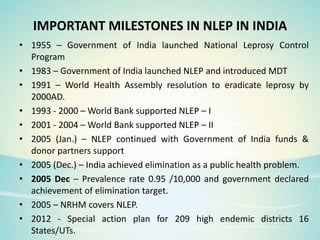
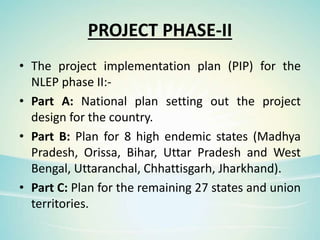
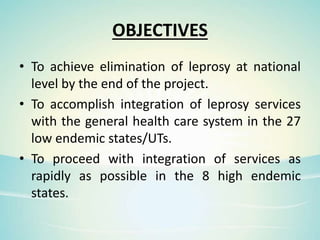
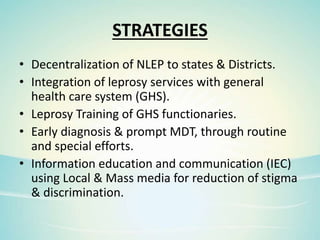
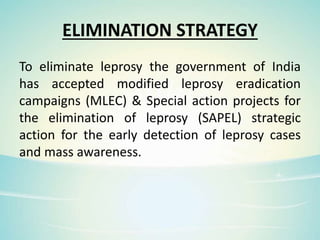
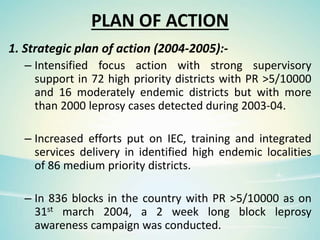
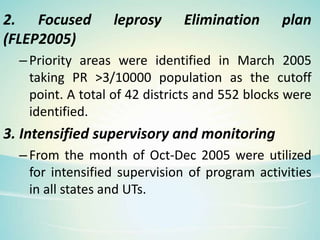
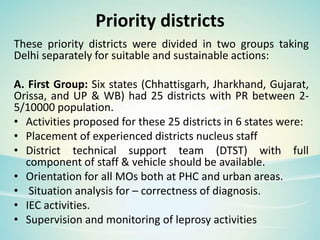
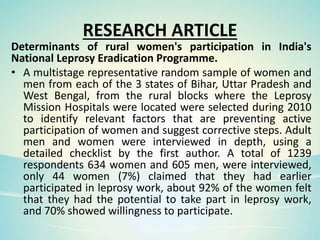
This document summarizes leprosy, including its causes, symptoms, history, classification, treatment, and the national leprosy eradication program in India. It discusses how leprosy is caused by Mycobacterium leprae, affects the skin and nerves, and was recognized in ancient civilizations. Multidrug therapy provided through the WHO has largely cured the 16 million cases treated over 20 years. The national program in India focuses on case detection, treatment, prevention, and social stigma reduction through various strategies including modified leprosy campaigns and special action projects.