Some key points include:
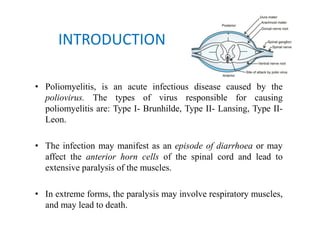
- Polio is caused by infection with the poliovirus and can lead to paralysis of muscles.
- It spreads via the fecal-oral or respiratory routes and infects the anterior horn cells of the spinal cord.
- Clinical features may include fever, neck rigidity, asymmetric limb paralysis that often affects the legs. Respiratory muscles can be involved.
- Treatment focuses on supportive care, splinting to prevent deformities, physiotherapy to