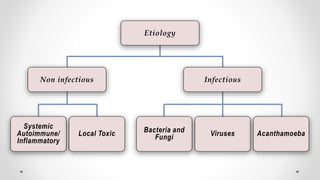
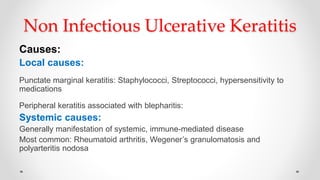
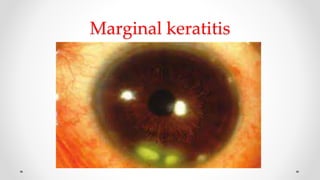
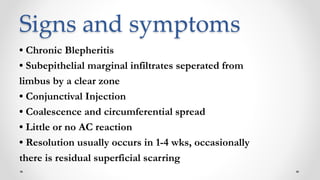
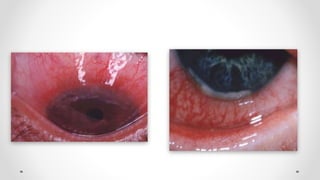
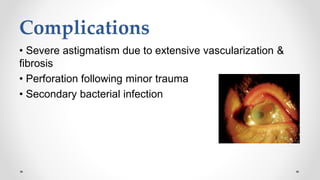
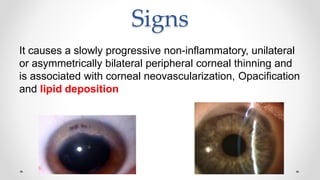
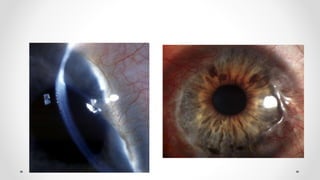
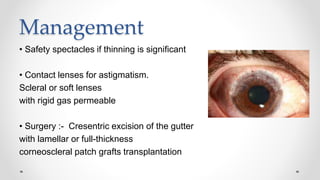
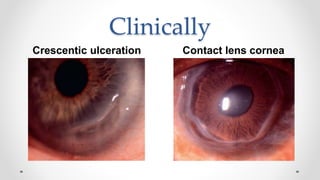
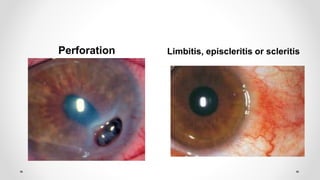
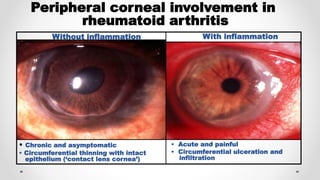
Non-infectious corneal ulcers can be caused by local factors like punctate marginal keratitis due to hypersensitivity to medications or peripheral keratitis associated with blepharitis, or systemic immune-mediated diseases like rheumatoid arthritis. Marginal keratitis is characterized by chronic blepharitis and subepithelial marginal infiltrates separated from the limbus by a clear zone. Mooren's ulcer is a rare autoimmune disease seen as progressive peripheral circumferential stromal ulceration. Terrien marginal degeneration is an idiopathic thinning of the peripheral cornea. Peripheral ulcerative keratitis can be associated with underlying systemic autoimmune diseases like rheumatoid arthritis.