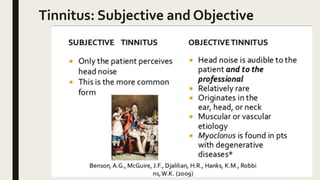
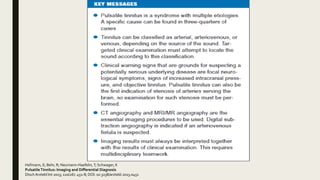
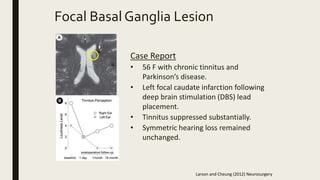
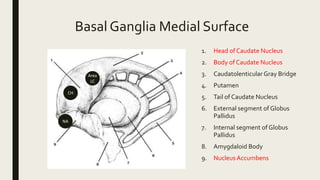
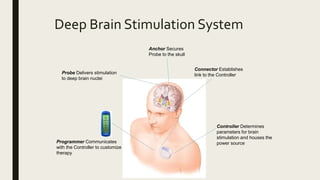
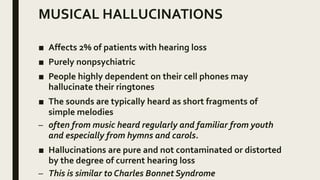
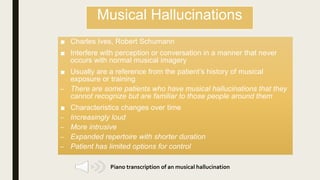
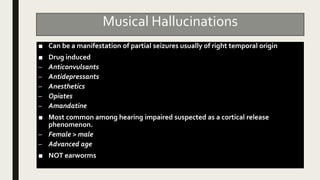
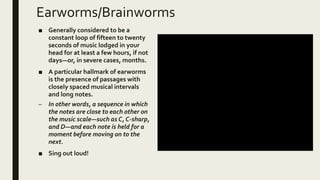
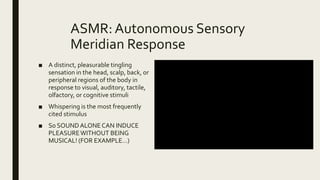
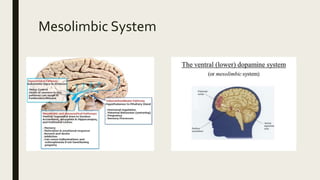
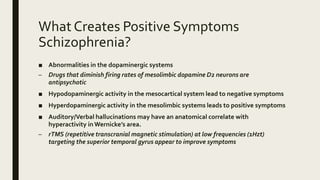
The document discusses various auditory phenomena, including tinnitus, musical hallucinations, and auditory hallucinations associated with schizophrenia. It highlights the neurological origins and pathophysiology of these conditions, as well as potential treatments like deep brain stimulation and transcranial magnetic stimulation. Additionally, it addresses the prevalence and characteristics of these auditory experiences, emphasizing their impact on patients' lives.


![Episodic Cranial Sensory Shock
(“Exploding Head Syndrome)
■ Benign condition in which a person hears loud "imagined" noises (such as a bomb
exploding, a gunshot, or a cymbal crash) or experiences an explosive feelingwhen
falling asleep or waking up.[
■ The most prevalent theory on the cause of EHS is dysfunction of the reticular
formation in the brainstem responsible for transition between waking and
sleeping.[2]
■ Paroxysmal sensory parasomnia not associated with significant pain.
■ Consider hypnagogic hallucinations and sleep paralysis as other parasomnias that
occur at the onset of sleep and before awakening
■ Treatment has included Anafanil, carbamazepine, methyphenidate. Reassurance
may be best approach.](https://image.slidesharecdn.com/auditoryhallucinations121017-180105205010/85/Auditory-Hallucinations-27-320.jpg)