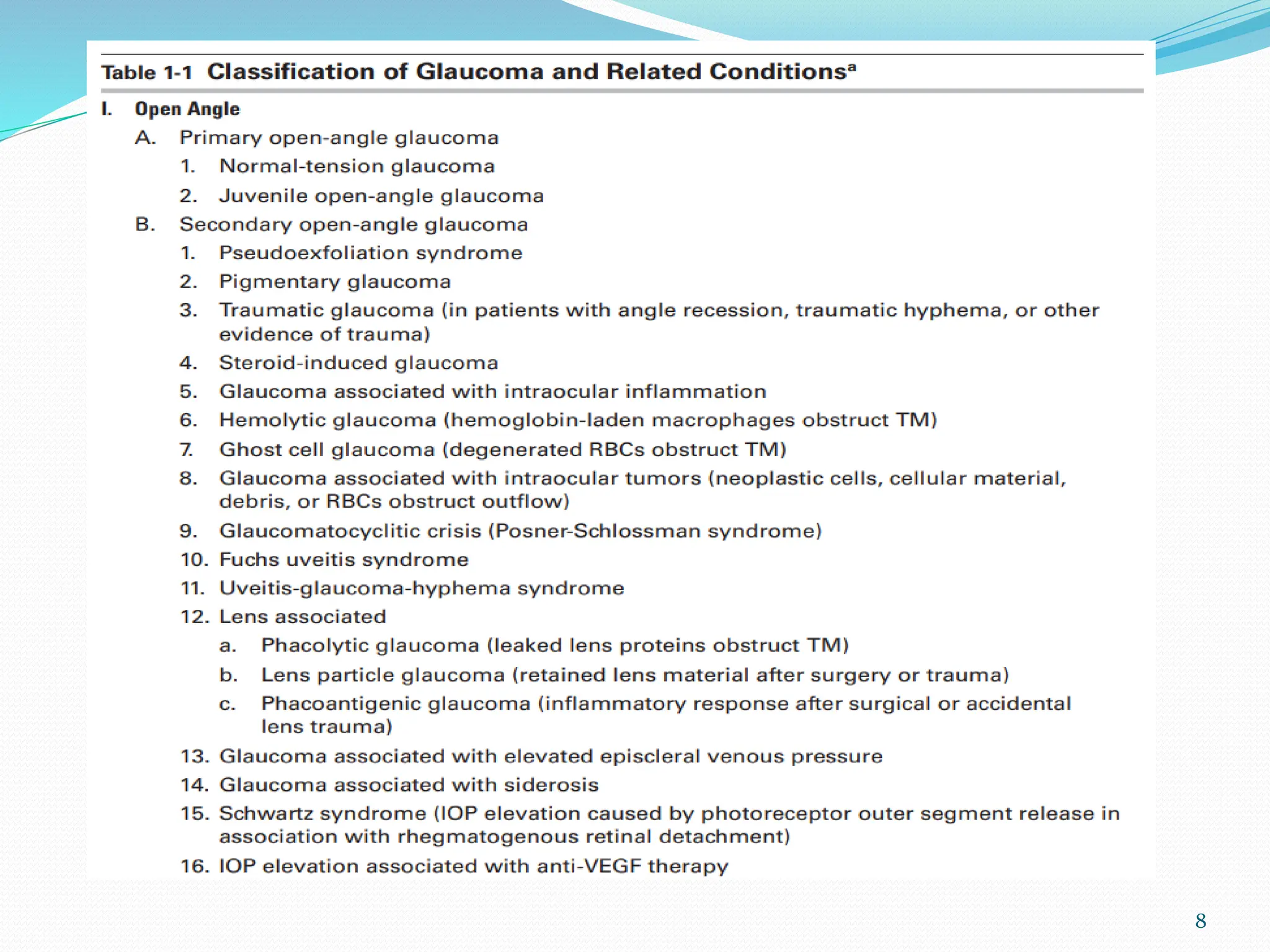
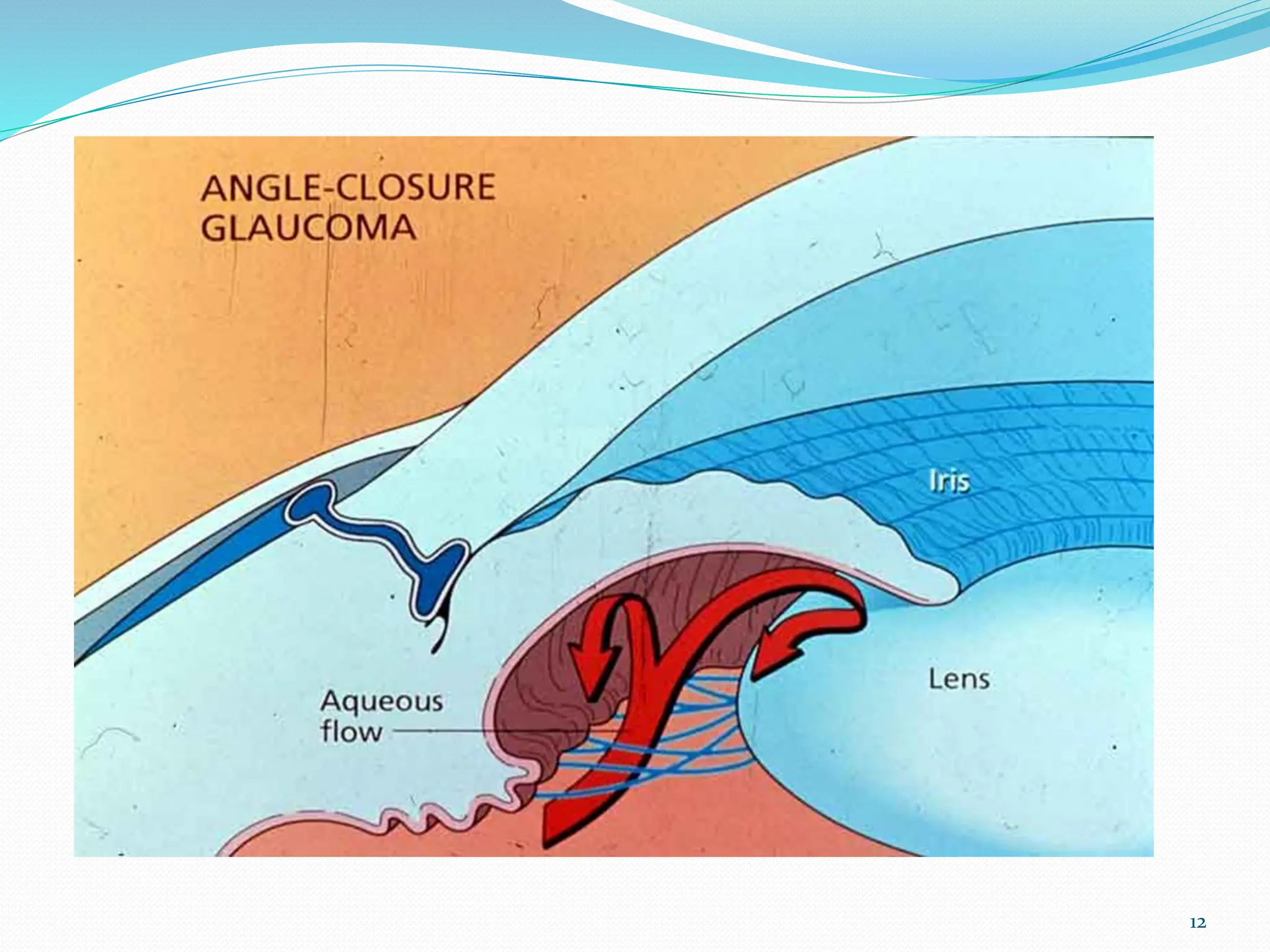
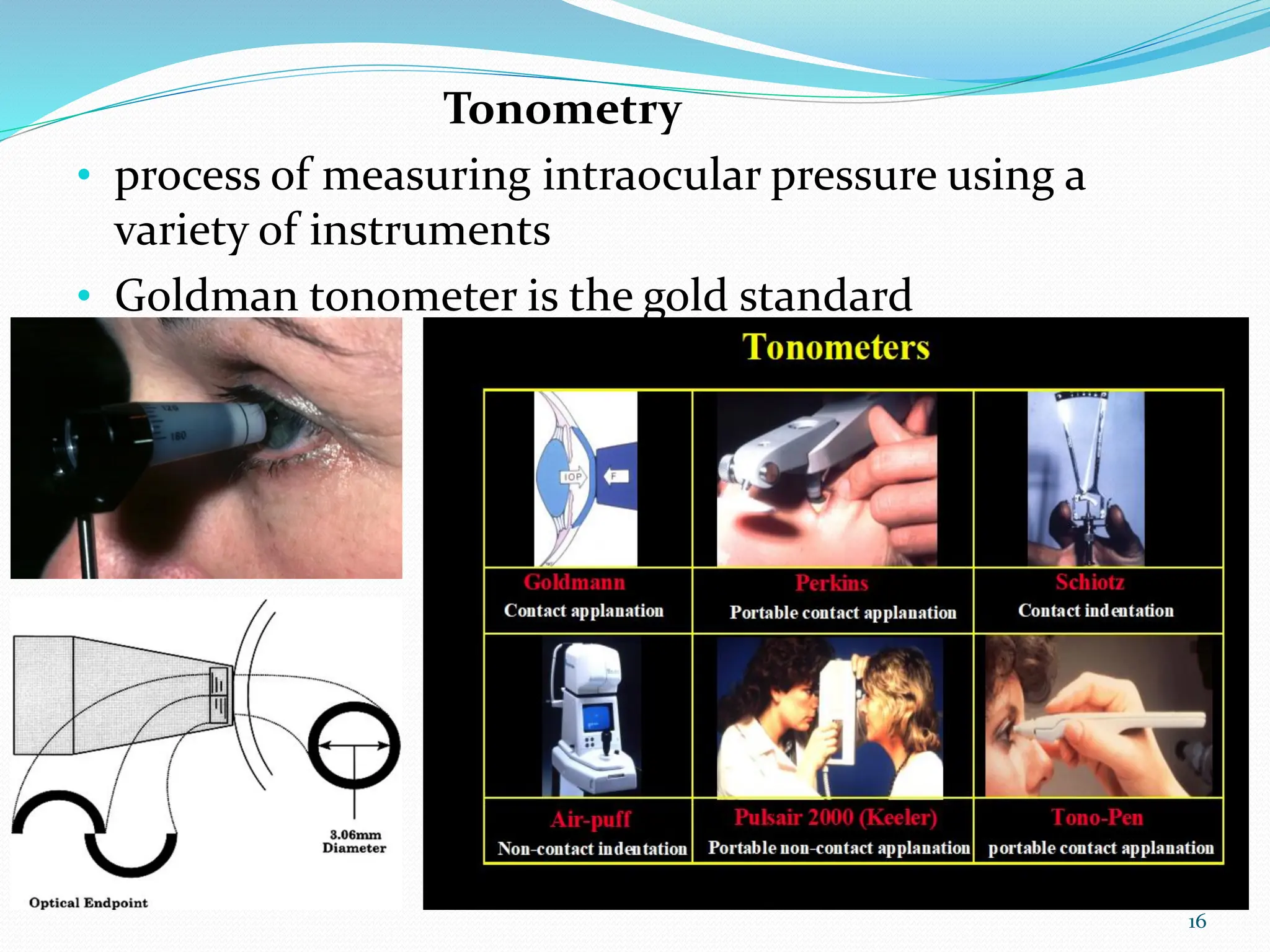
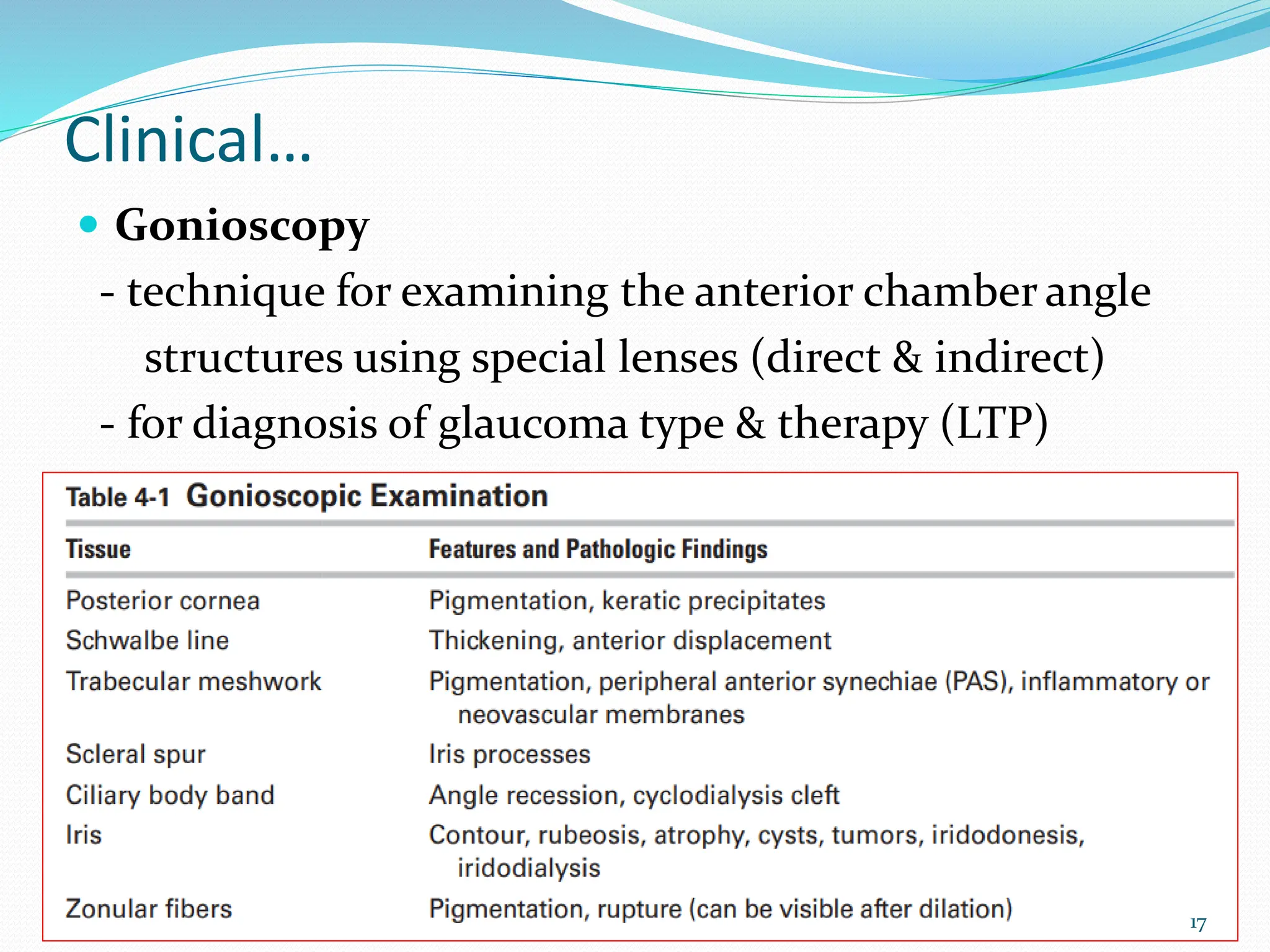
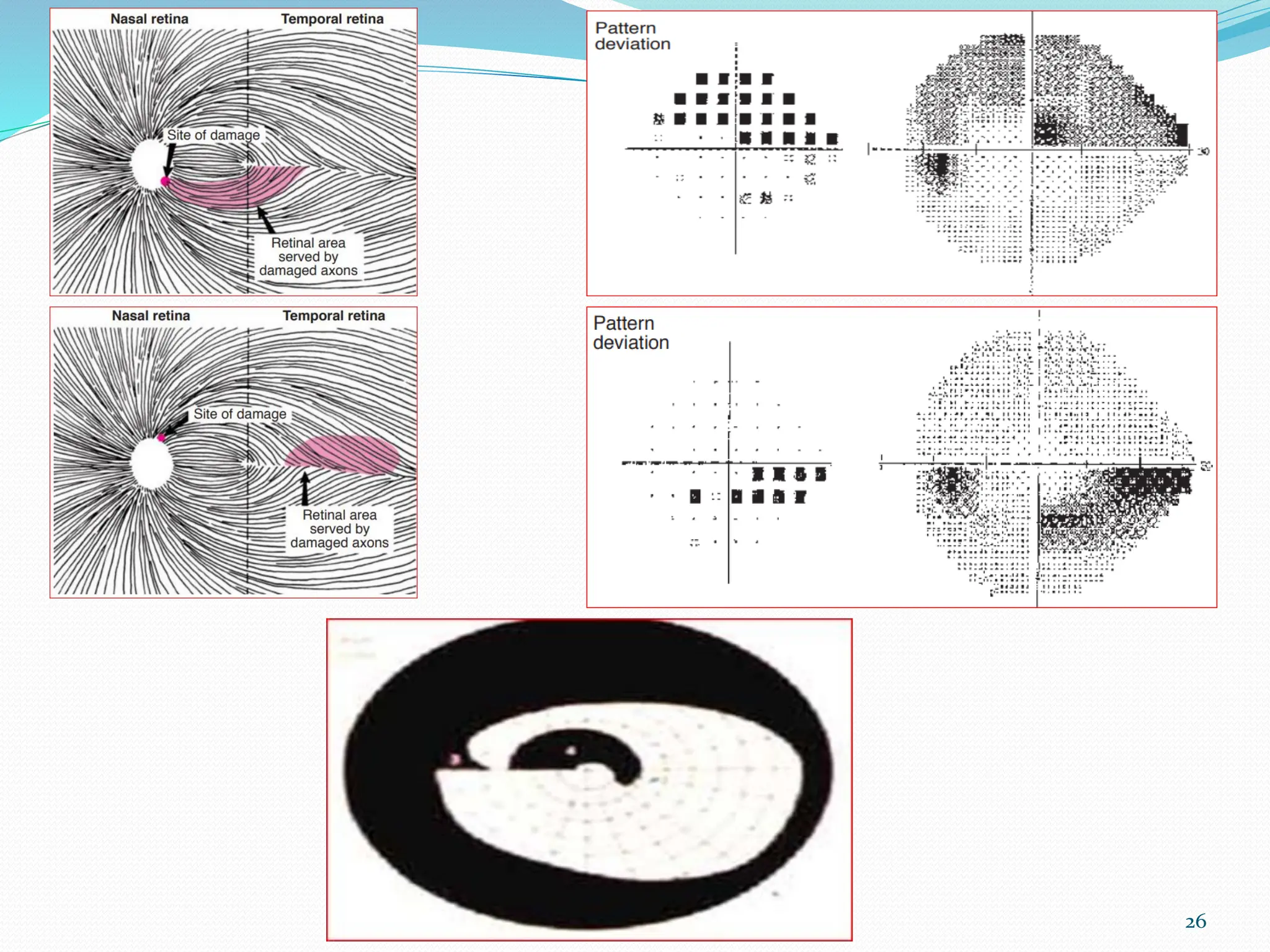
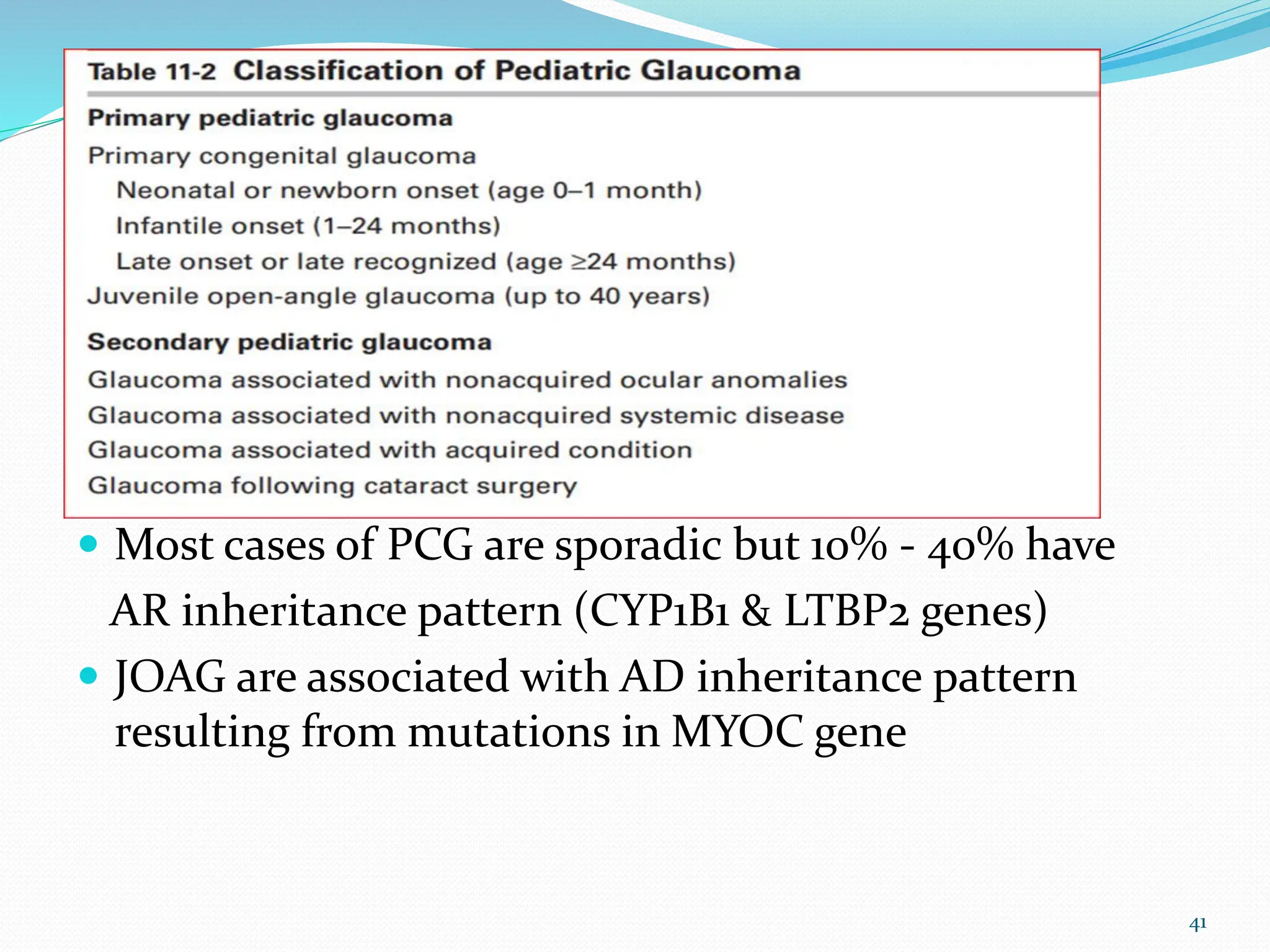
The document provides a comprehensive overview of glaucoma, including its definitions, classifications (open-angle, angle-closure, and pediatric glaucoma), clinical evaluation methods, and management strategies. It emphasizes the importance of early diagnosis and treatment to prevent irreversible visual loss, detailing various risk factors, symptoms, and evaluation techniques such as tonometry and visual field tests. Additionally, it outlines medical and surgical management options aimed at lowering intraocular pressure to preserve visual function.