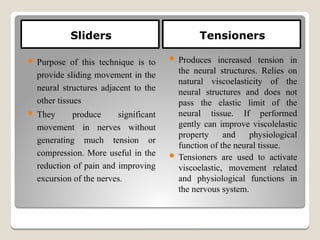
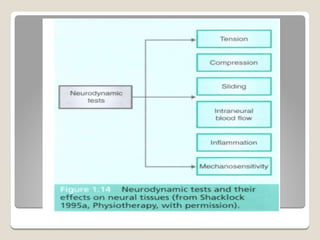
The document outlines neurodynamics, detailing its definitions, principles, and concepts from experts Butler and Shacklock. Key concepts include the relationships between the nervous system’s mechanical and physiological aspects, neurodynamic treatment techniques such as tensioners and sliders, and the mechanics of nerve movement and compression. Additionally, it addresses potential dysfunctions within the neurodynamic system, including mechanical interface dysfunction and neural movement issues.