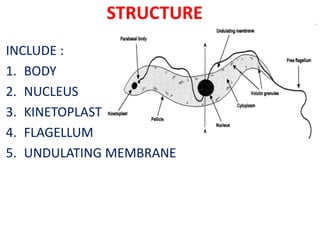
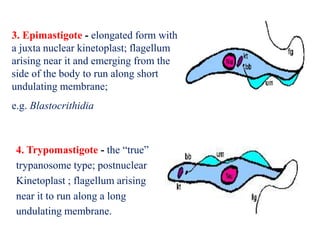
The document discusses hemoflagellates, single-celled flagellated parasites that infect the blood and tissues of humans and animals. It describes the structure, life cycles, transmission, geographic distribution, pathogenesis, diagnosis, treatment, and prevention of two important genera of hemoflagellates: Trypanosoma brucei, which causes African sleeping sickness, and Trypanosoma cruzi, which causes Chagas disease in South and Central America. Key aspects of the parasites, diseases they cause, and approaches to control are summarized.