This document discusses the laboratory diagnosis of infections caused by the genus Mycobacterium. It focuses on Mycobacterium tuberculosis and Mycobacterium leprae. Key points include:
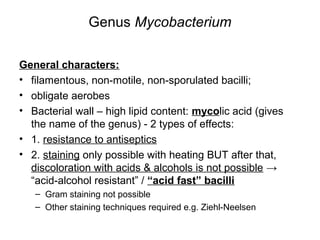
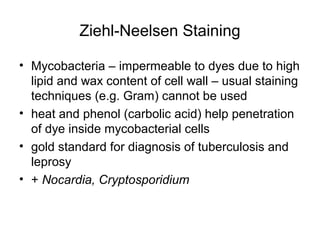
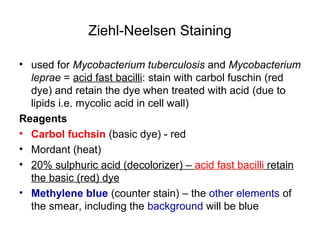
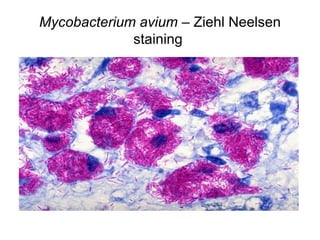
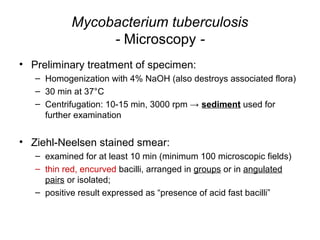
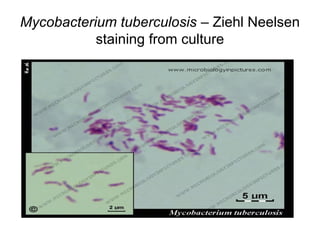
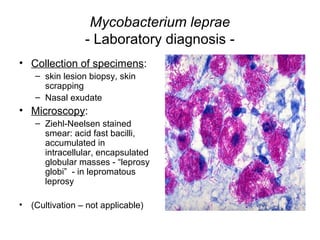
- Mycobacteria are acid-fast bacilli that require special staining techniques like Ziehl-Neelsen staining.
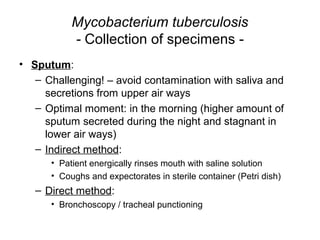
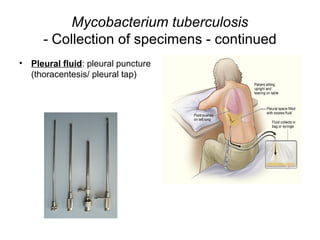
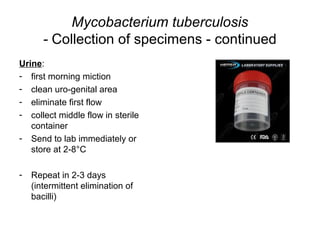
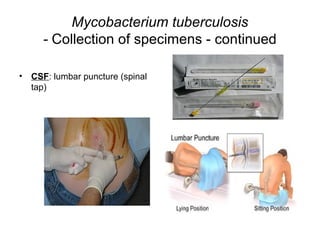
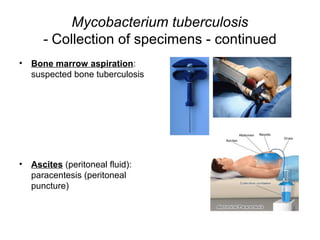
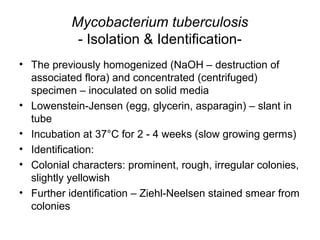
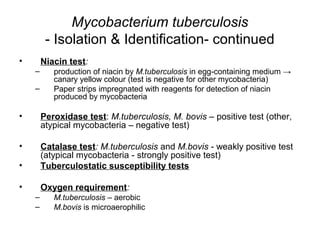
- Specimen collection and microscopy are used for diagnosis. Isolation requires slow growth on media like Lowenstein-Jensen. Identification uses tests for niacin, catalase, and tuberculostatic susceptibility.
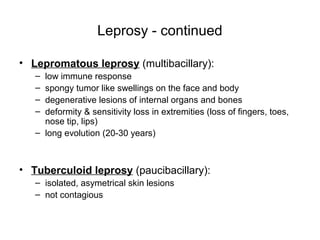
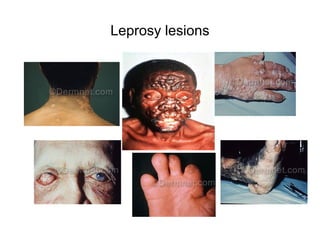
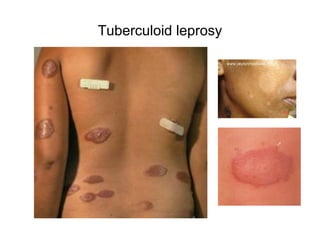
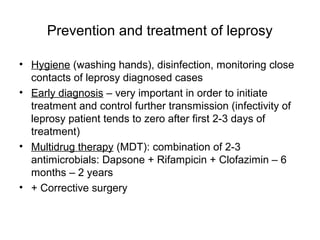
- Leprosy is caused by M. leprae and presents as lepromatous or tuberculoid forms. Diagnosis involves biopsy staining for acid-fast