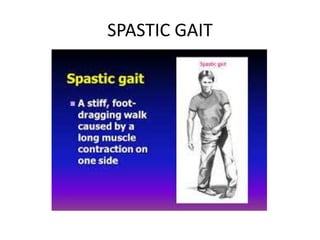
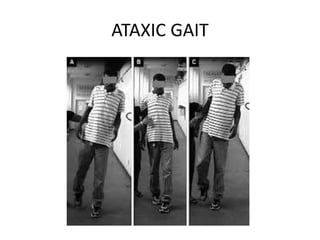
This document describes different types of gait disorders including spastic, ataxic, parkinsonian, dyskinetic, tabetic, paretice, and painful gait. Each type is defined by its localization in the nervous system, description of abnormalities, and common causes. Spastic gait is caused by upper motor neuron lesions and involves stiff-legged walking. Ataxic gait results from cerebellar lesions and is wide-based and staggering. Parkinsonian gait is caused by basal ganglia dysfunction and appears slow and shuffling.