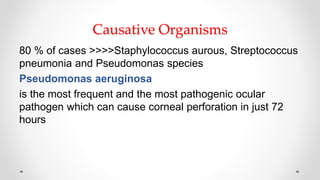
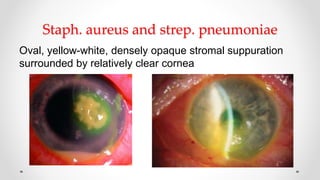
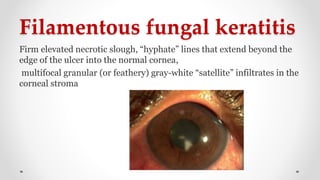
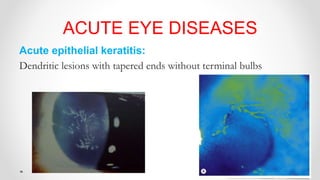
The document provides an overview of corneal ulcers, detailing their definitions, classifications, and types—both infectious and non-infectious. It highlights important facts regarding the management of corneal diseases, including treatment principles and specific management strategies for various etiologies such as bacterial, fungal, and viral keratitis. The document emphasizes the urgency of corneal ulcers as ocular emergencies that potentially lead to significant vision loss.