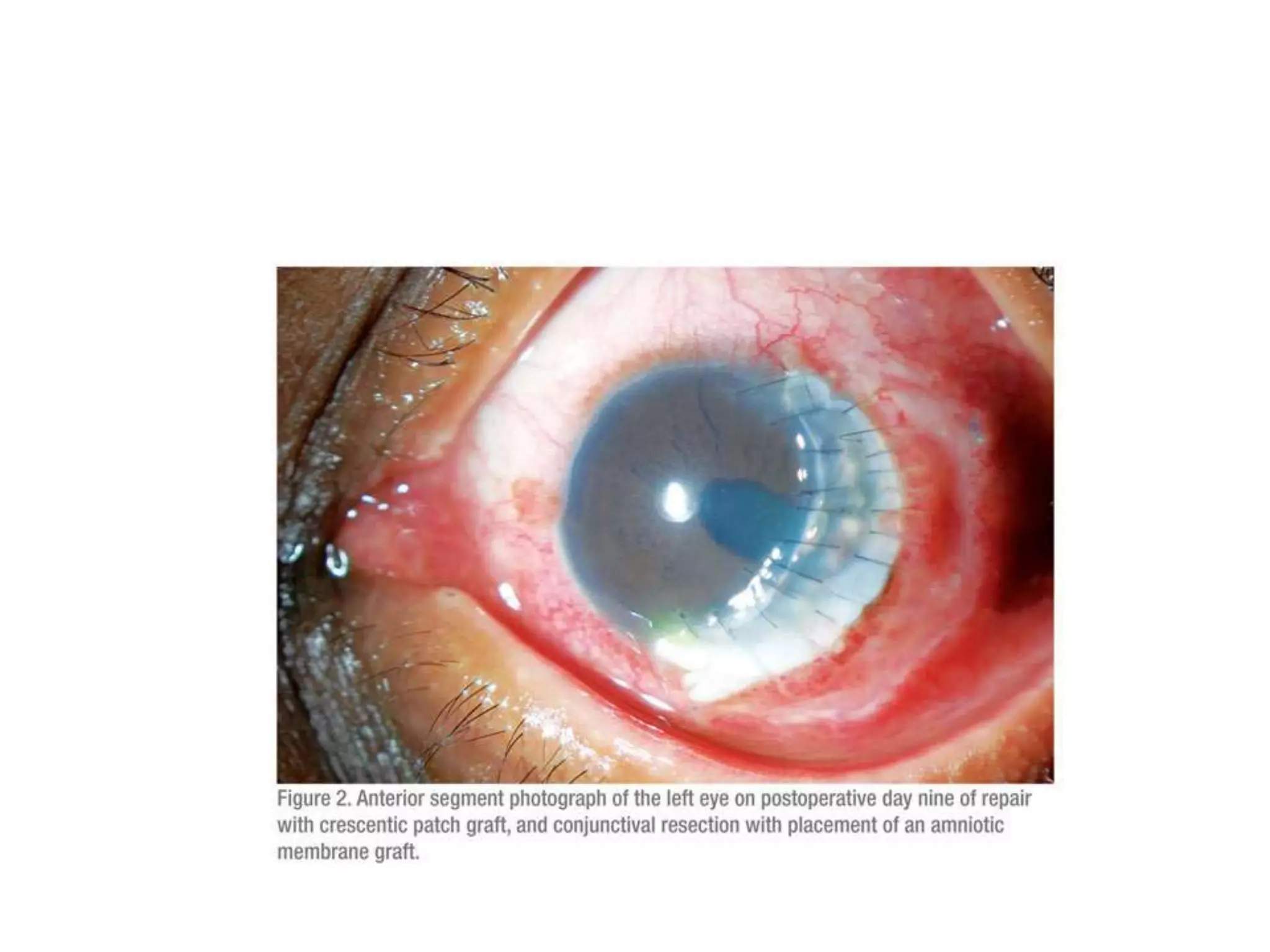
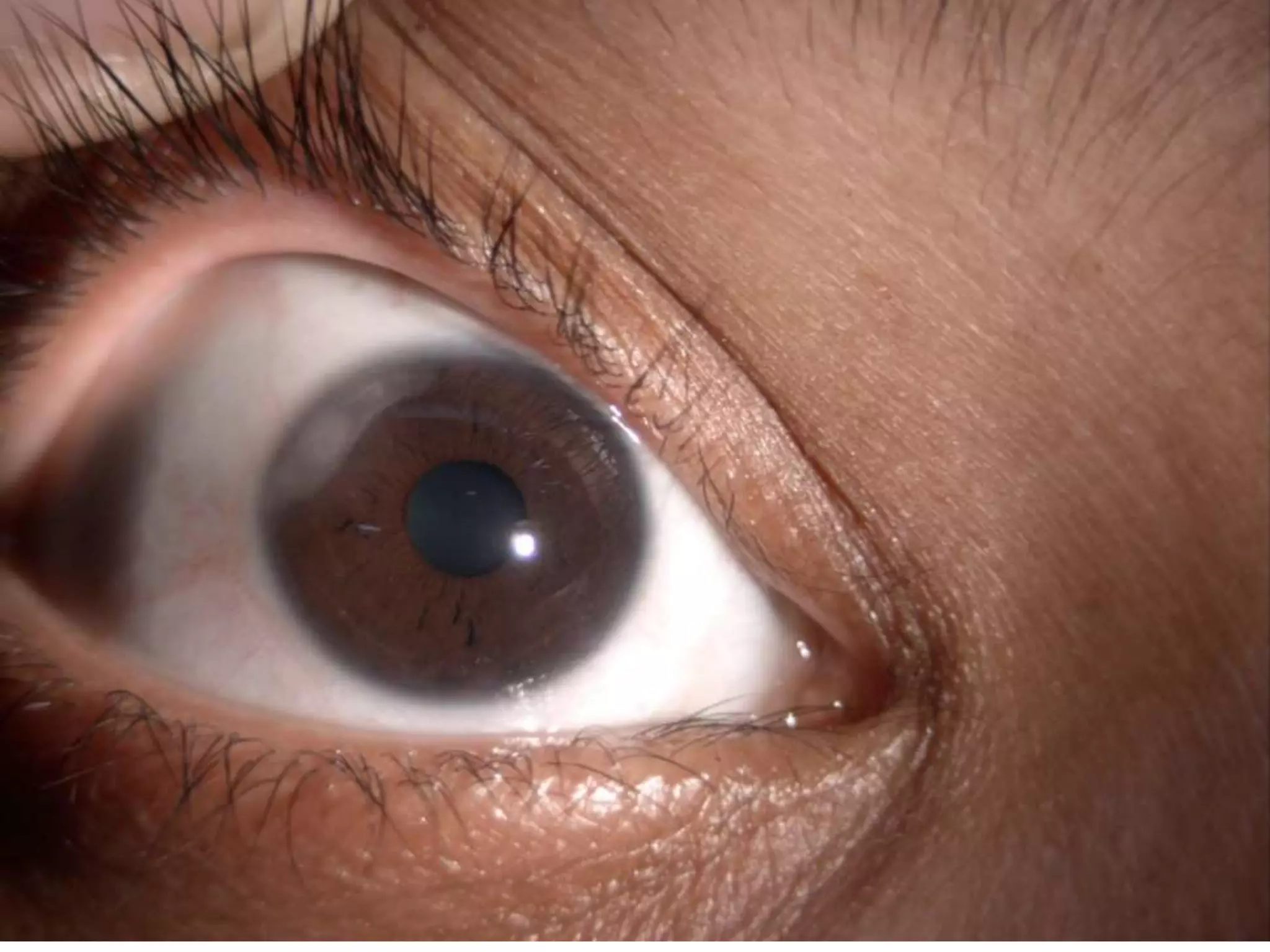
Peripheral ulcerative keratitis is characterized by crescent-shaped inflammation of the corneal stroma, often associated with autoimmune disorders and various ocular conditions. Differential diagnoses include several forms of keratitis and degeneration, while treatment typically involves steroids, immunosuppression, and surgical options such as amniotic membrane grafts. The condition requires careful management due to its association with systemic diseases and potential for severe ocular complications.