This document discusses disease transmission and infection control. It covers the following key points:
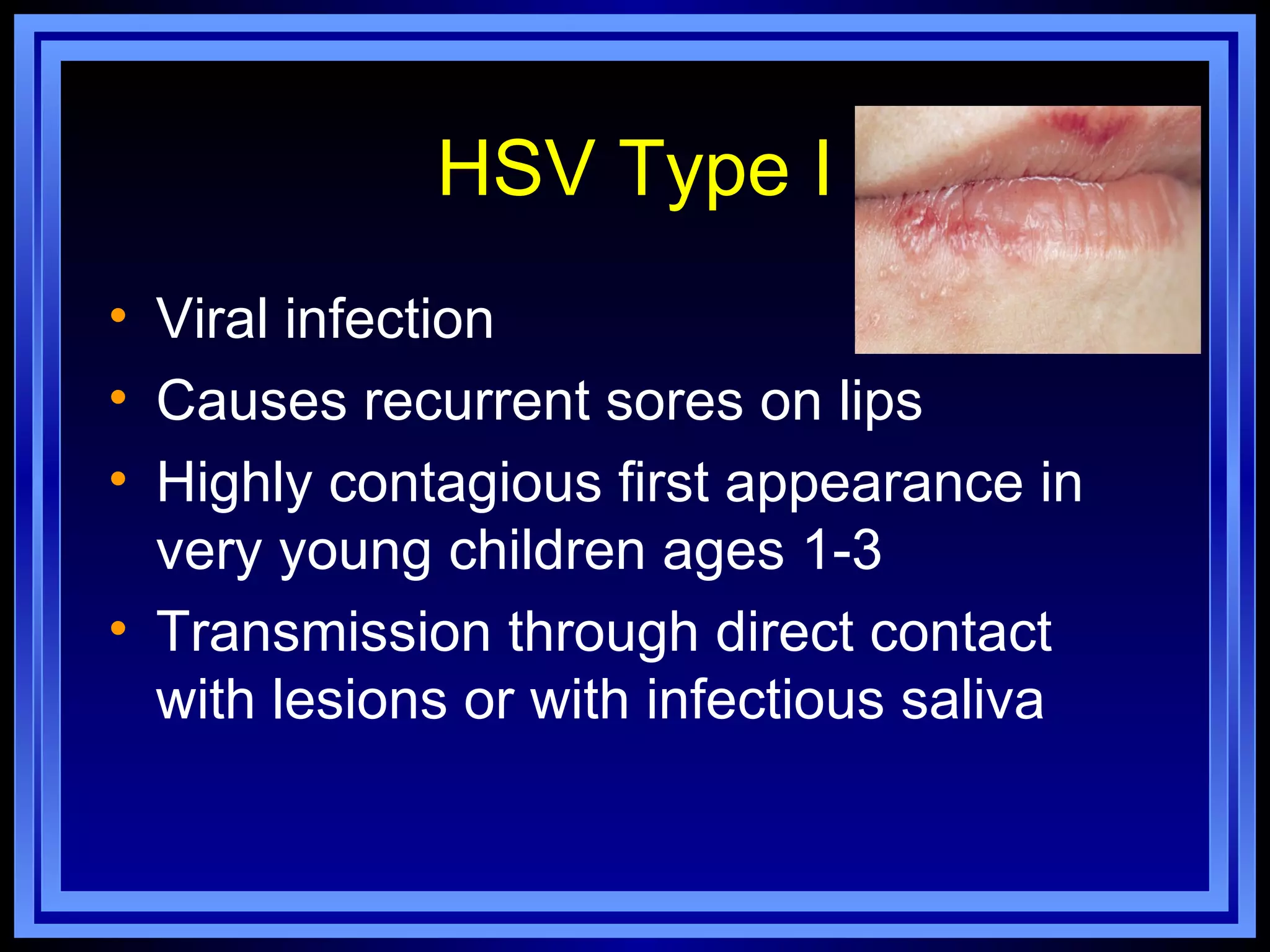
1. Microorganisms like bacteria, viruses, fungi and protozoa can cause illness in humans. The chain of infection requires a microorganism, a mode of transmission to a susceptible host, and a portal of entry.
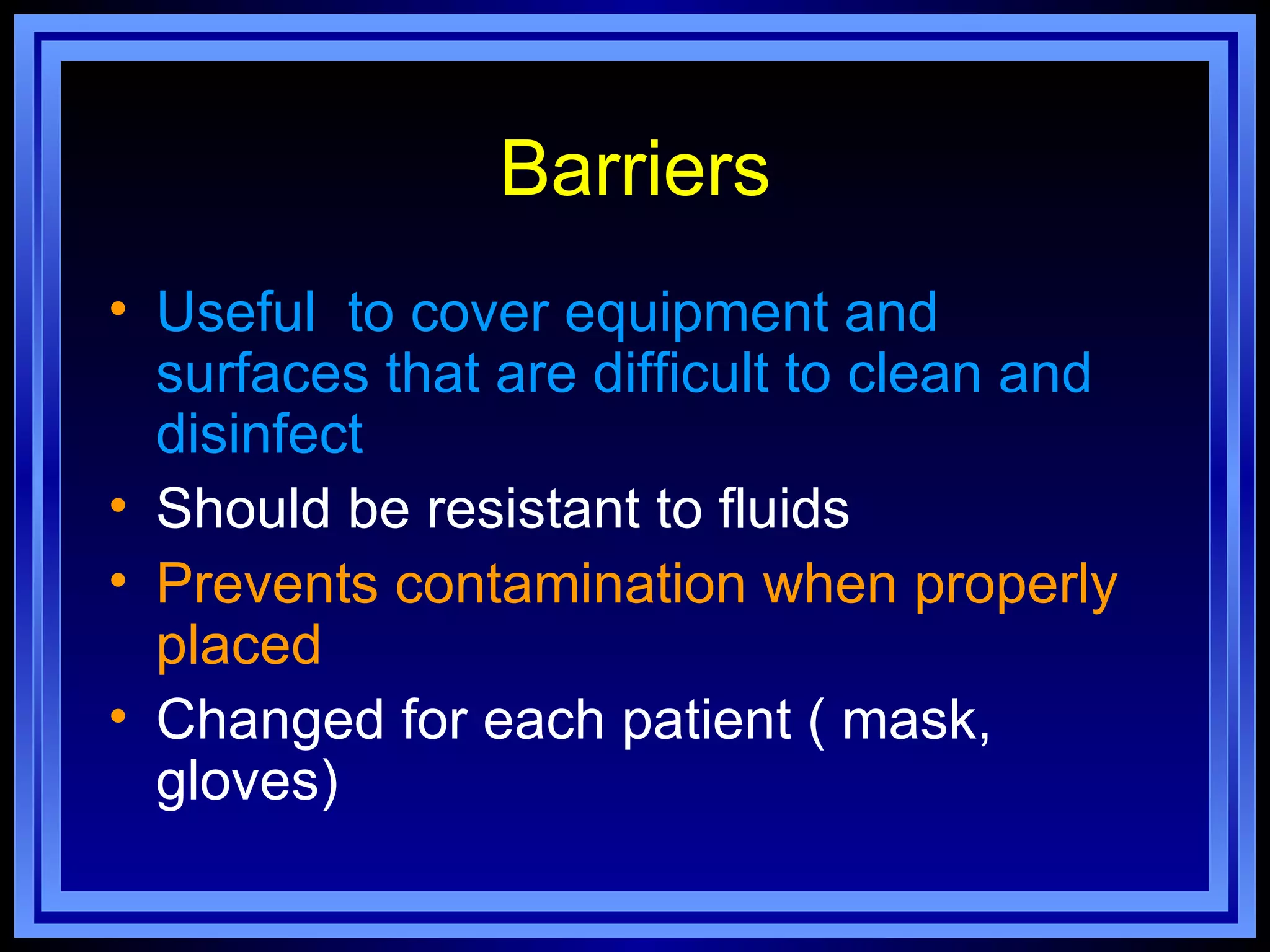
2. Common modes of disease transmission include airborne via aerosols or droplets, direct contact, fecal-oral, and blood or body fluids. Standard precautions like hand hygiene and barriers are used to prevent transmission.
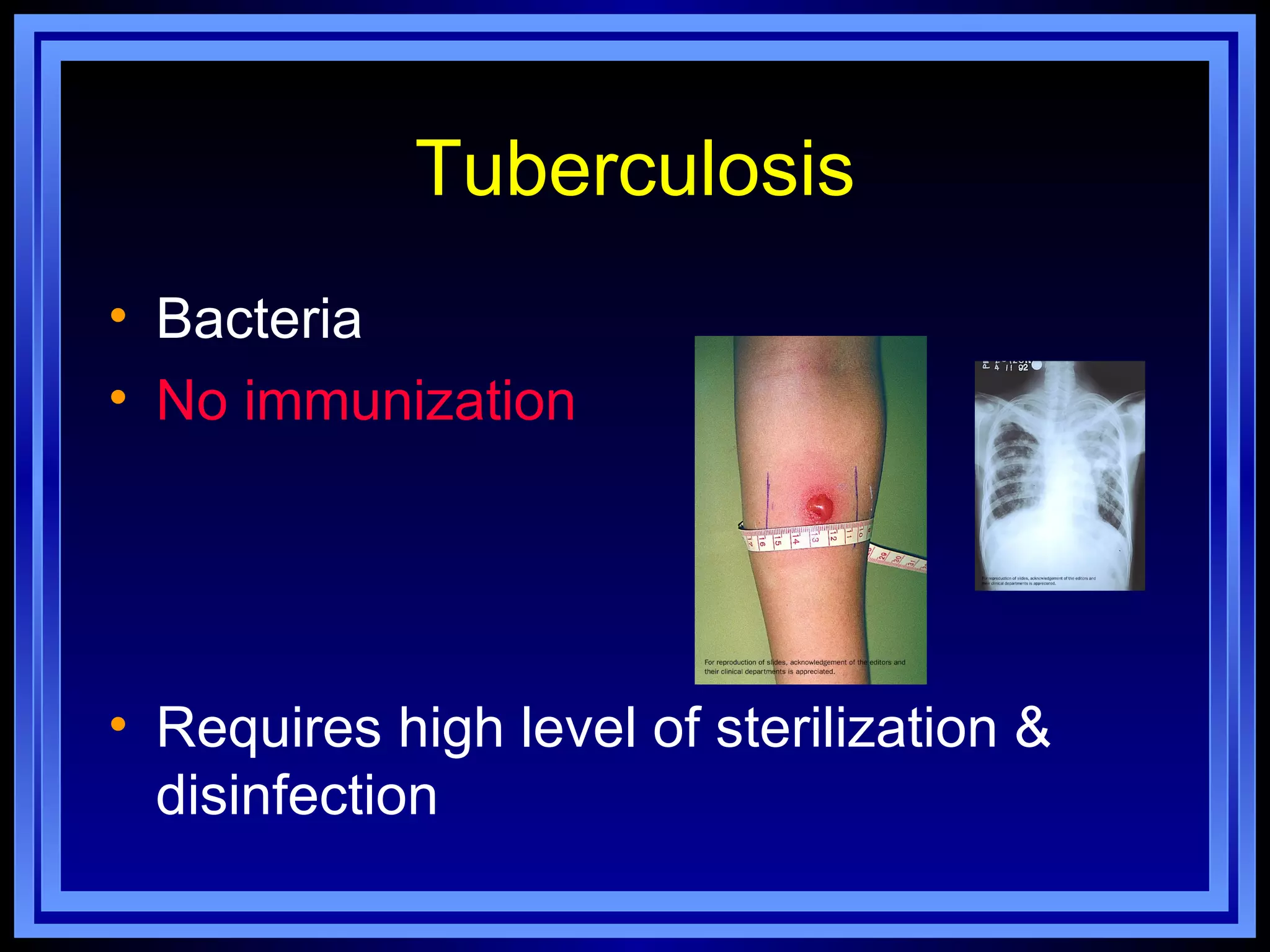
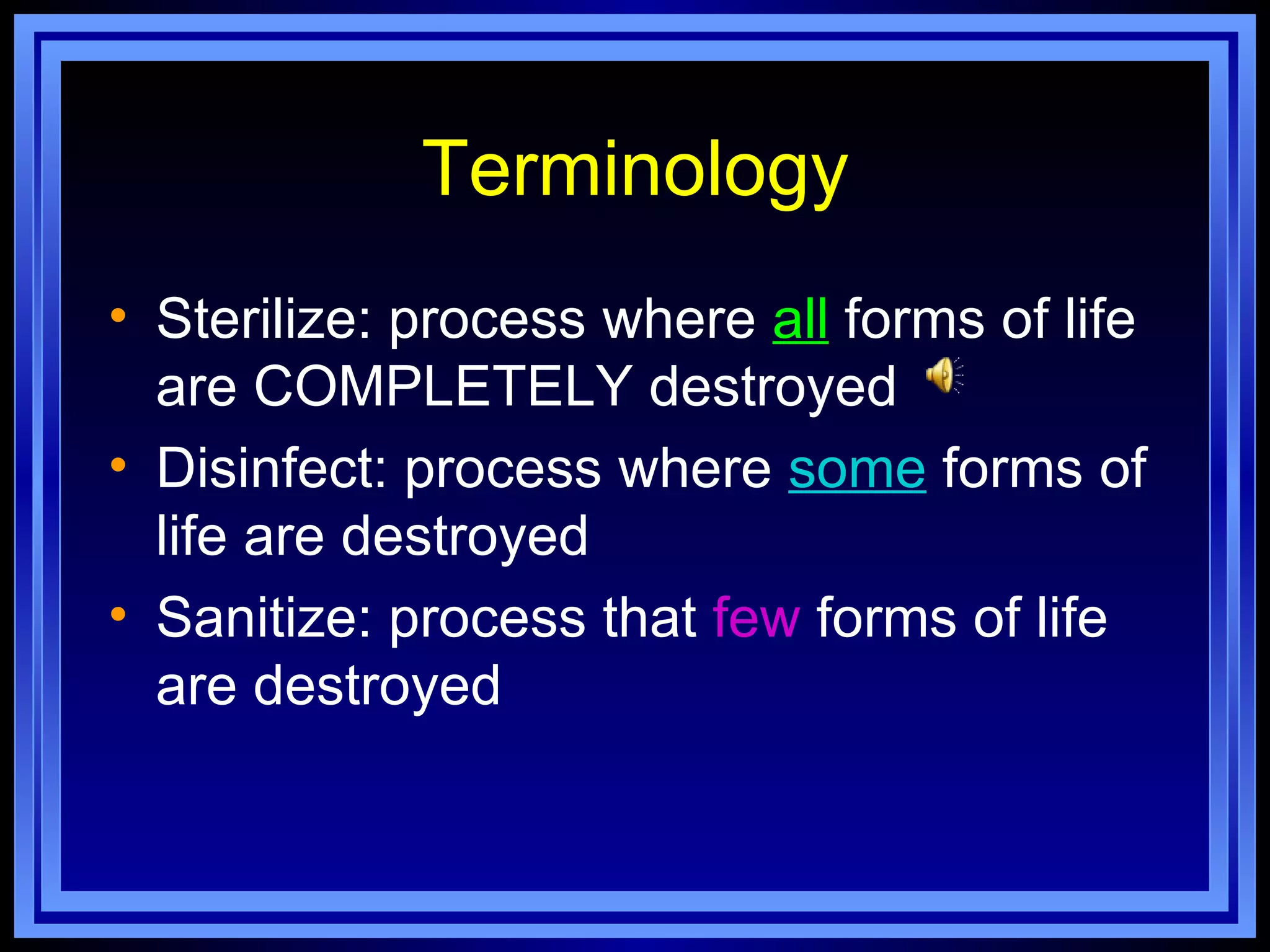
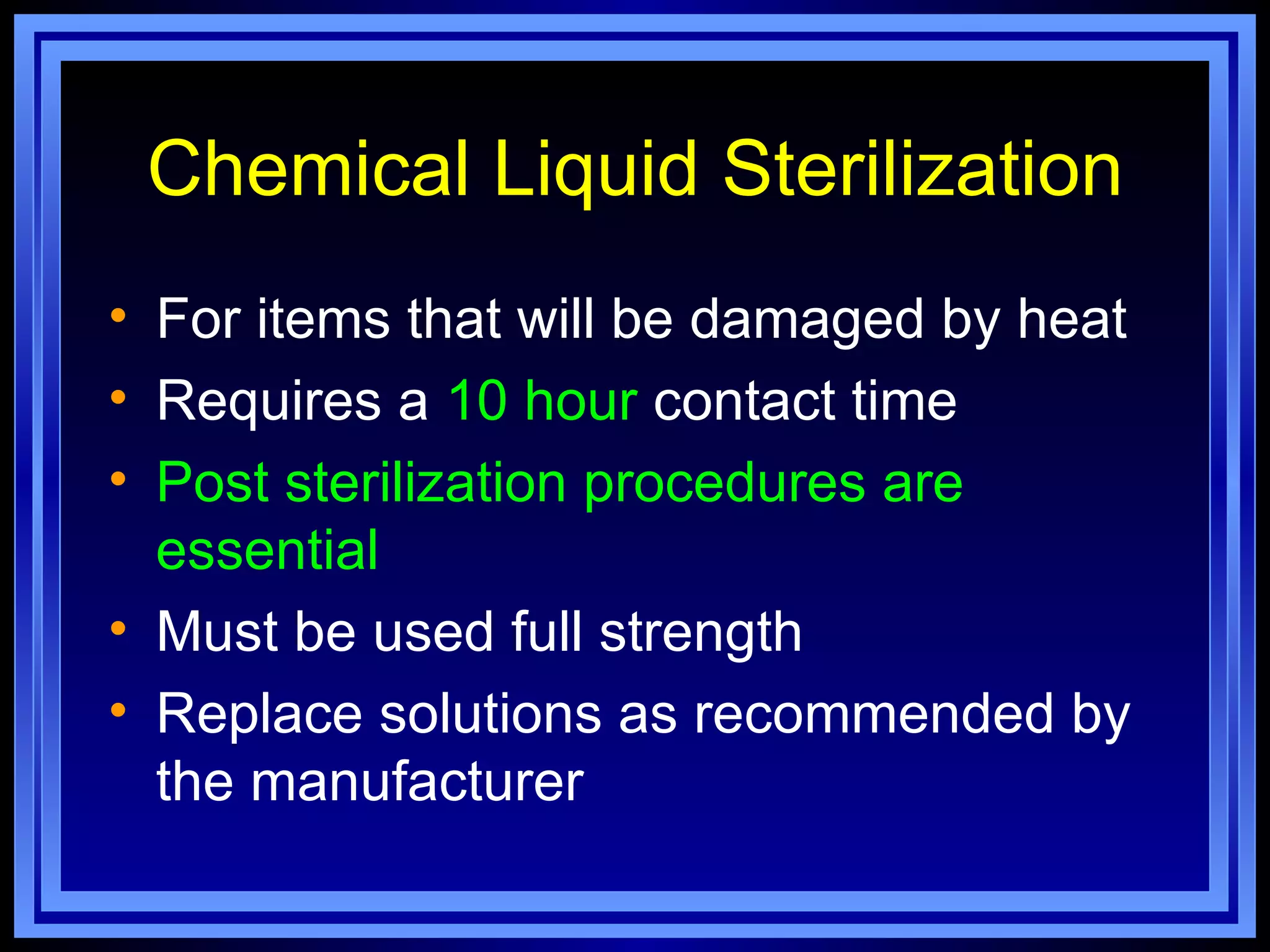
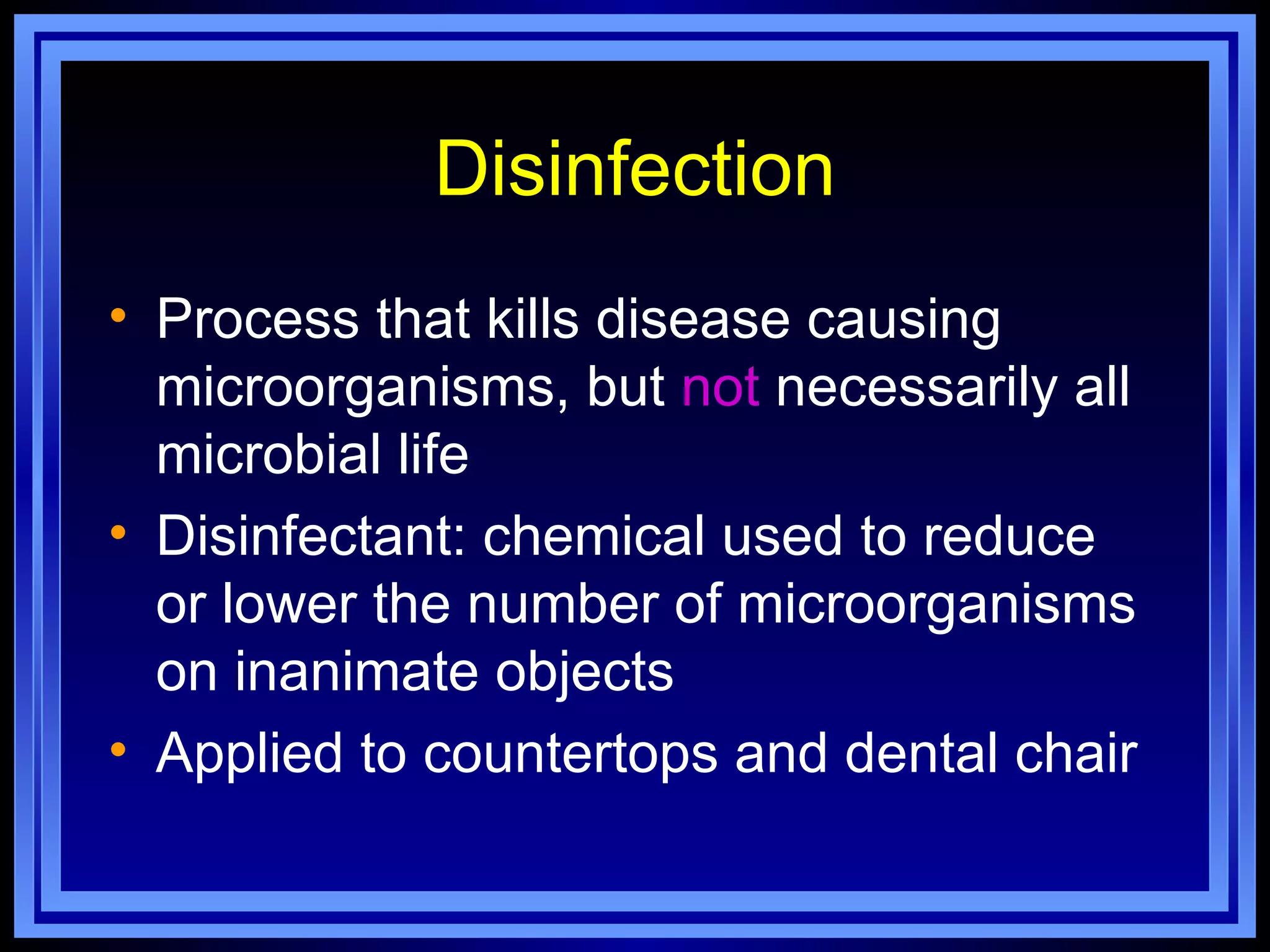
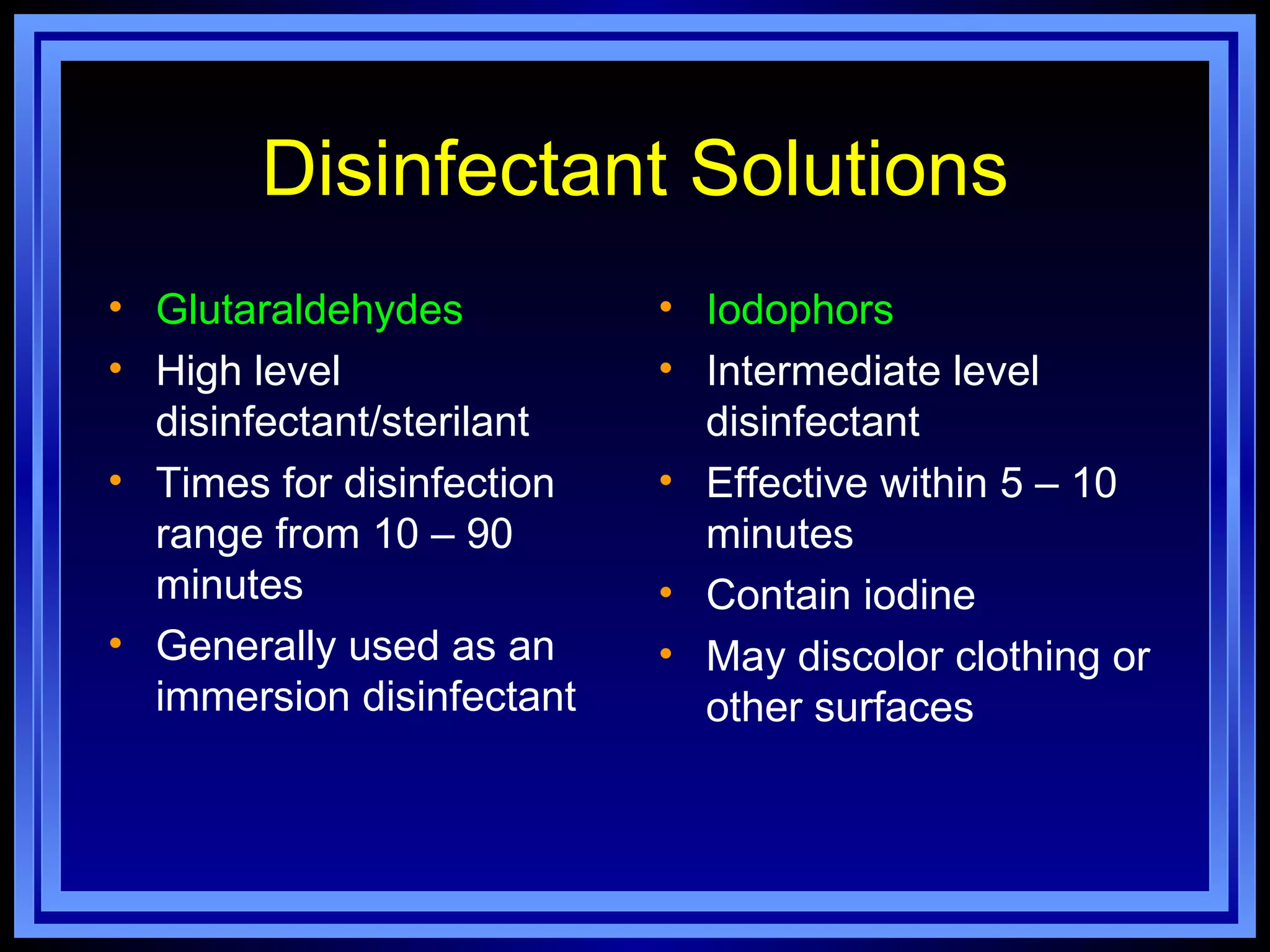
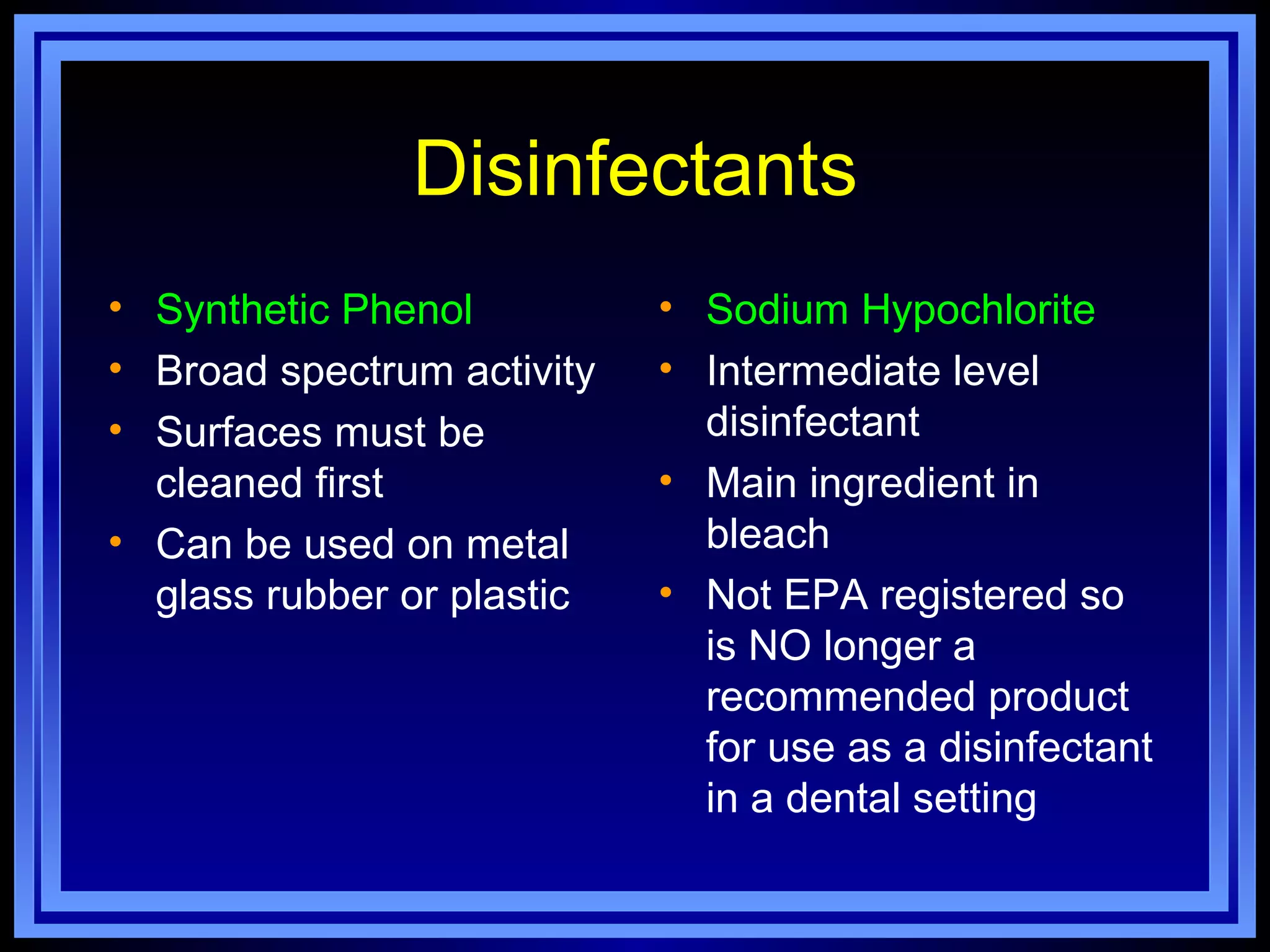
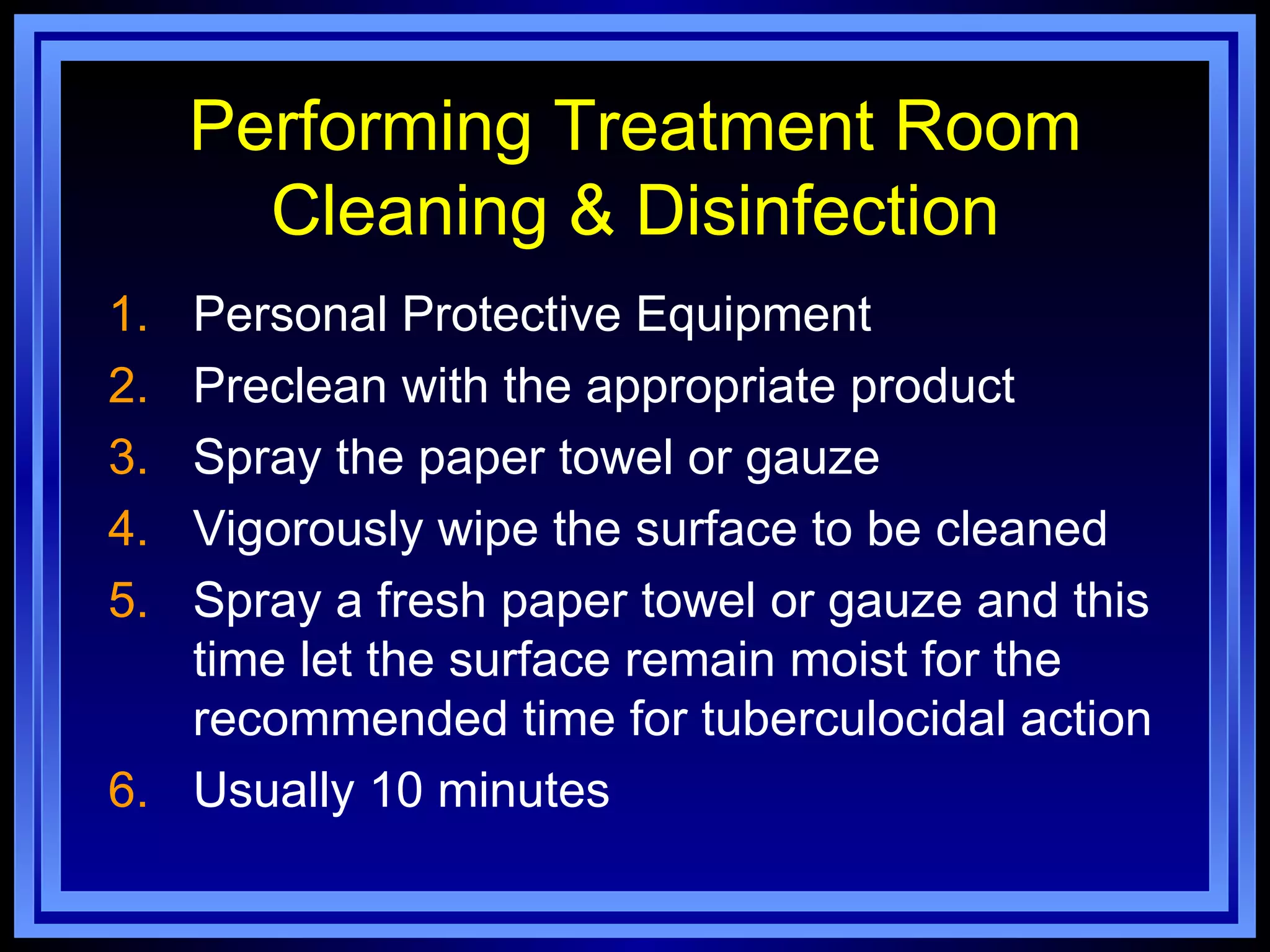
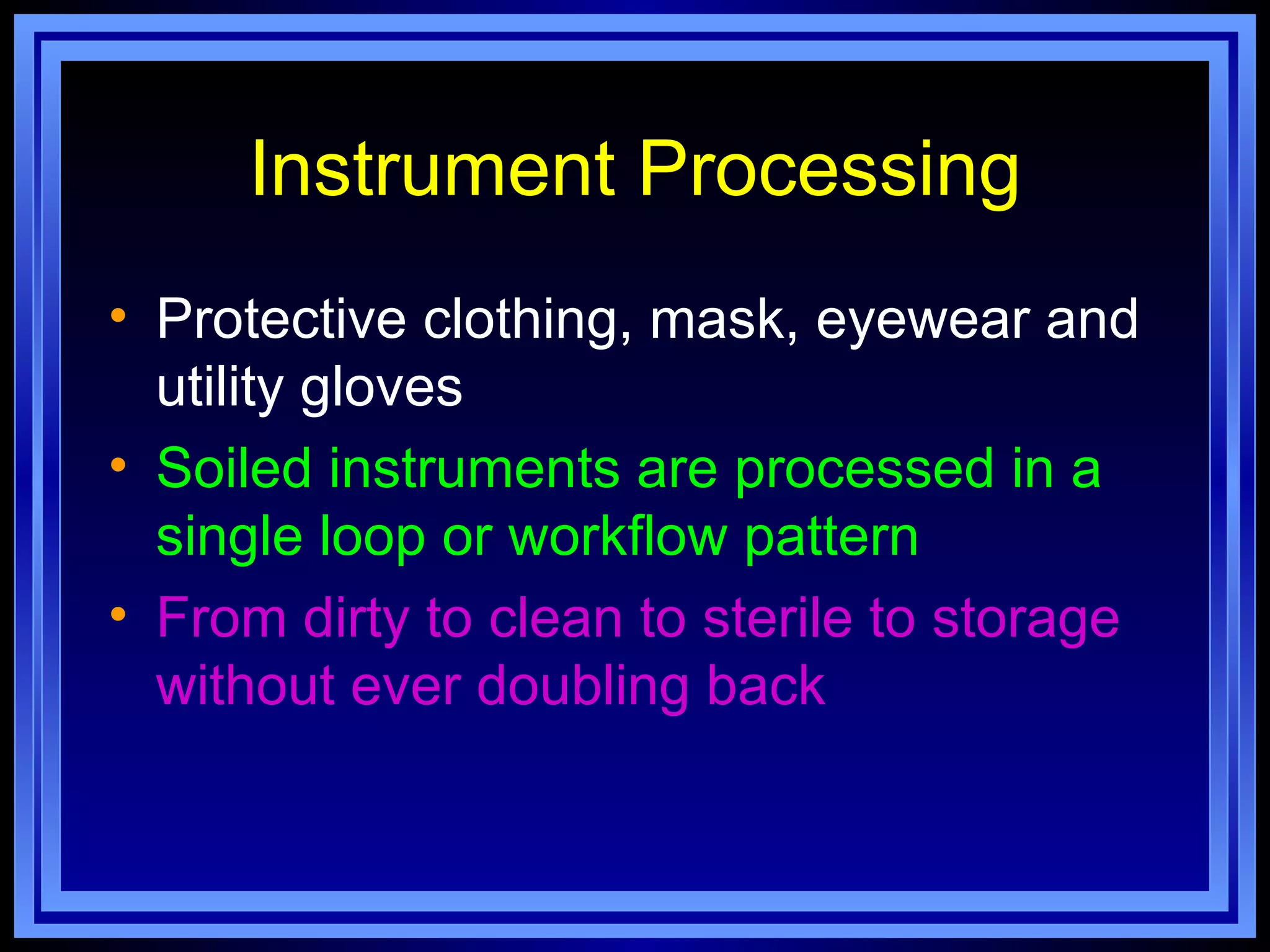
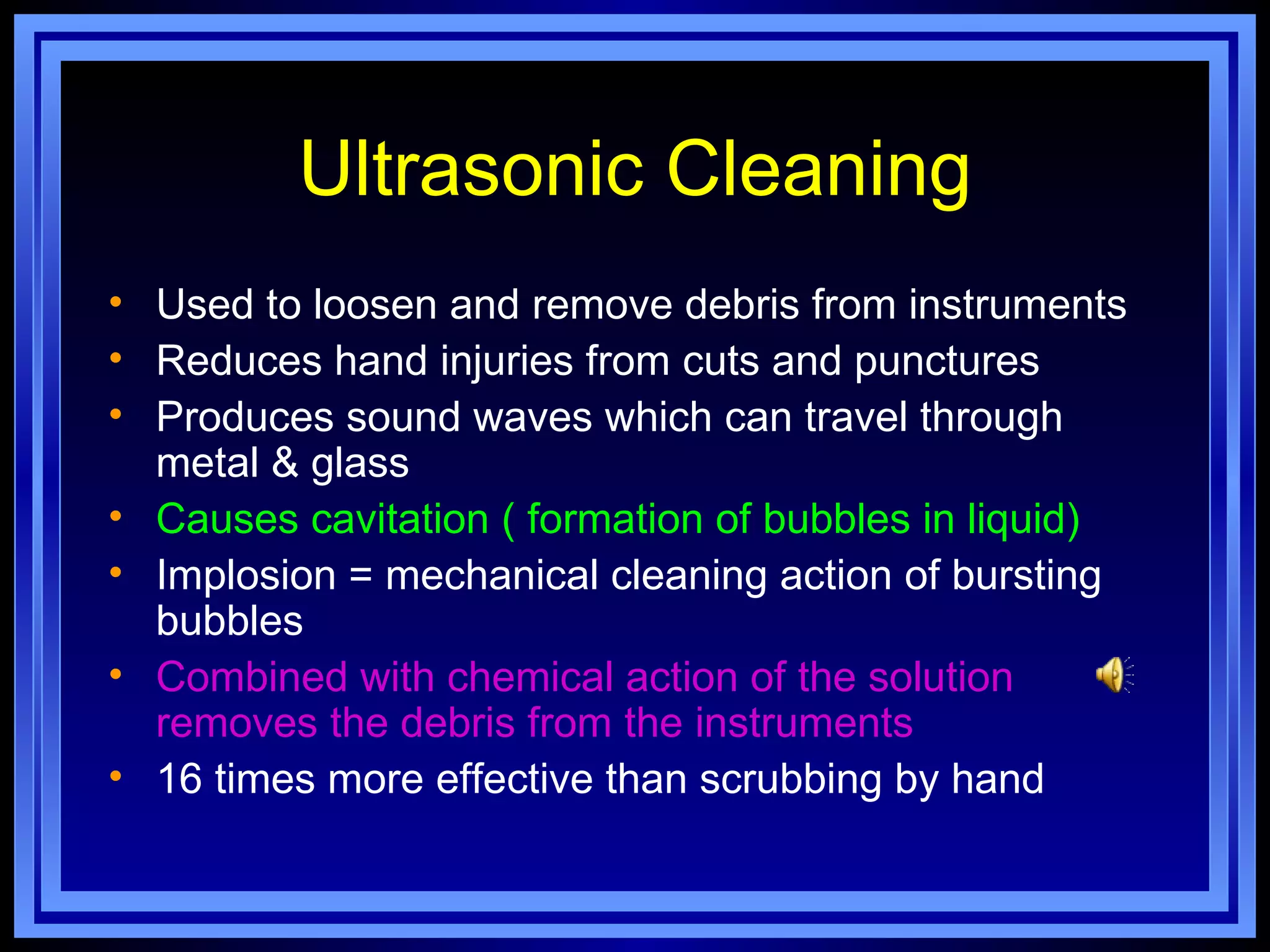
3. Proper sterilization, disinfection and barriers are critical for infection control. Sterilization kills all microbes using steam, dry heat or chemicals