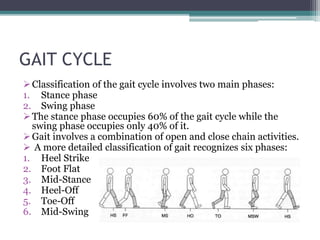
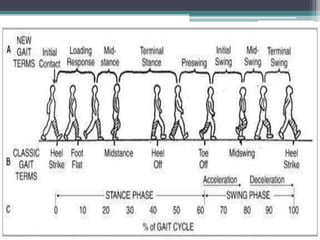
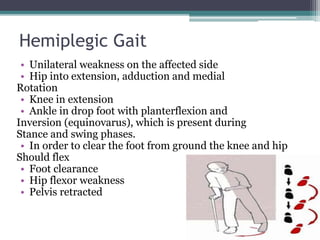
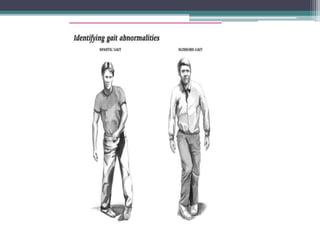
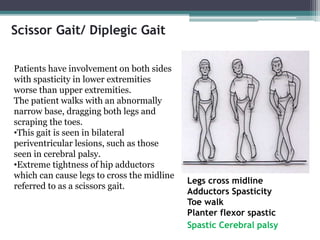
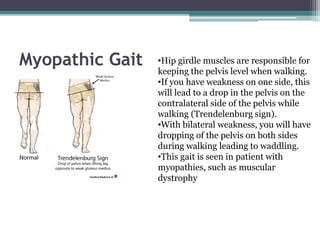
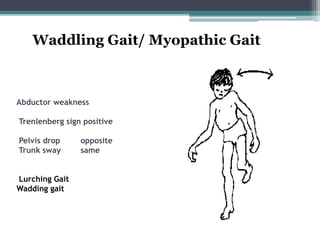
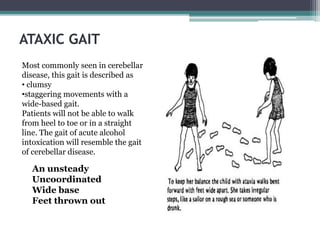
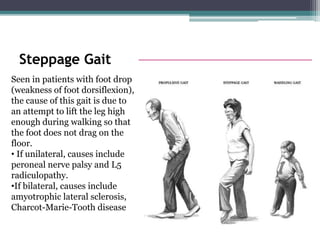
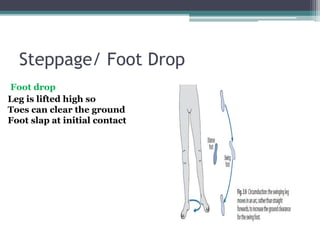
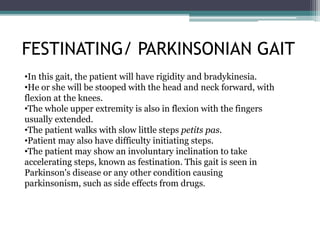
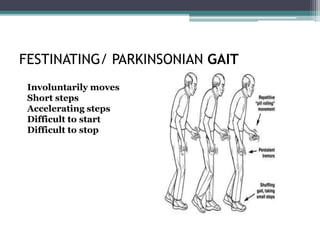
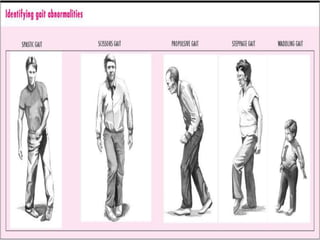
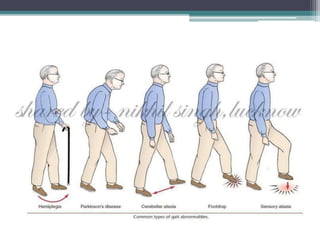
The document discusses various types of abnormal gaits seen in different medical conditions. It begins by defining the normal gait cycle and its phases. It then describes common causes of abnormal gaits including pain, joint/muscle limitations, weakness, and neurological involvement. Specific gaits are then outlined, including hemiplegic gait seen in stroke, scissor gait in cerebral palsy, myopathic gait in muscular diseases, steppage gait in foot drop conditions, Parkinsonian gait, and sensory gait related to proprioceptive loss.