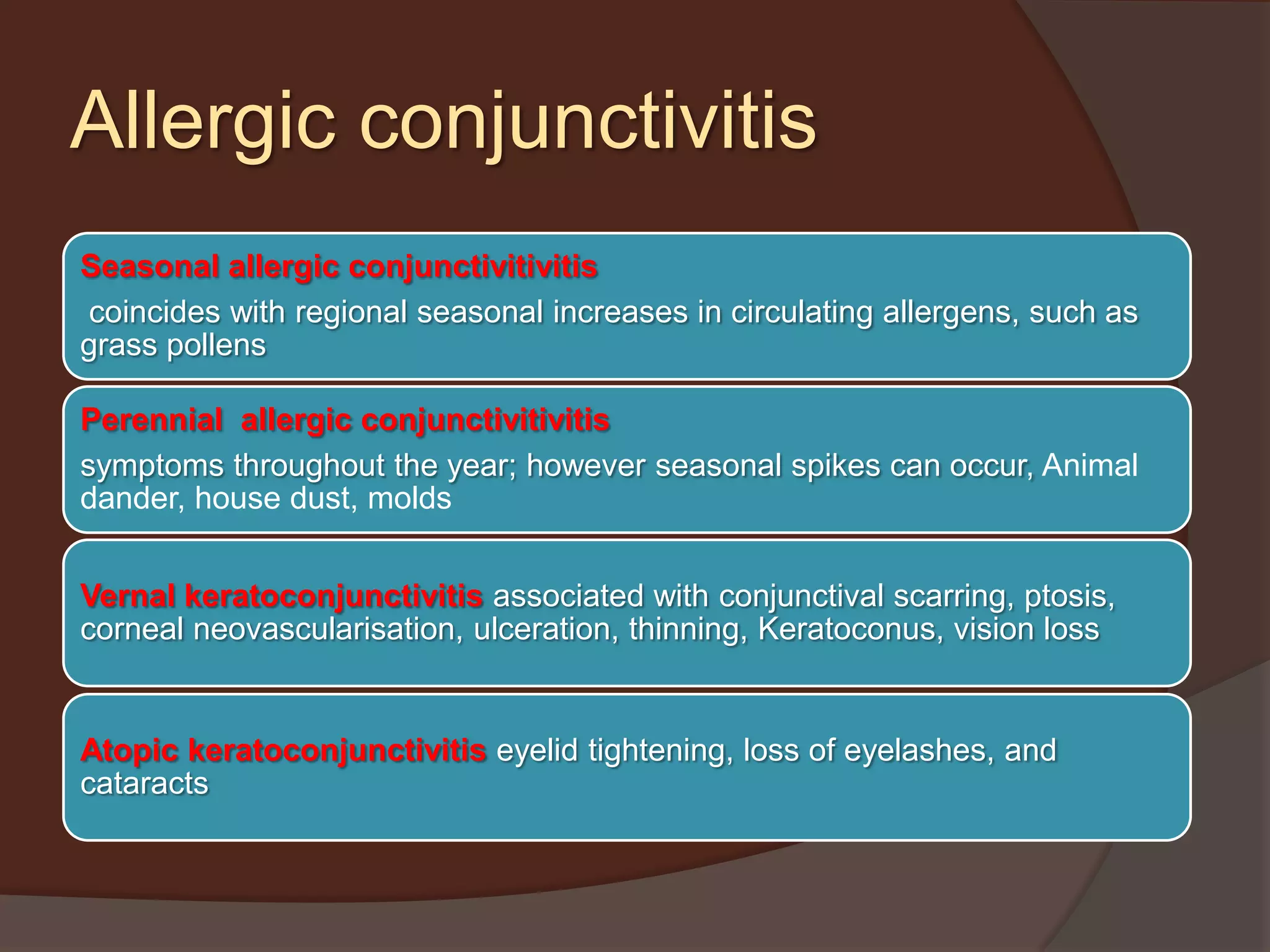
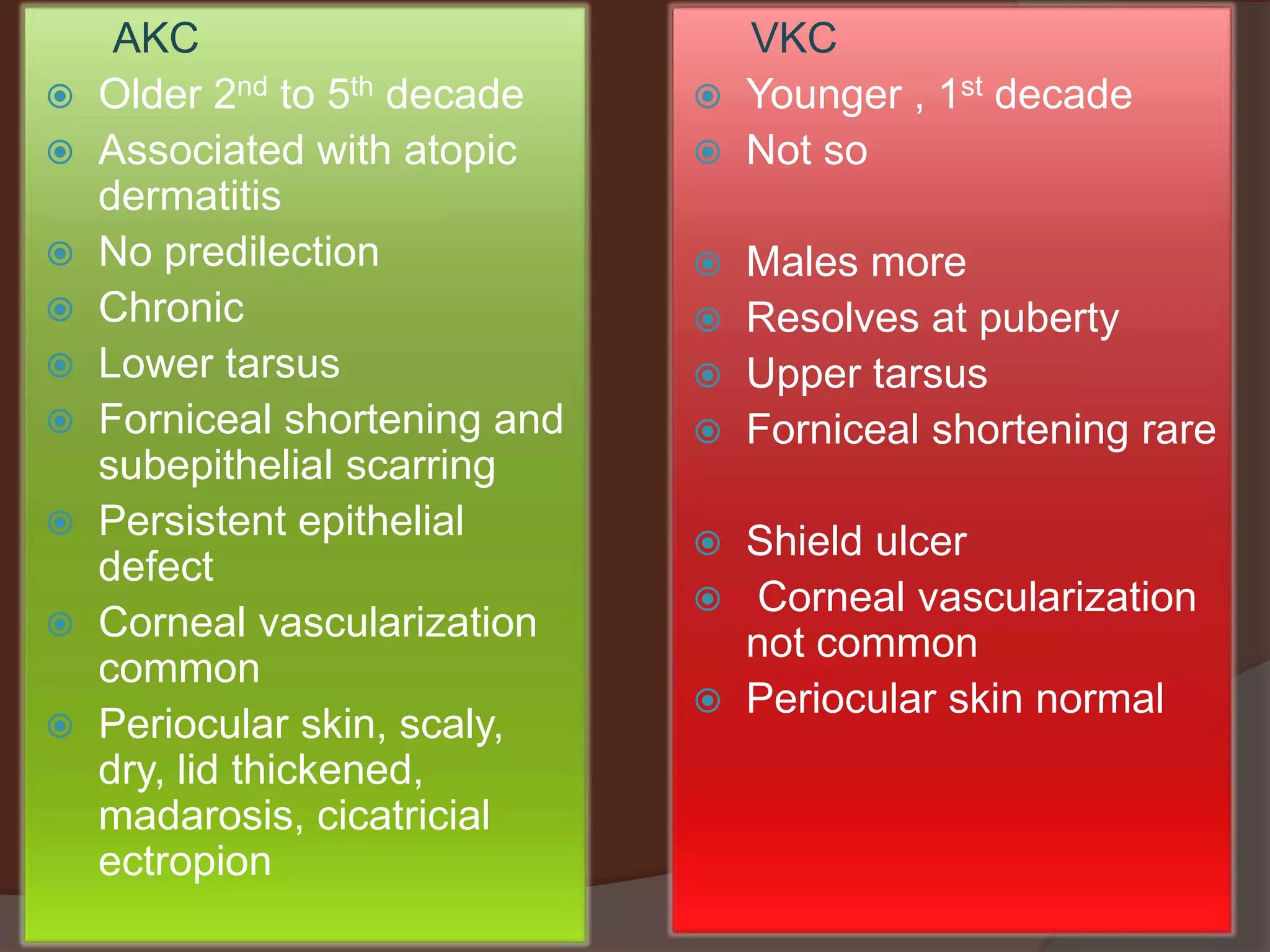
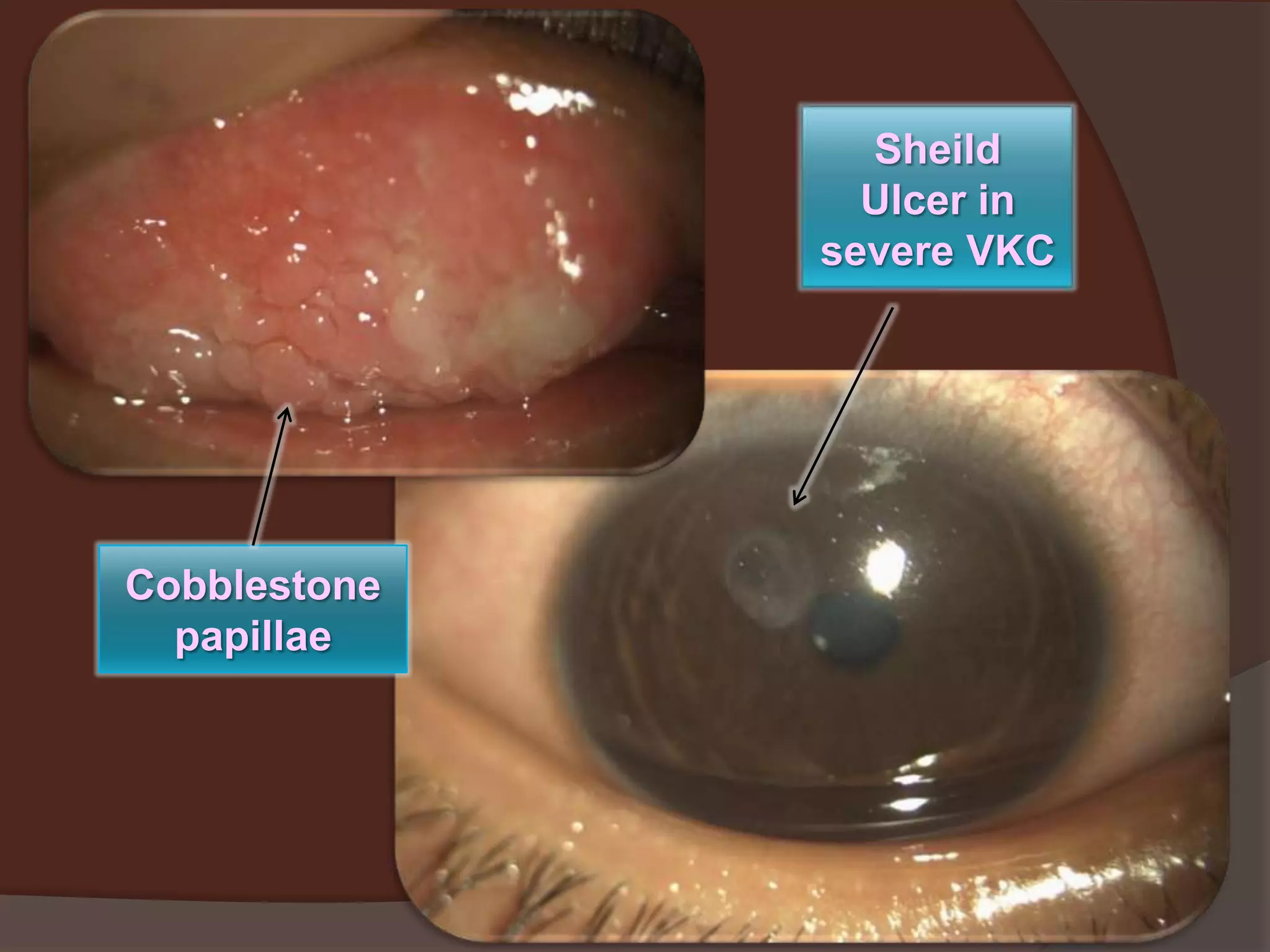
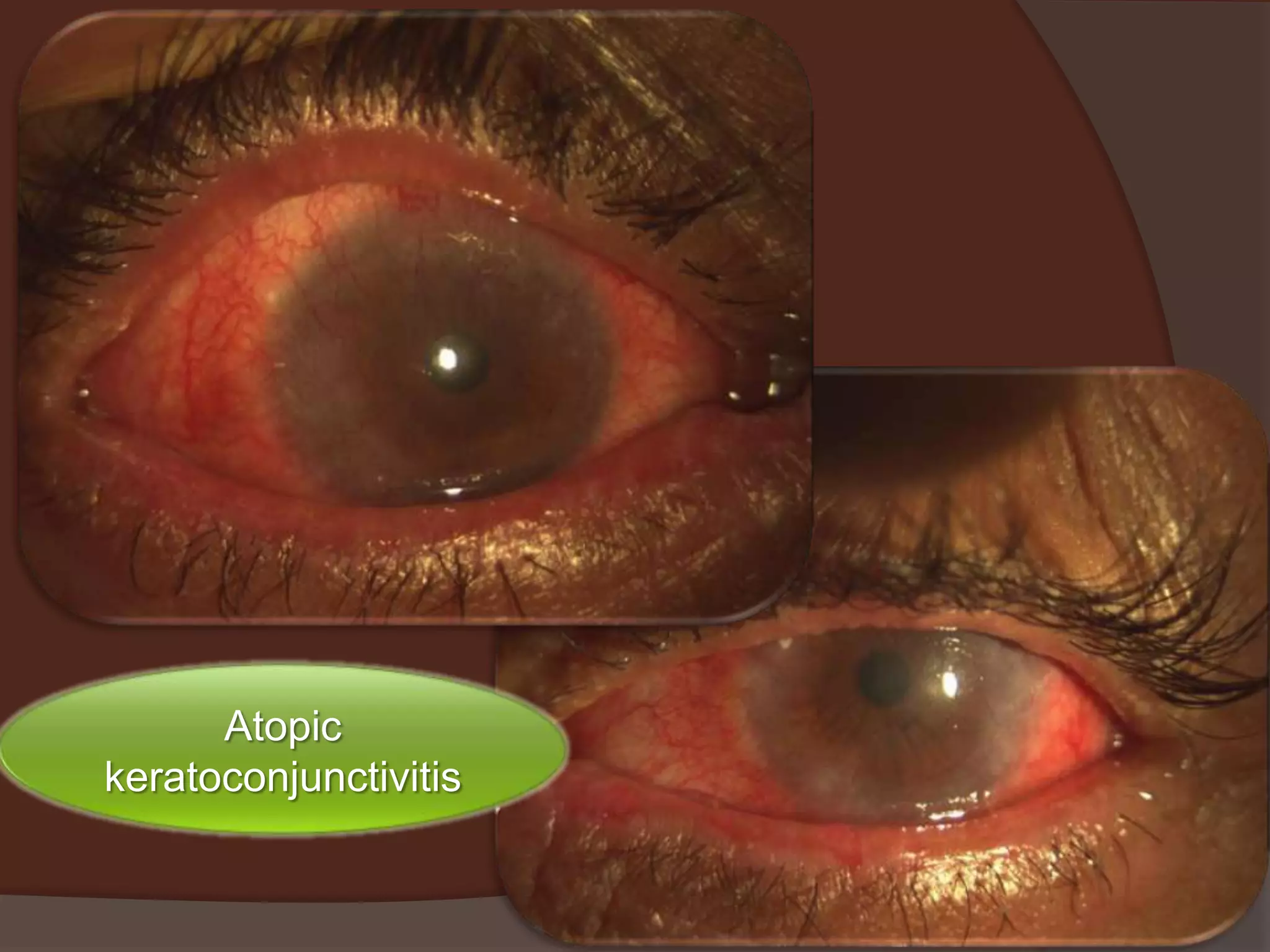
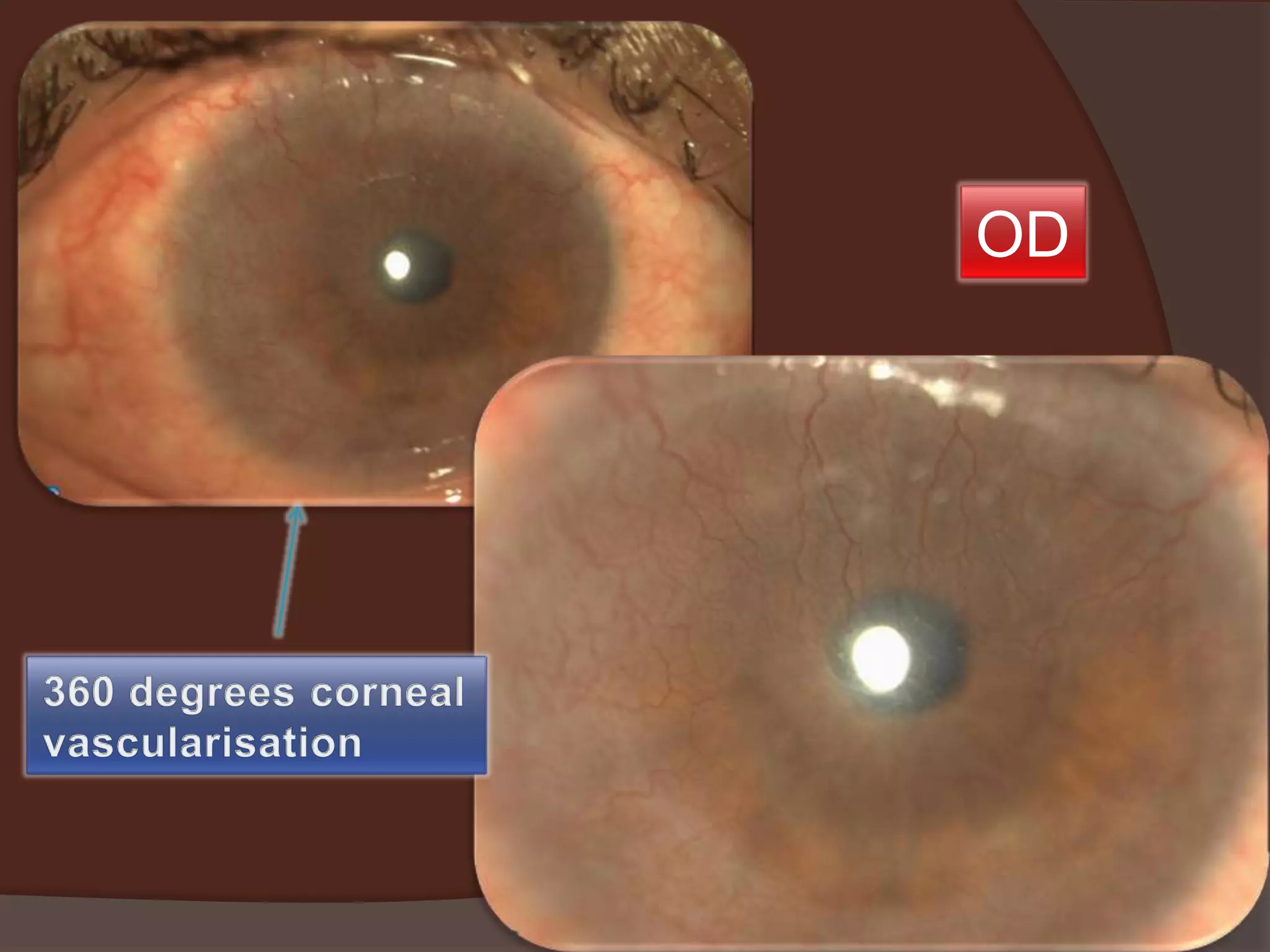
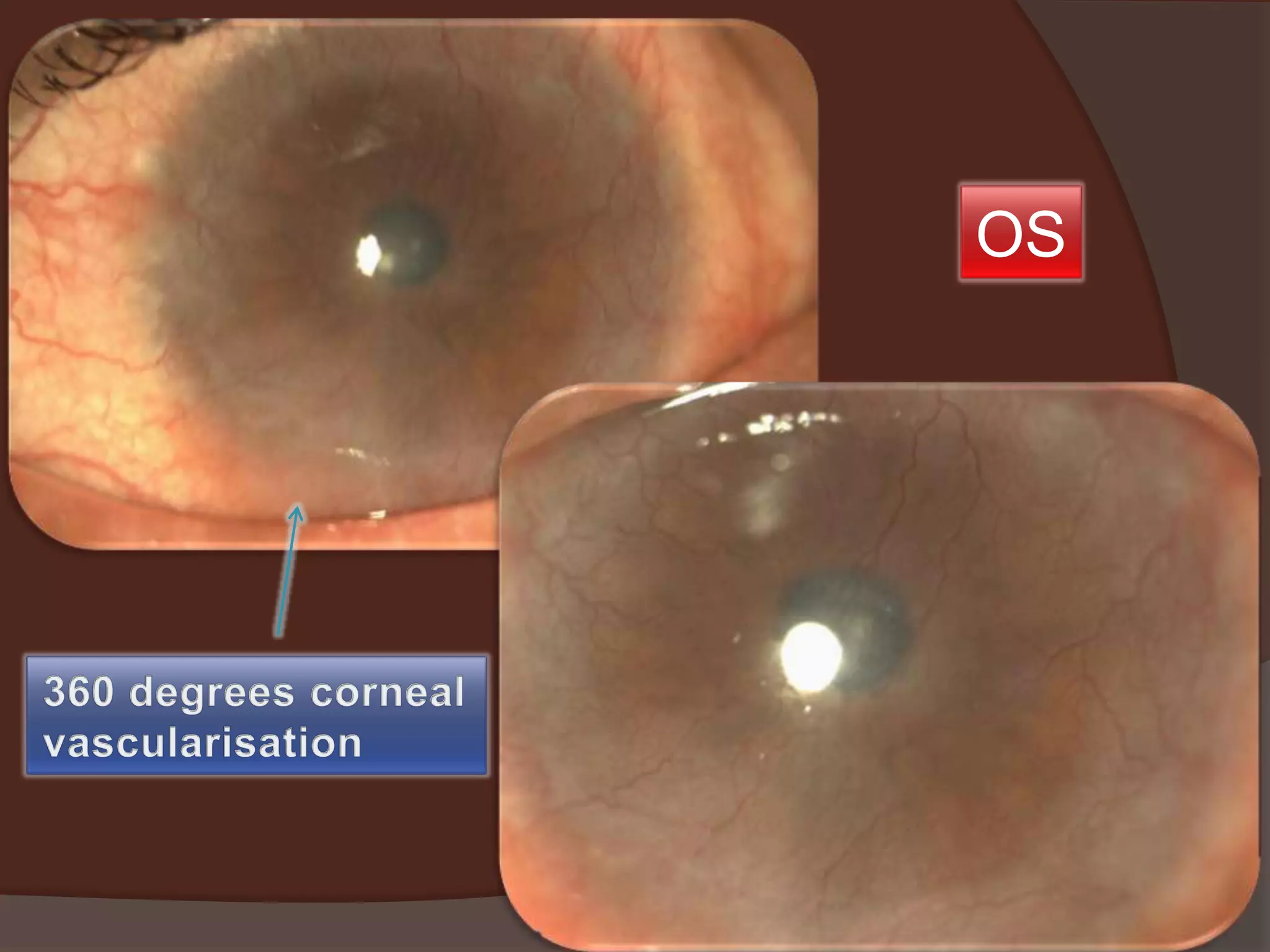
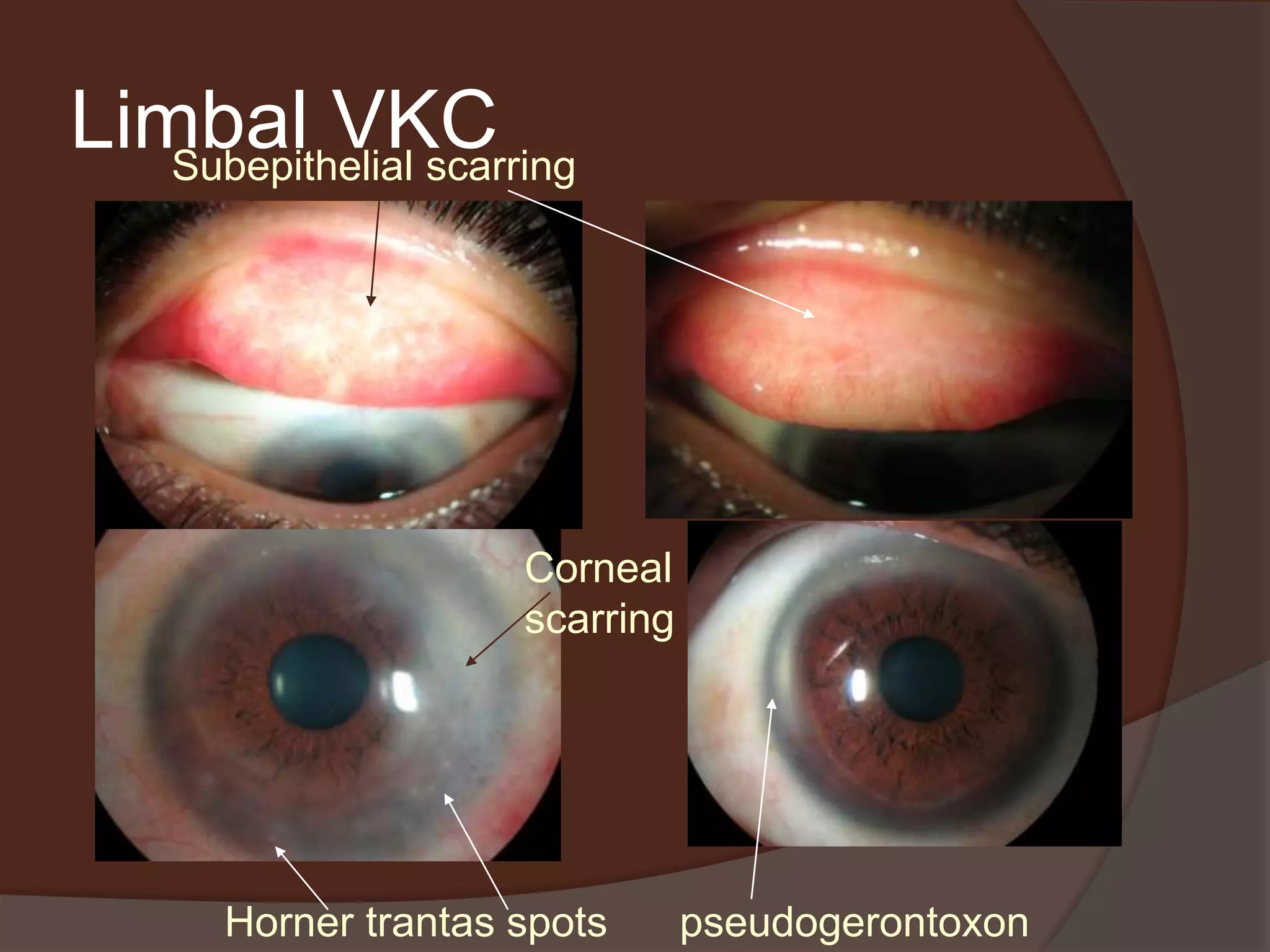
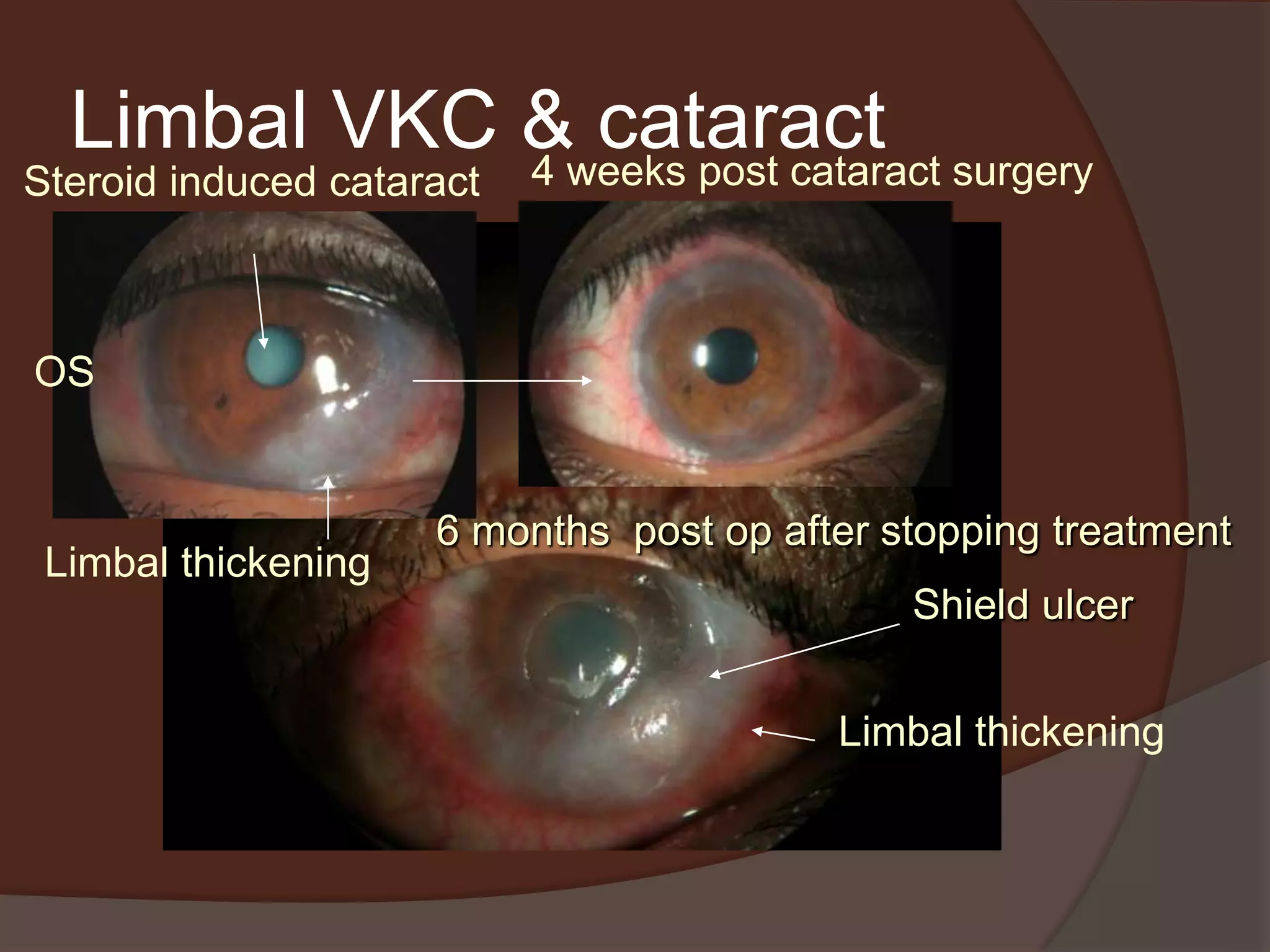
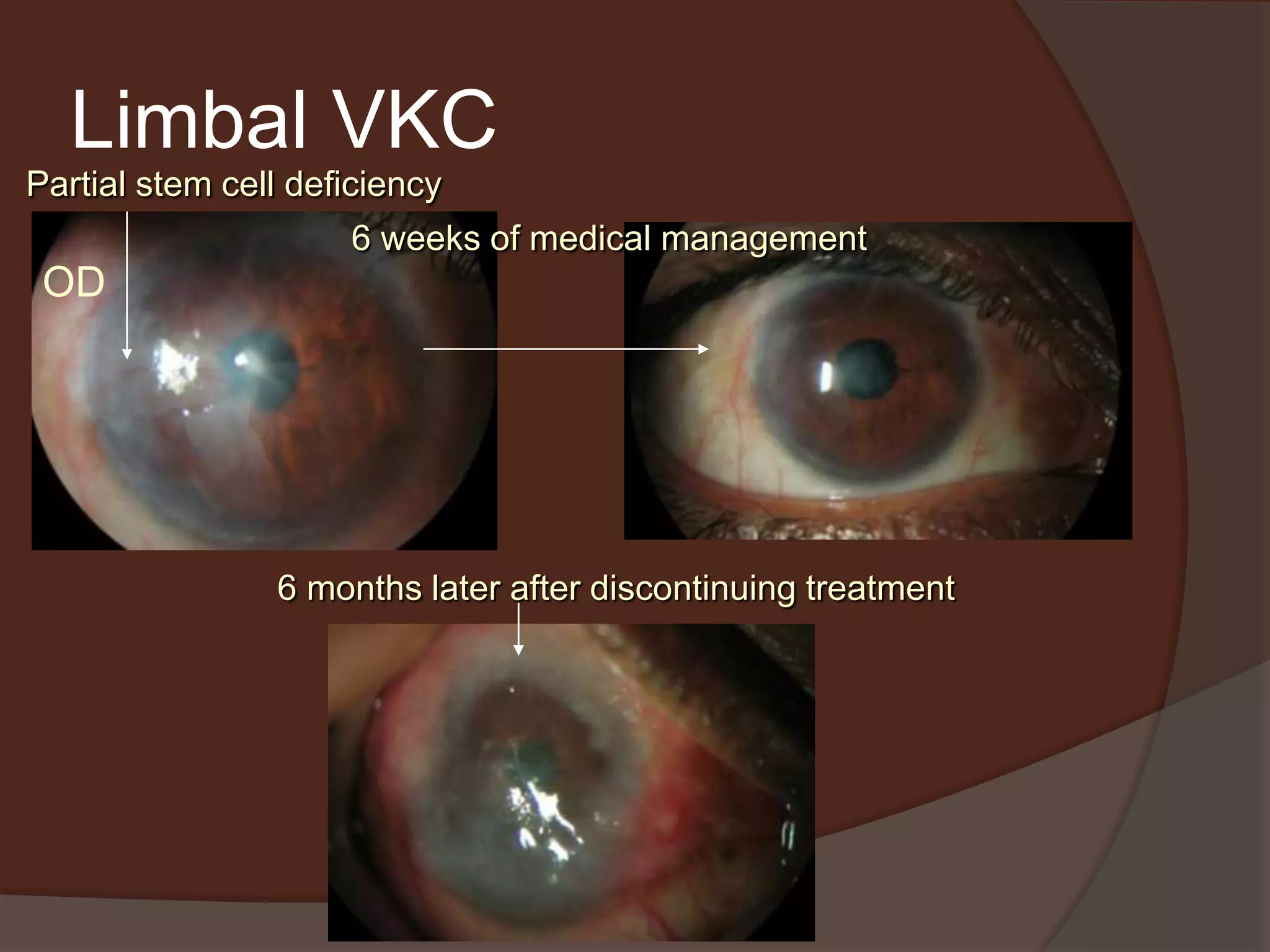
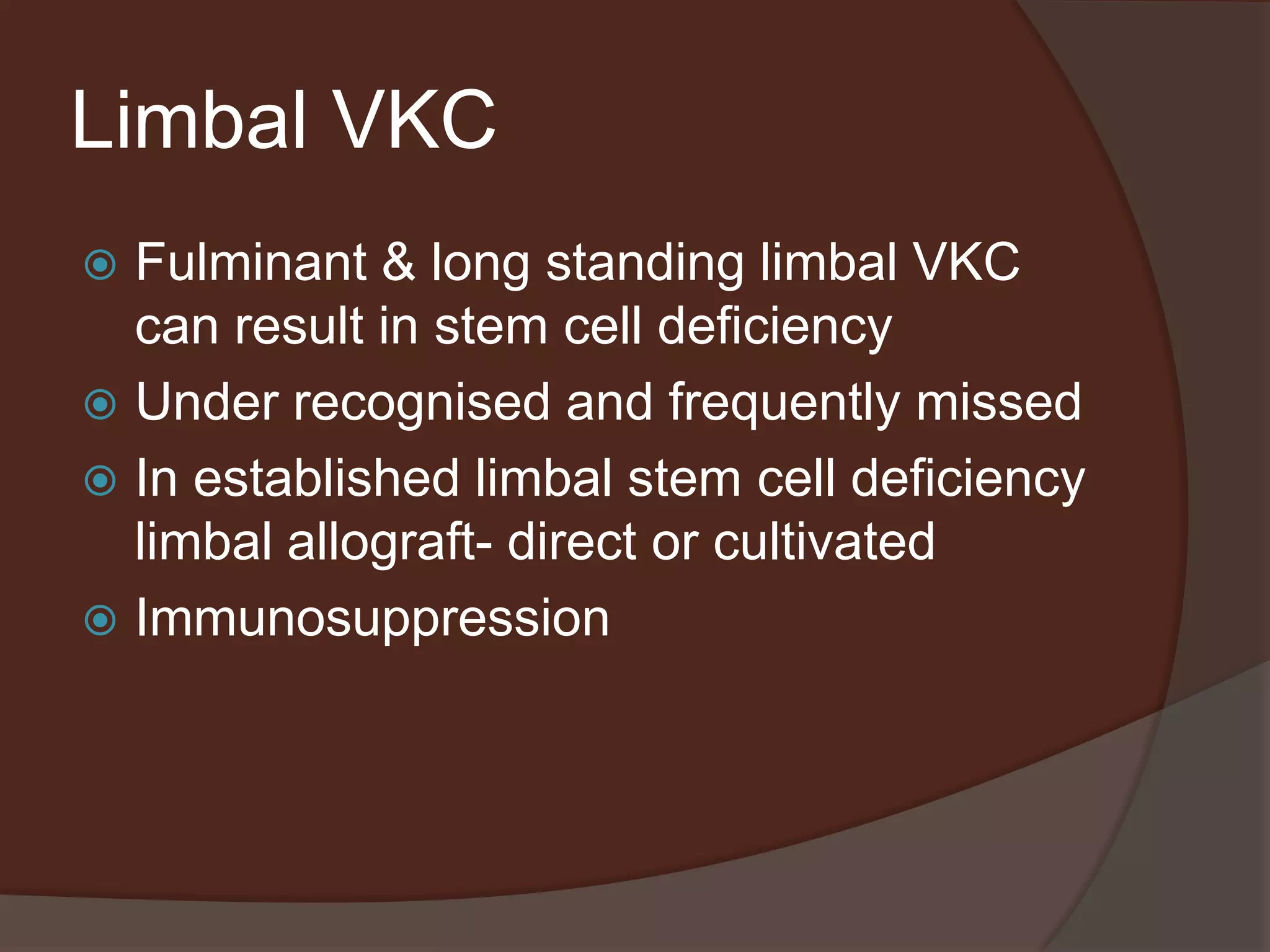
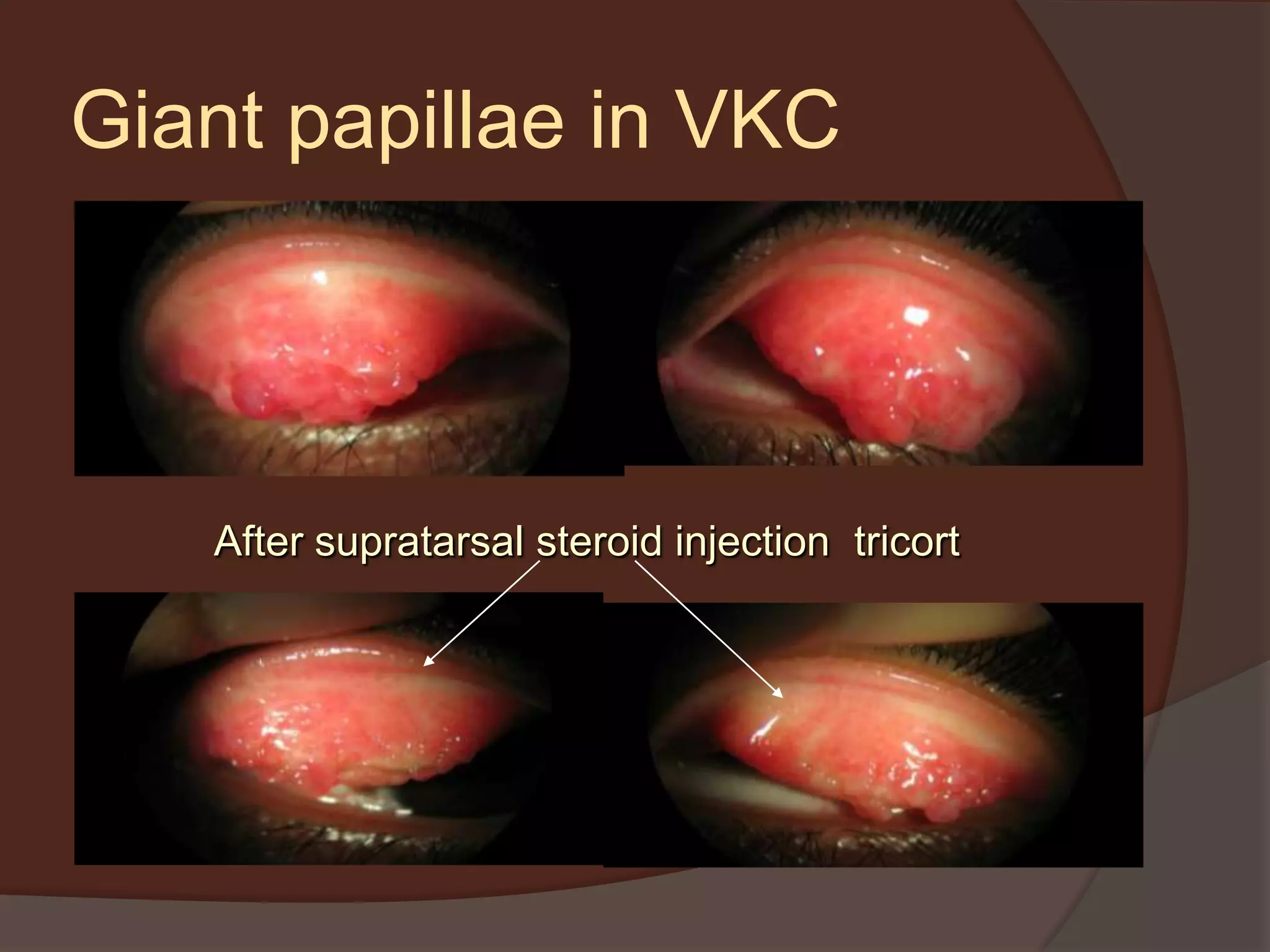
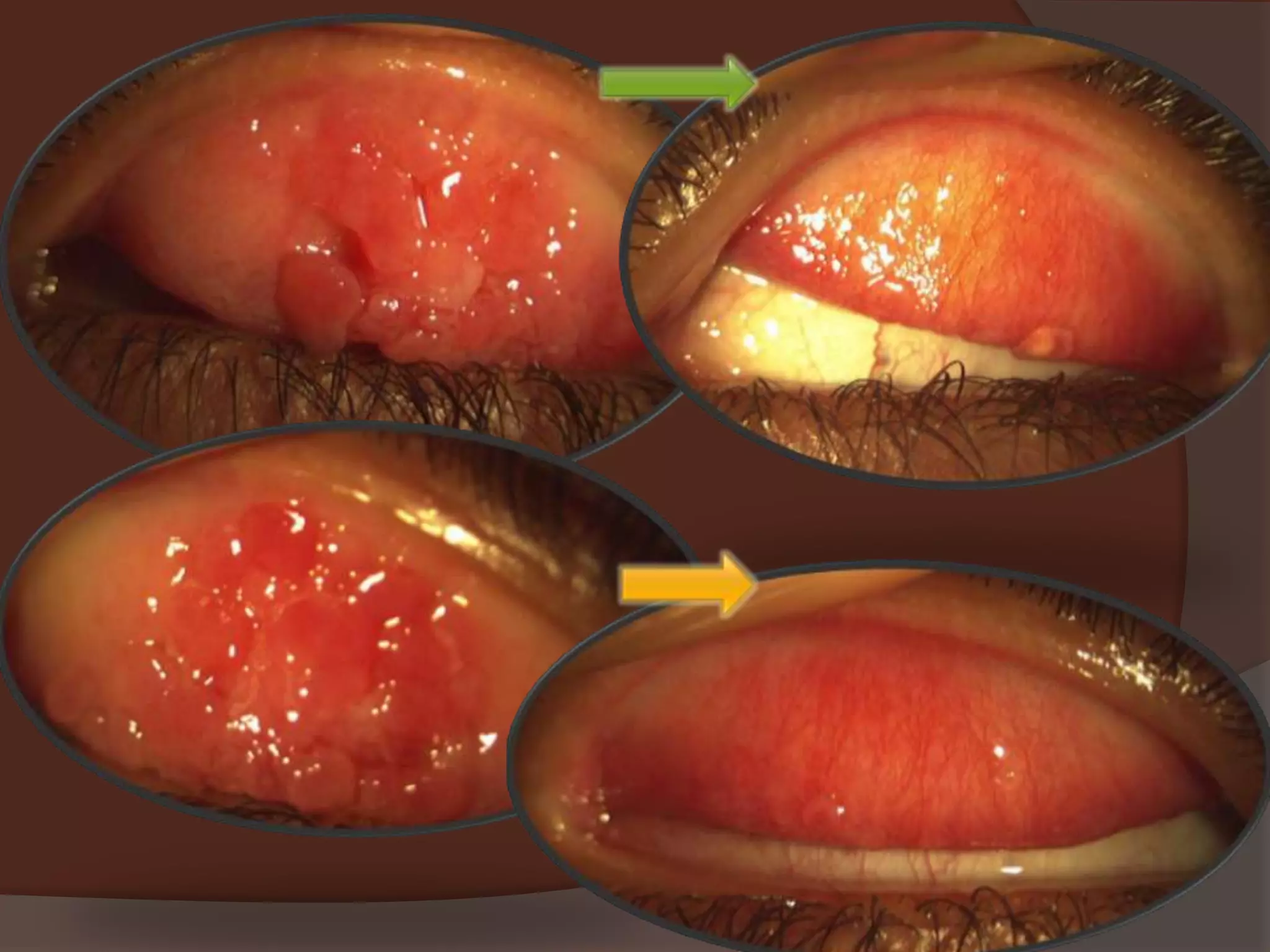
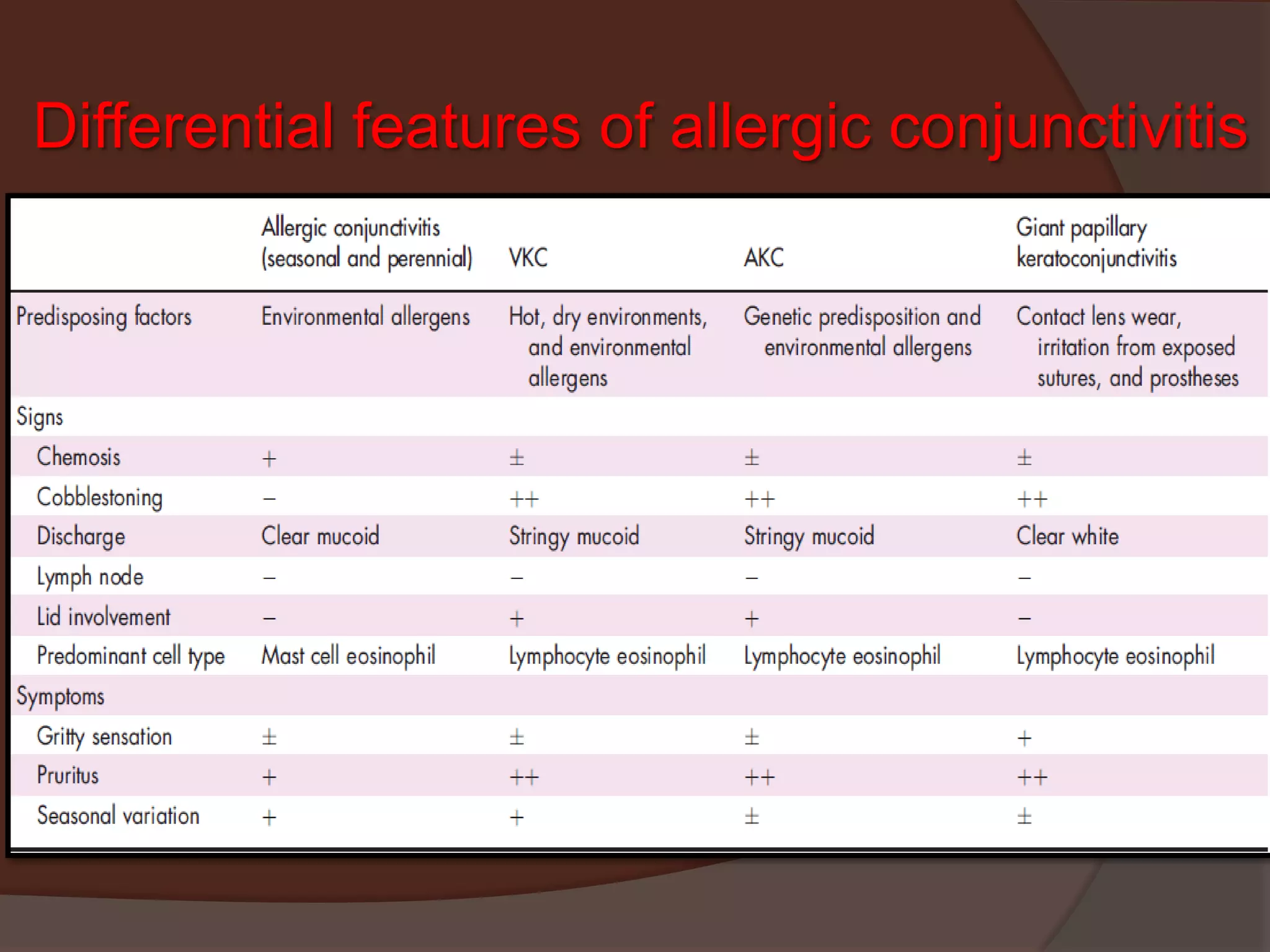
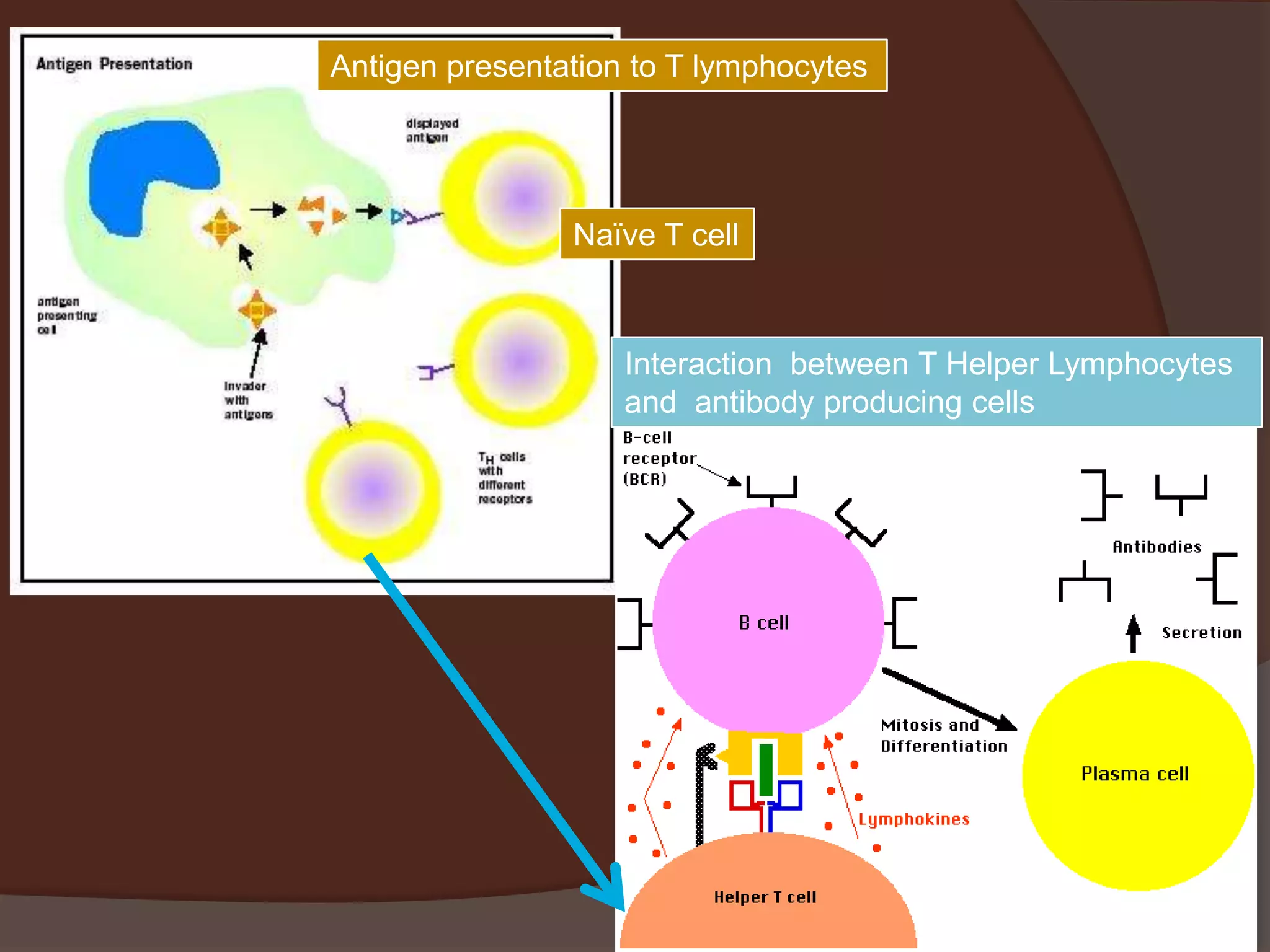
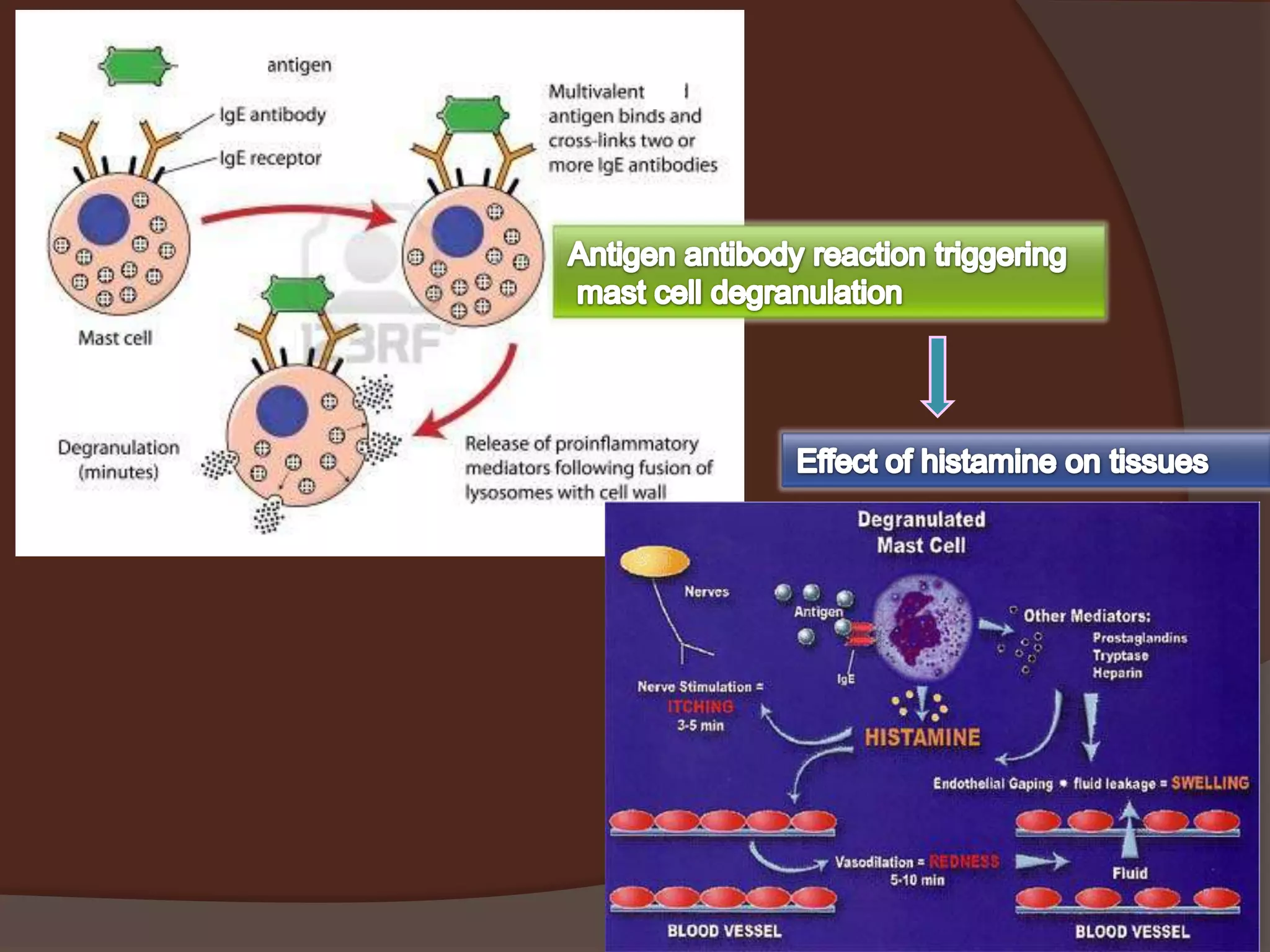
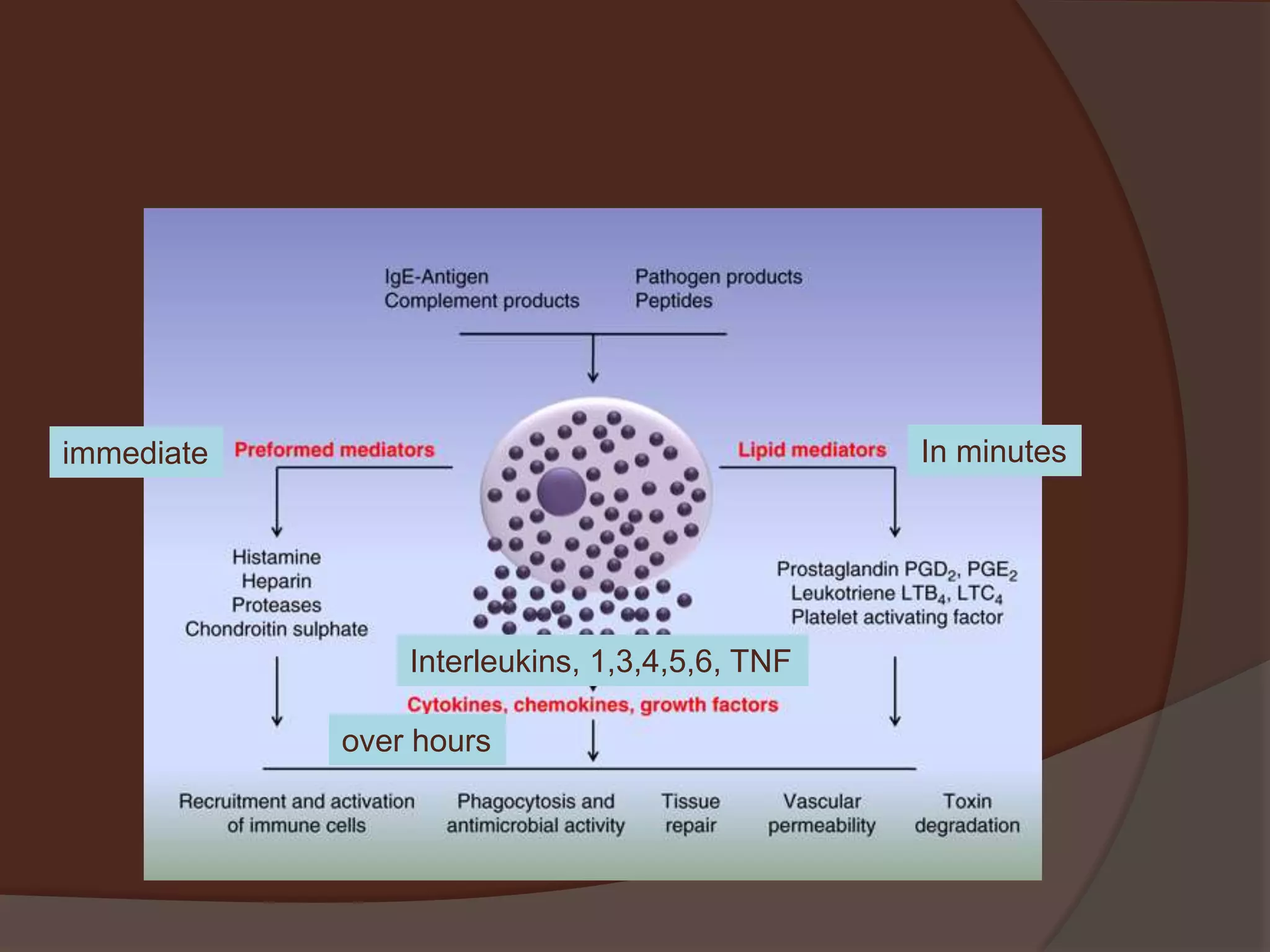
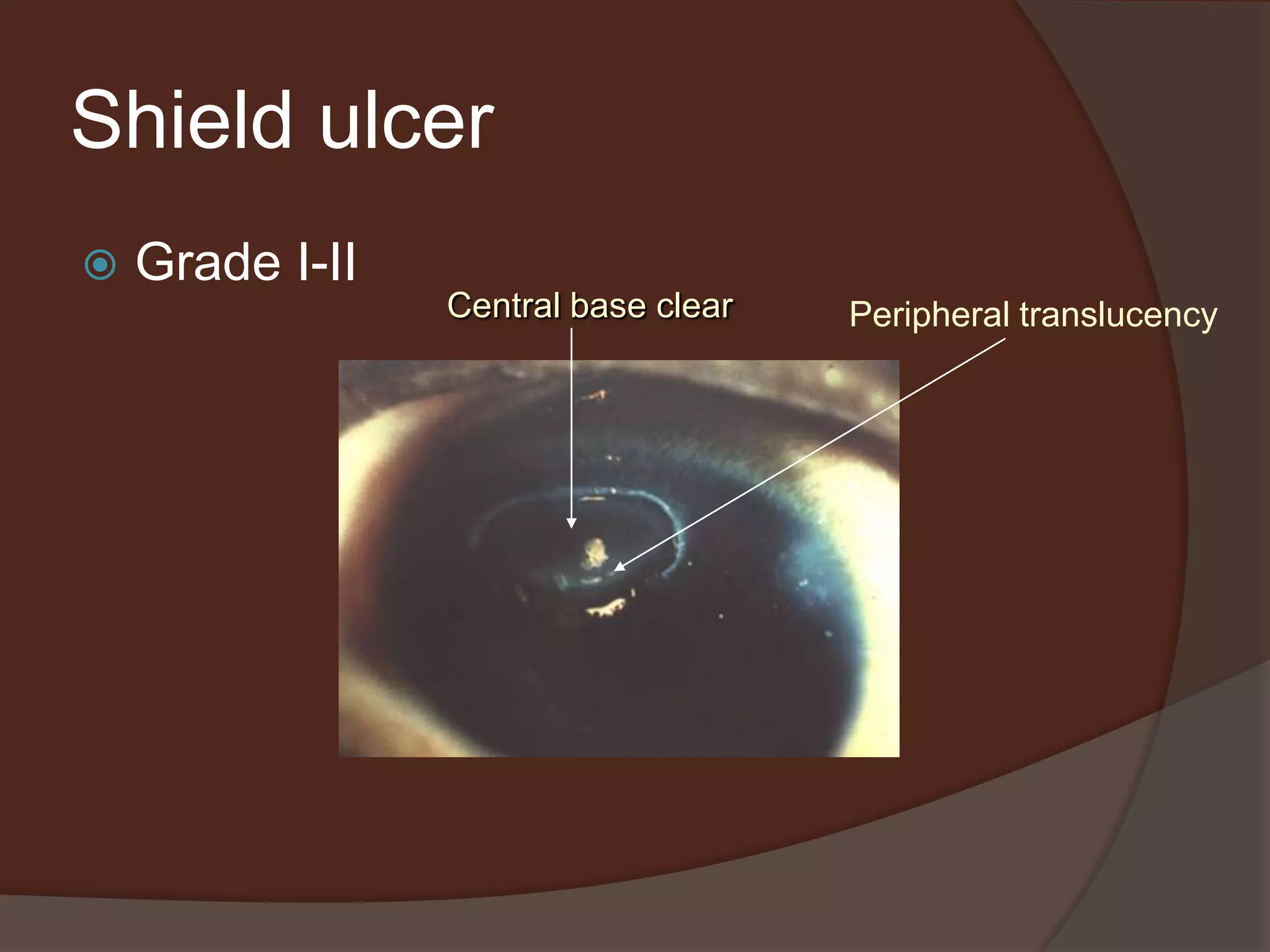
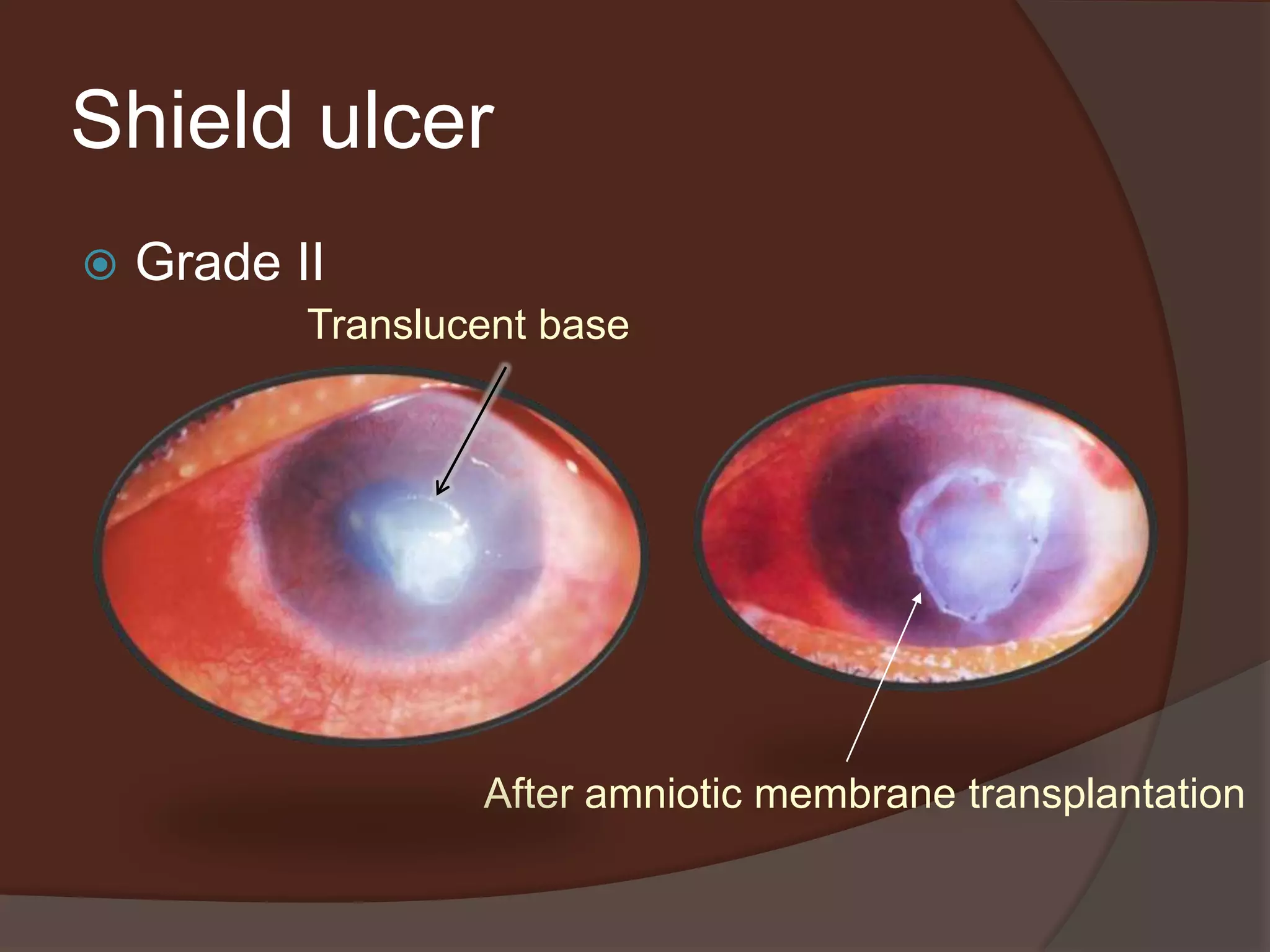
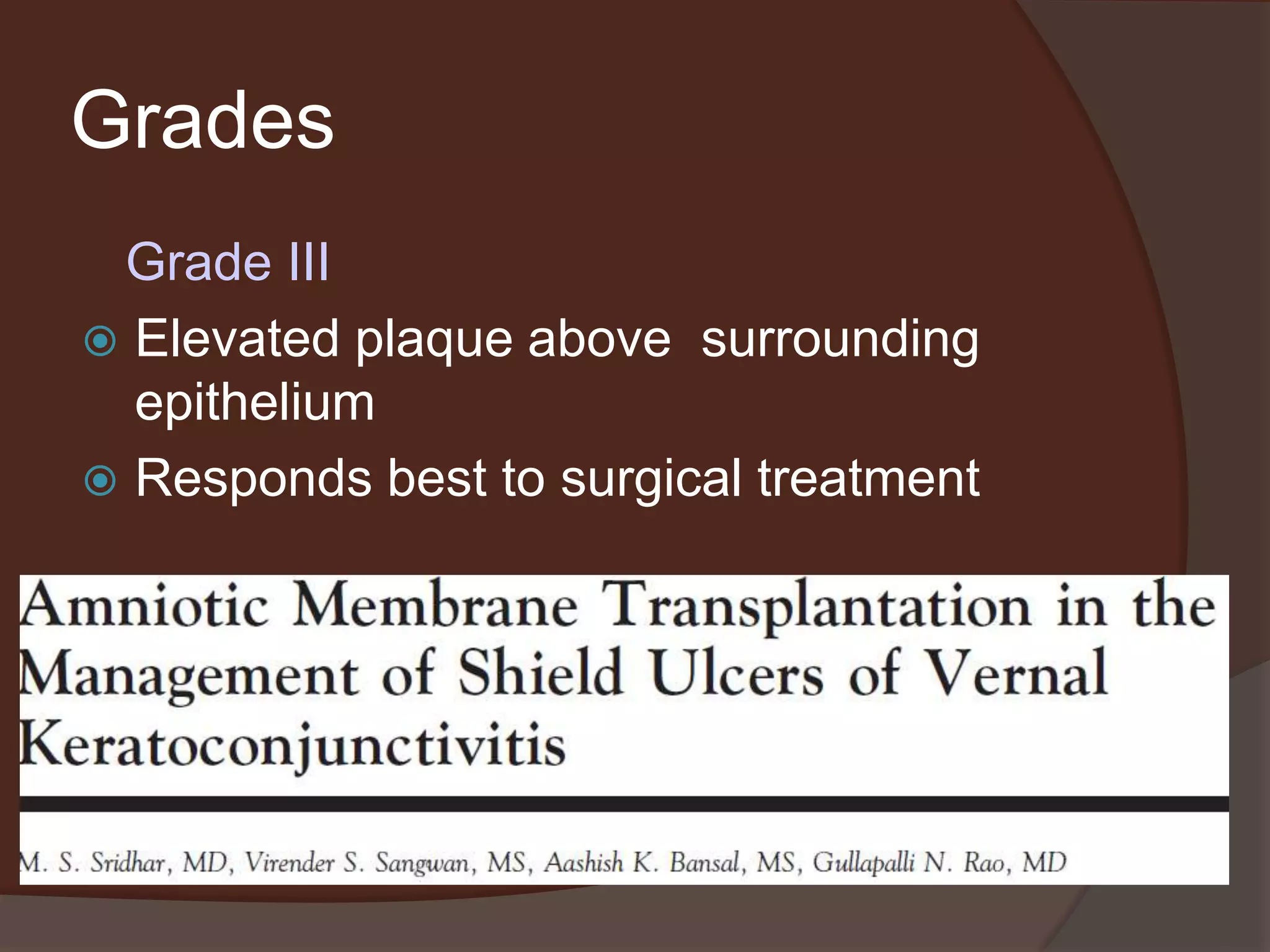
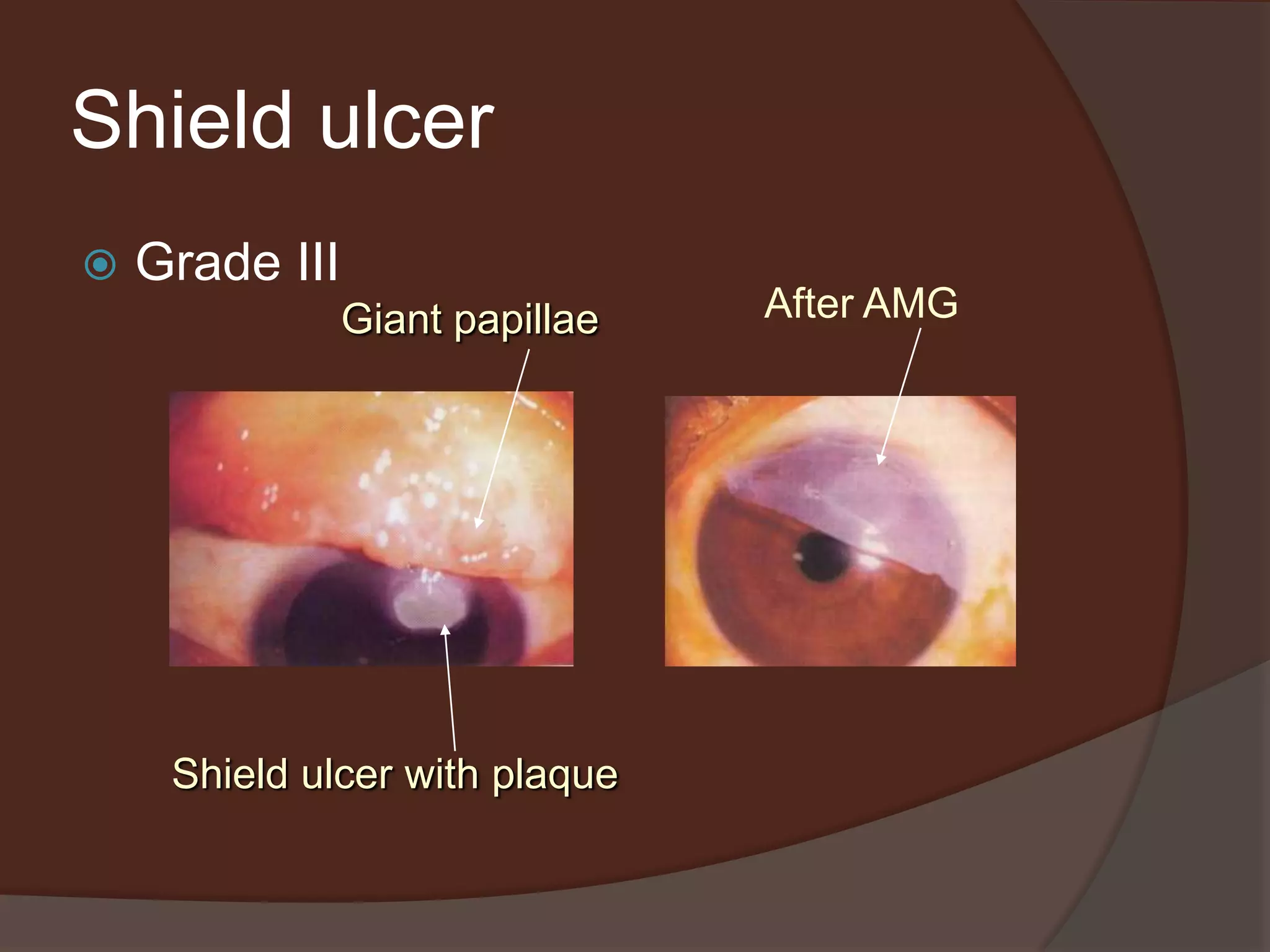
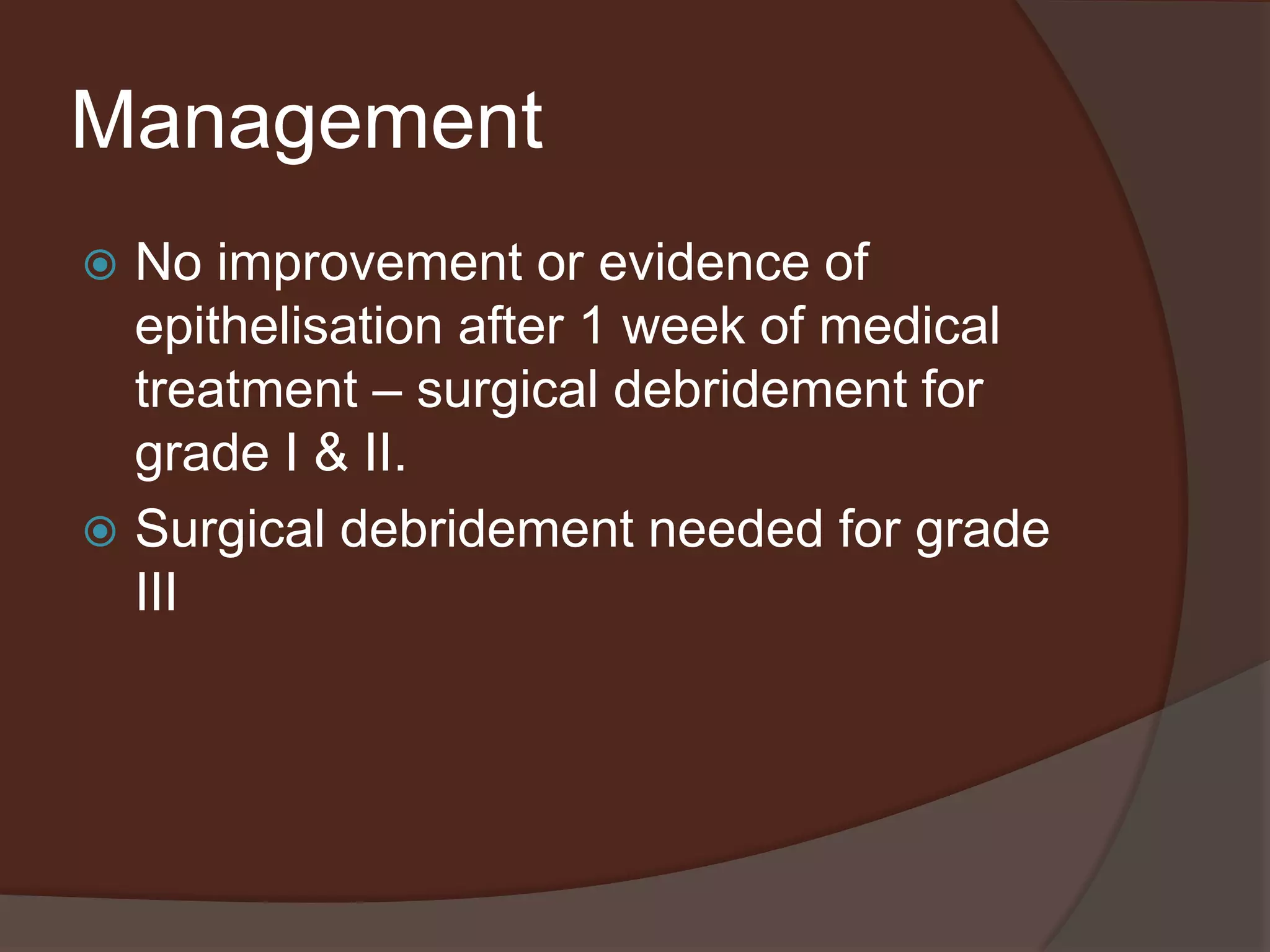
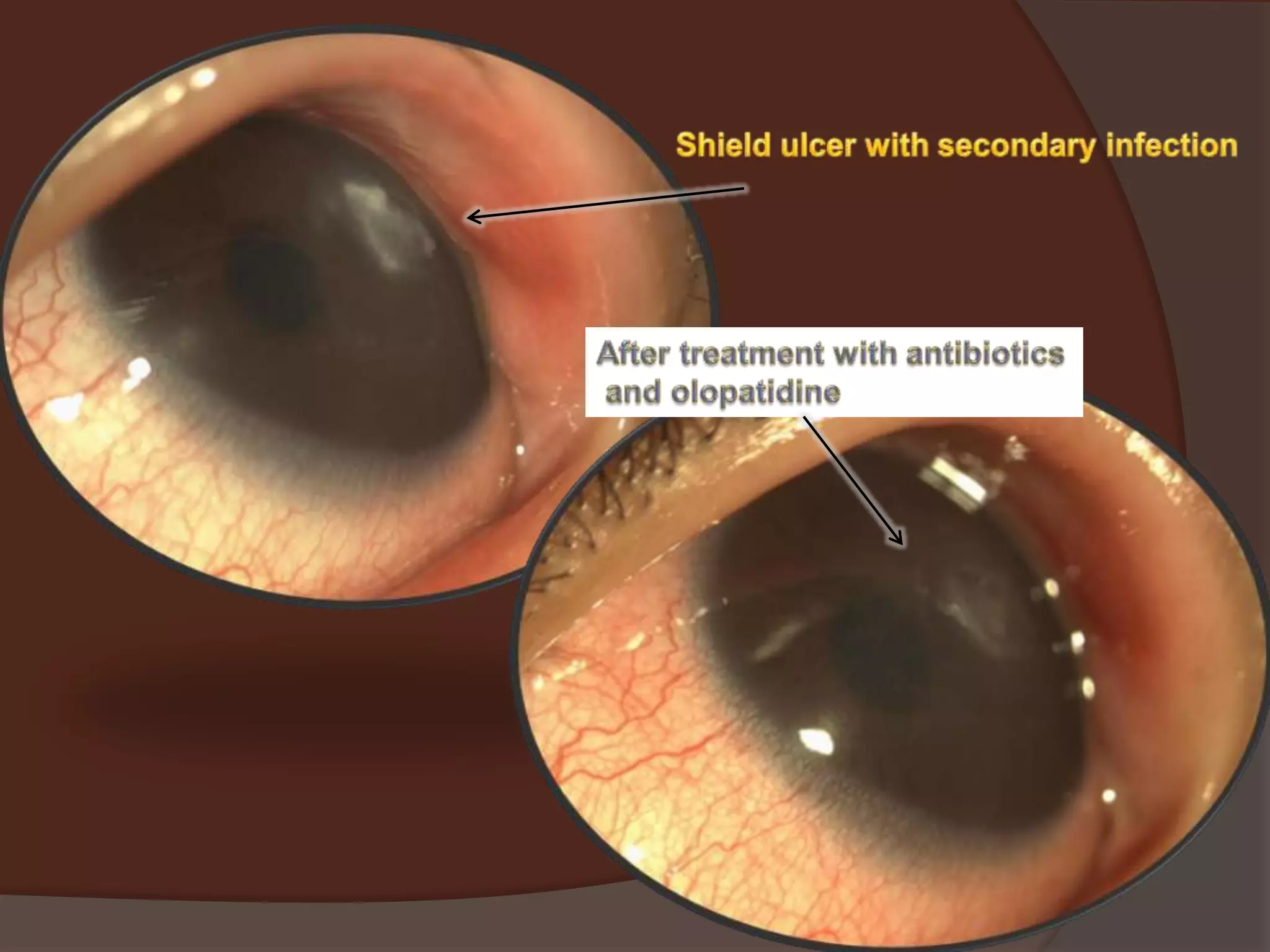
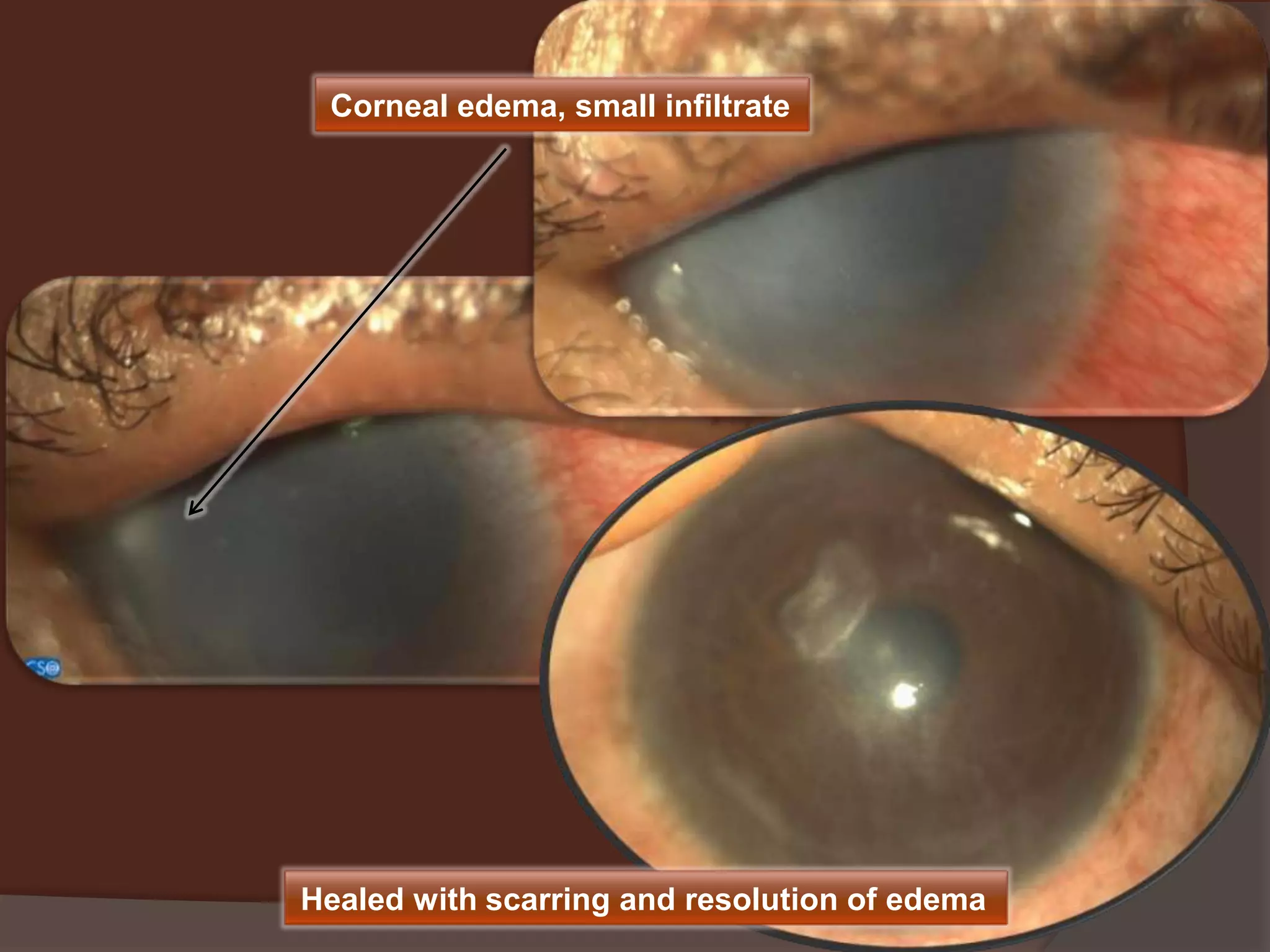
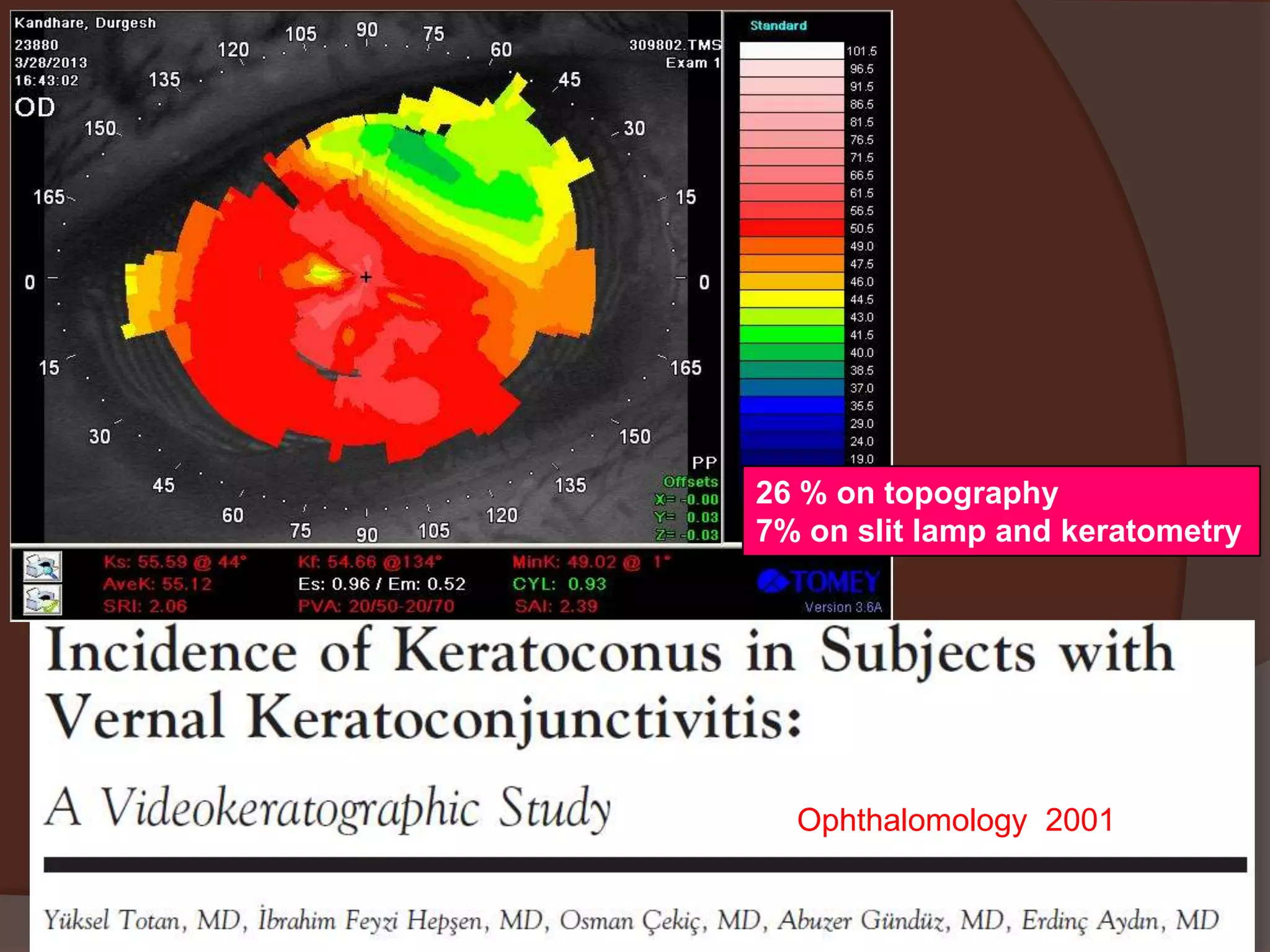
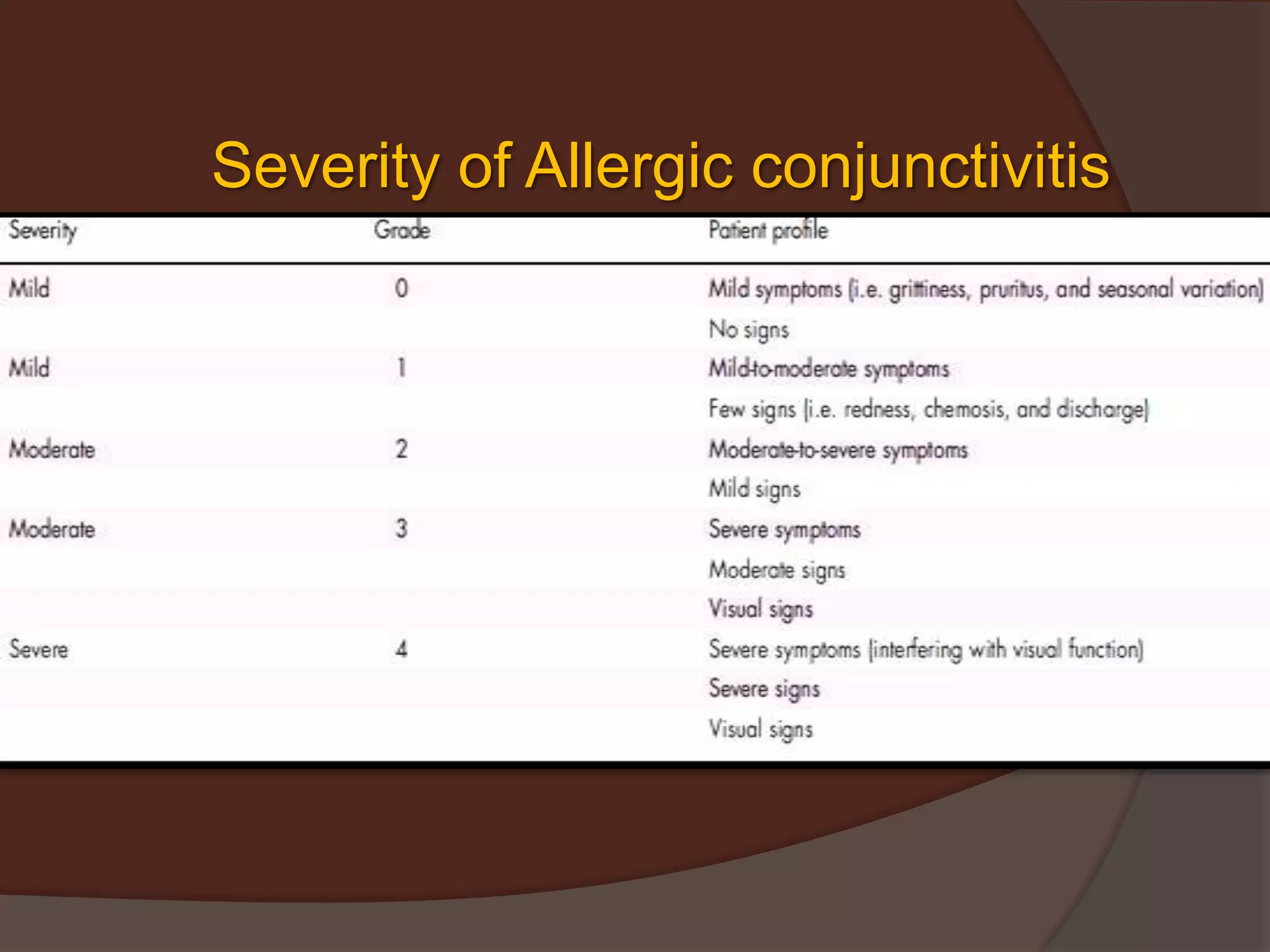
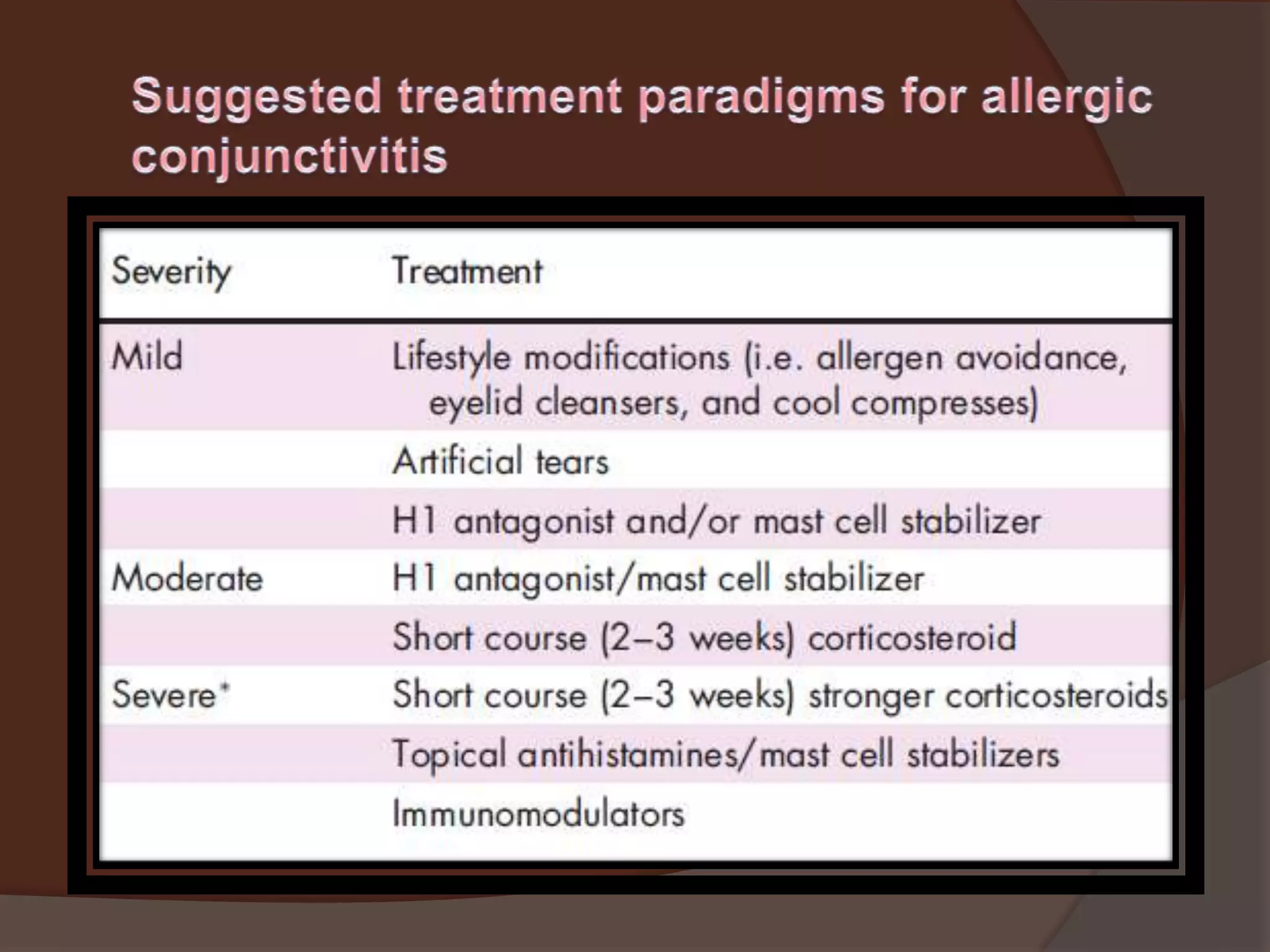
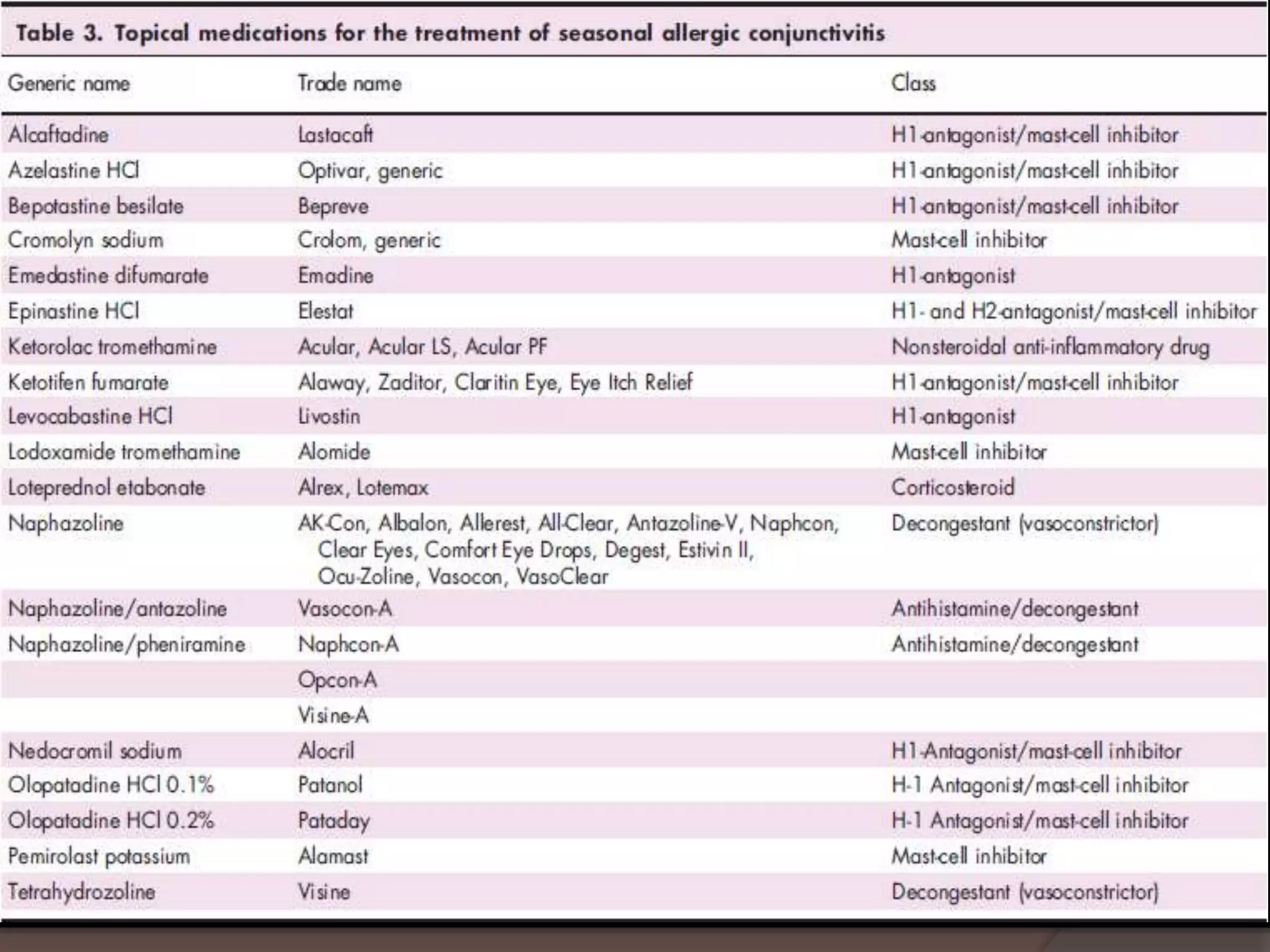
This document discusses allergic conjunctivitis and its subtypes. It describes the signs, symptoms, pathogenesis, differential diagnosis, and management of various forms of allergic conjunctivitis including seasonal allergic conjunctivitis, perennial allergic conjunctivitis, vernal keratoconjunctivitis (VKC), atopic keratoconjunctivitis (AKC), and shield ulcers which can complicate VKC. Treatment options discussed include lifestyle modifications, topical antihistamines, mast cell stabilizers, corticosteroids, cyclosporine, tacrolimus, and sublingual immunotherapy.