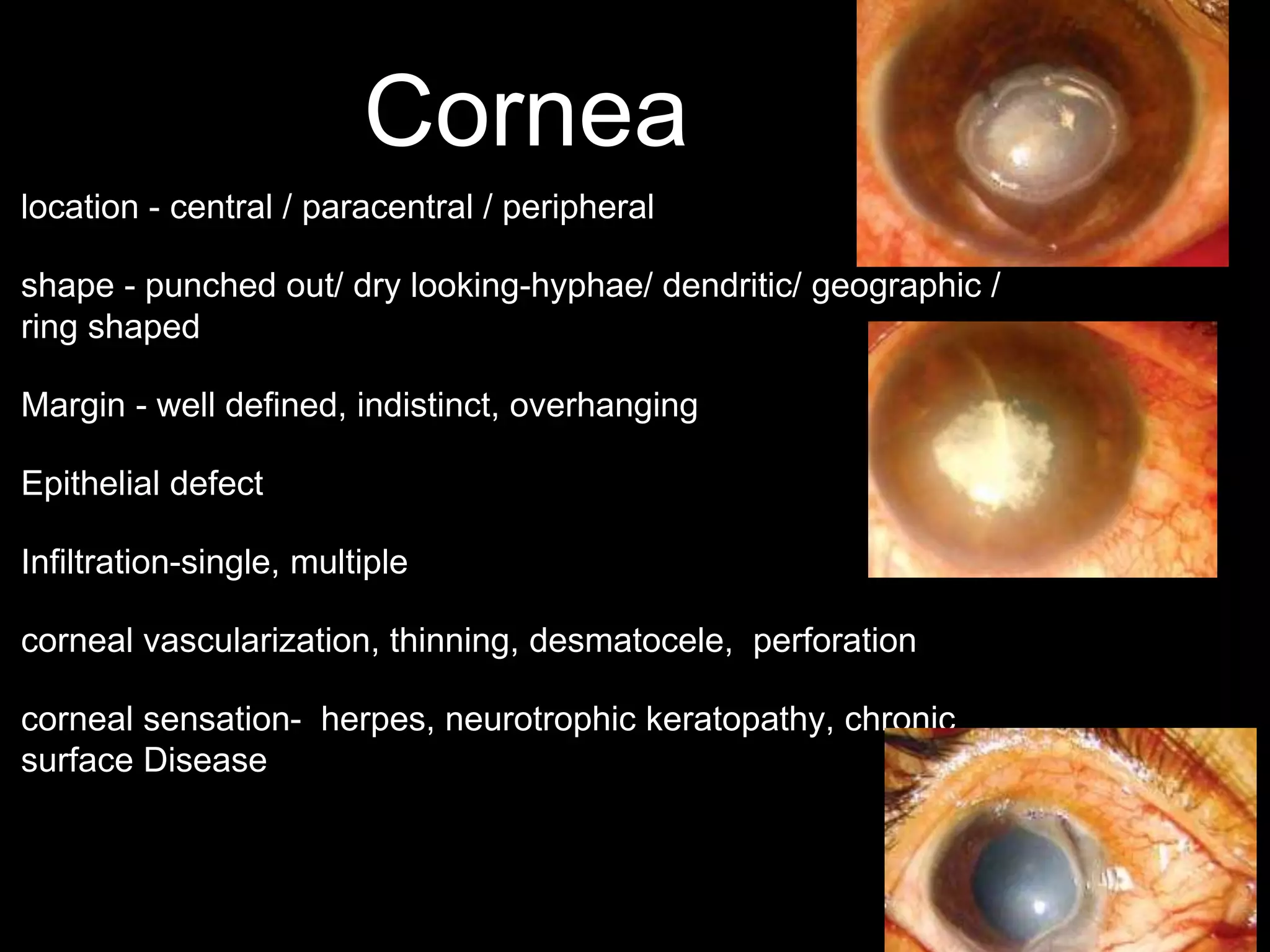
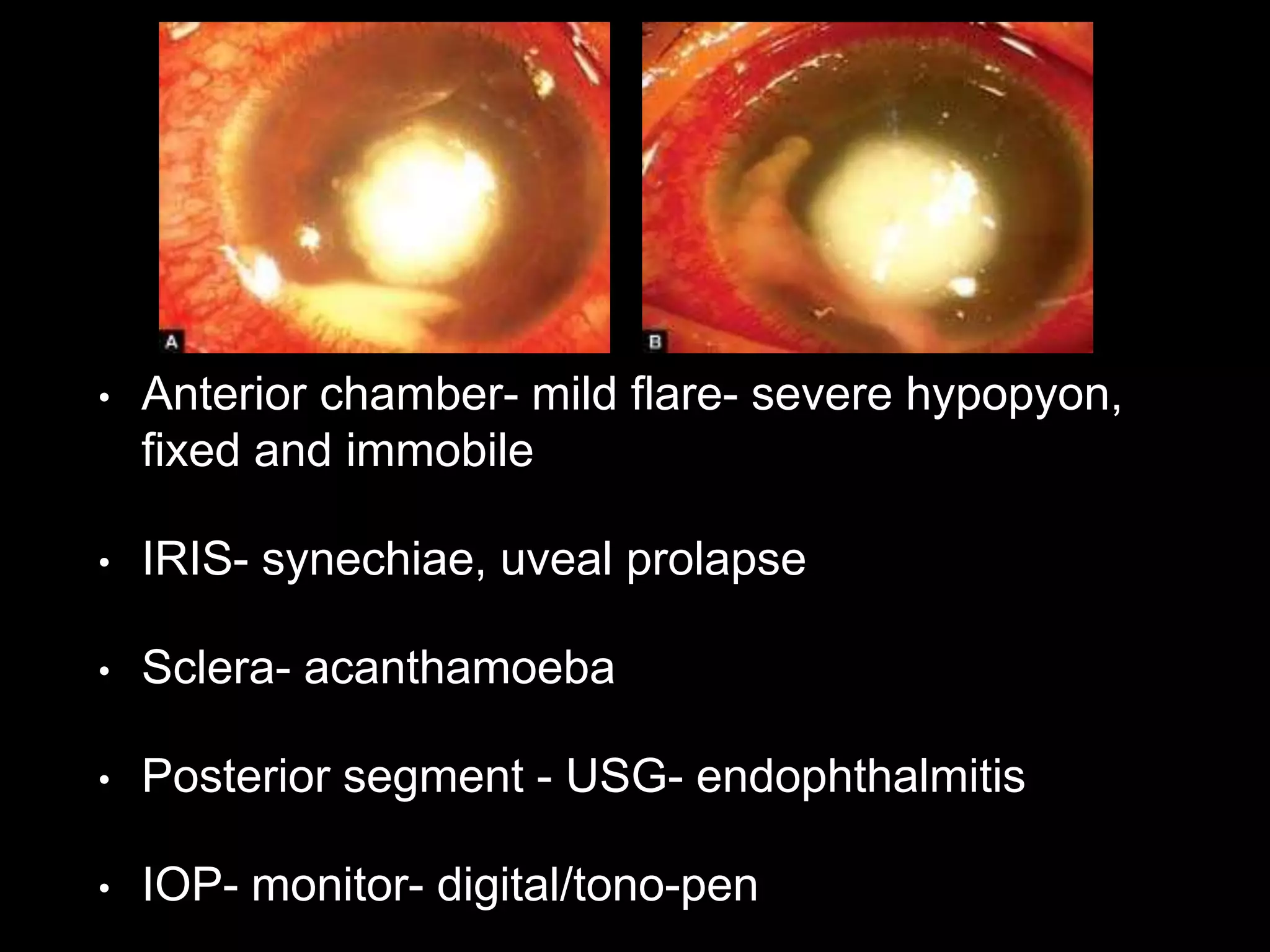
This document discusses corneal ulcers, including their definition, causes, microbiology, pathogenesis, stages, grading, symptoms, clinical examination, investigations, treatment, and complications. Key points include:
- Corneal ulcers are tissue excavations associated with epithelial defects, edema, infiltration and necrosis. They are usually caused by injury or foreign materials that allow microbial infection.
- Common microbes include bacteria (e.g. streptococcus, pseudomonas), fungi (e.g. candida, fusarium), protozoa (e.g. acanthamoeba), and viruses (e.g. herpes).
- Treatment involves local and systemic antibiotics, antifungals, or antiv