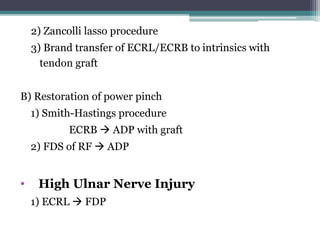
Tendon transfer is a surgical procedure that moves a tendon from one location to another to restore function lost due to nerve damage or injury. The document discusses pre and post-operative physiotherapy management for tendon transfers in the hand. Key points include indications for tendon transfers when nerve recovery is unlikely, prerequisites like full range of motion, and post-operative goals like protecting the transferred tendon and regaining range of motion. Specific procedures are described to address radial, ulnar and median nerve palsies. Post-operative splinting and rehabilitation protocols aim to protect the transfer initially and progress to strengthening.