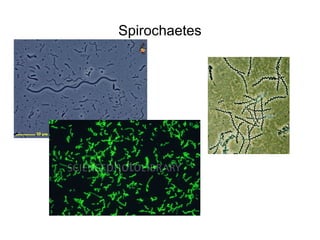
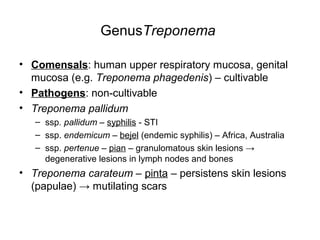
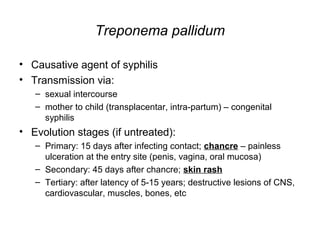
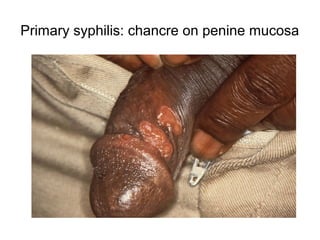
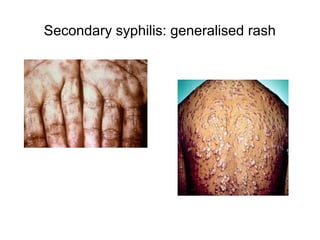
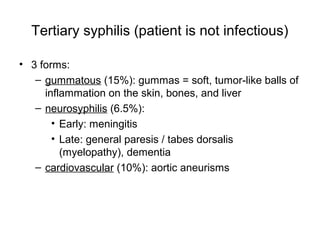
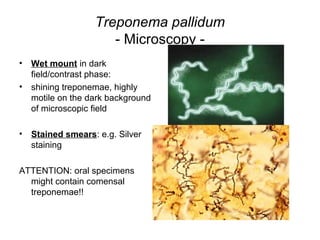
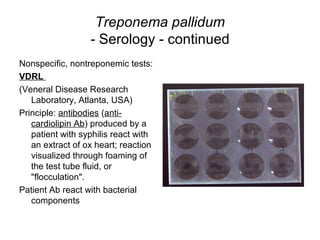
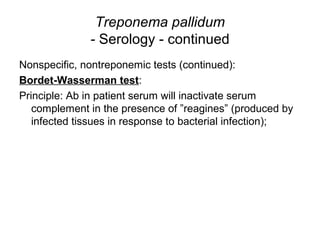
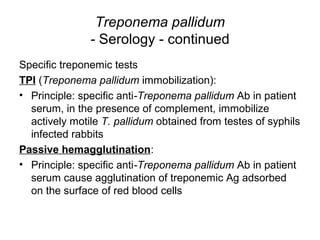
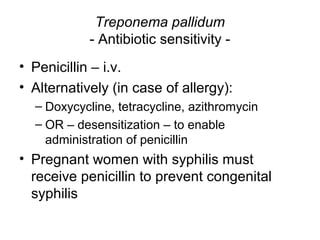
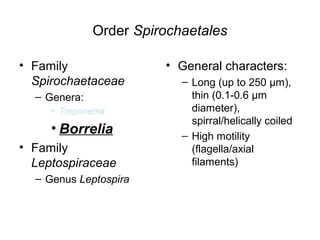
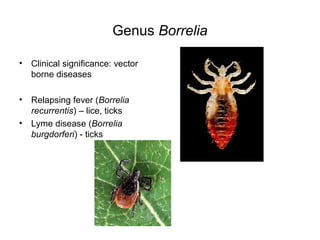
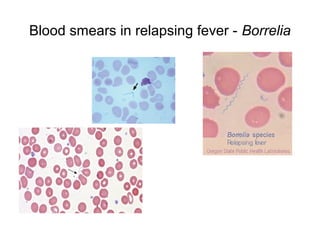
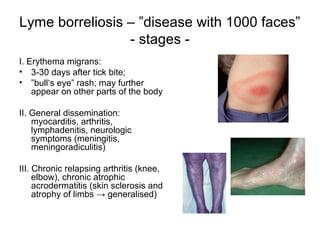
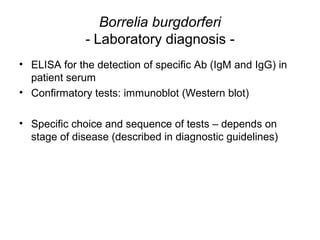
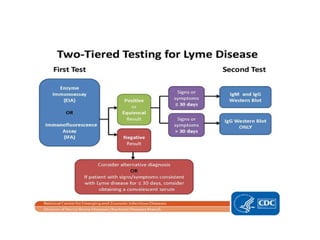
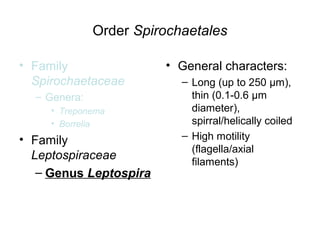
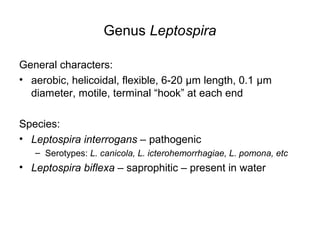
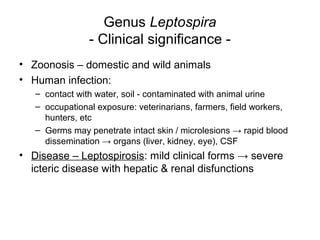
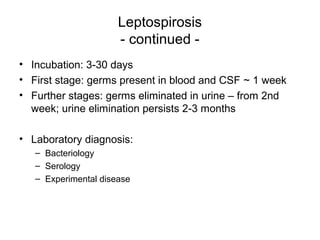
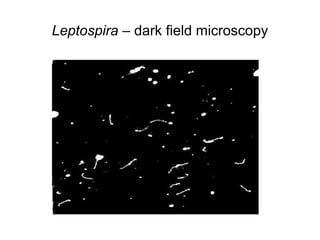
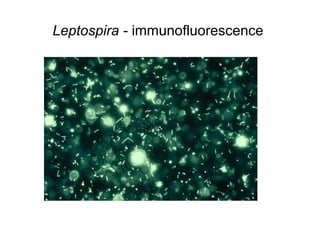
This document discusses the laboratory diagnosis of infections caused by Treponema, Borrelia, and Leptospira bacteria. It describes the characteristics and pathogenic species of each genus, how they cause diseases like syphilis, Lyme disease, and leptospirosis, and the methods used to diagnose infections through direct examination of clinical samples, culture techniques, and serological tests. Key diagnostic tests include darkfield microscopy, immunofluorescence, culture media, microscopic agglutination, ELISA and Western blot. Penicillin and doxycycline are commonly used for treatment.