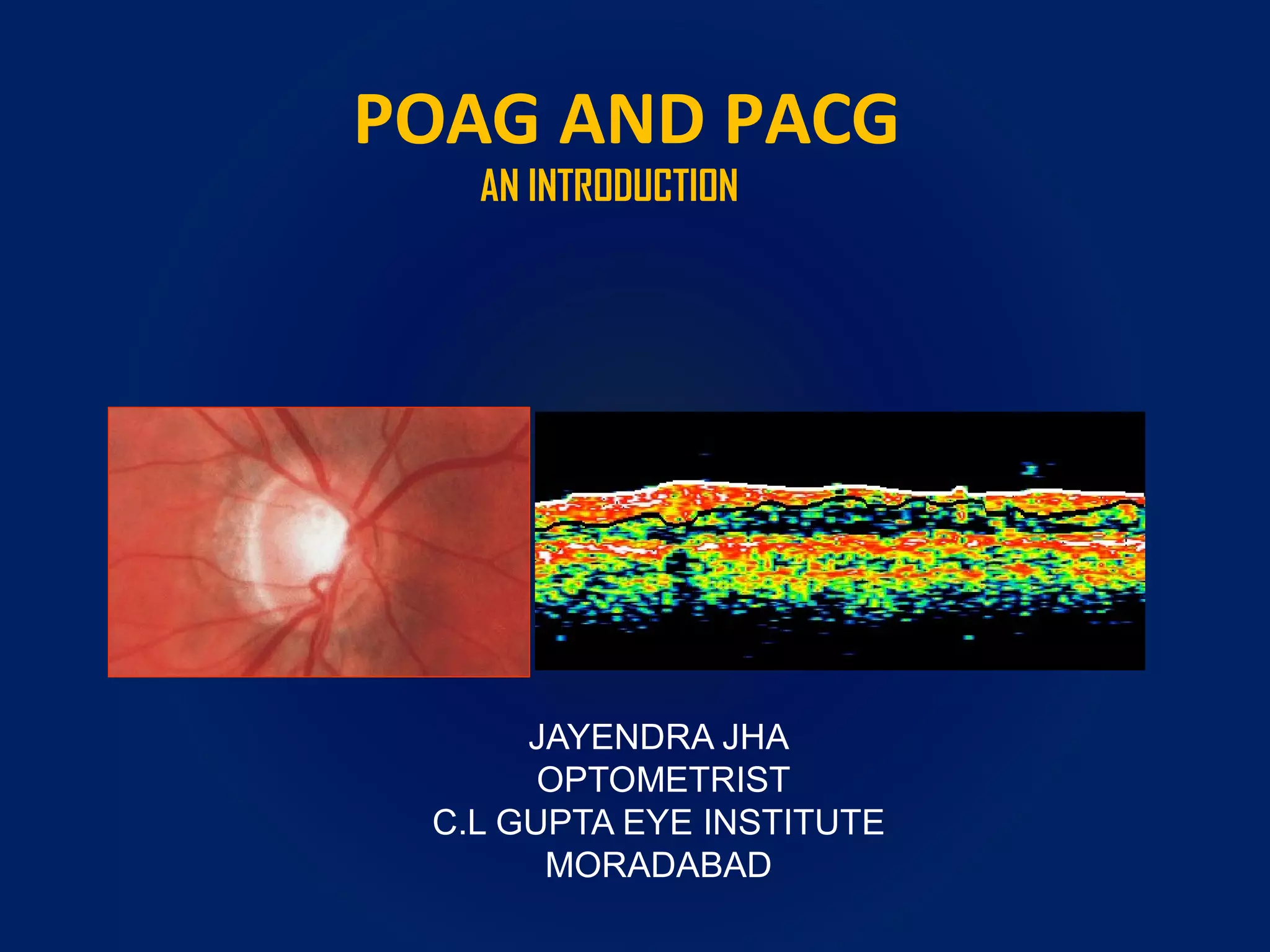
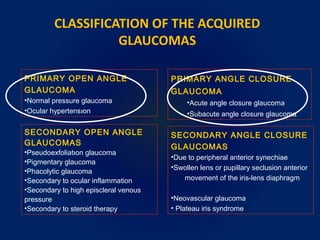
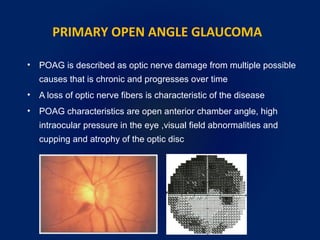
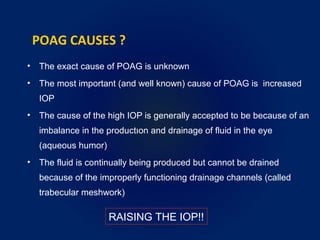
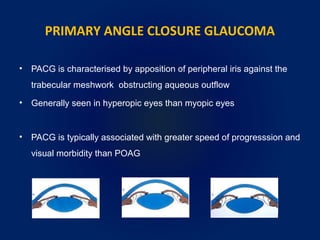
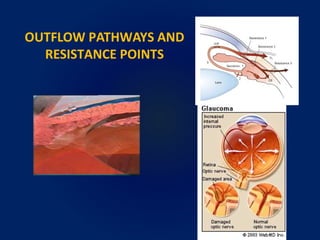
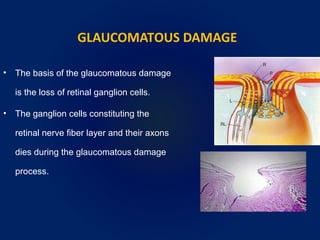
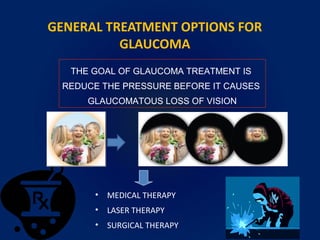
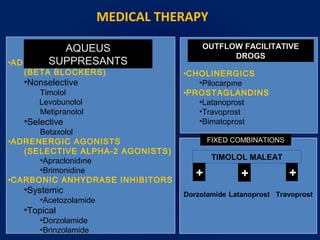
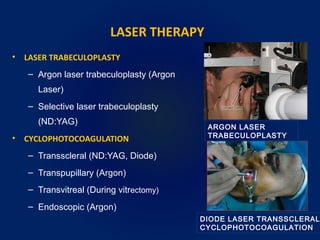
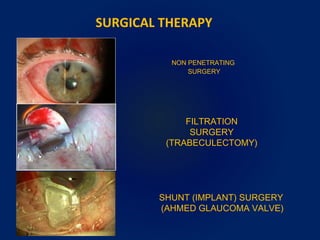
POAG and PACG are two major types of glaucoma. POAG is caused by increased intraocular pressure due to improper drainage of fluid from the eye. It progresses slowly and causes damage to the optic nerve and visual field loss over time. PACG occurs when the iris blocks the drainage angle, often in hyperopic eyes, and can progress more rapidly. Treatment options include medications, laser therapy, and surgery to lower pressure and prevent further vision loss. Regular eye exams are important for early detection and management of glaucoma.