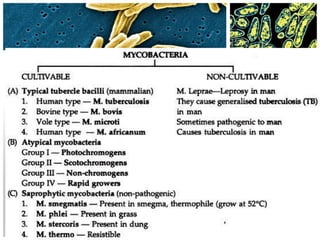
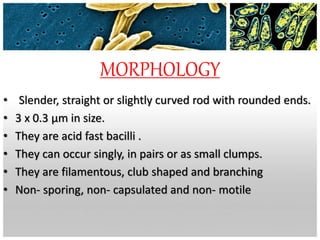
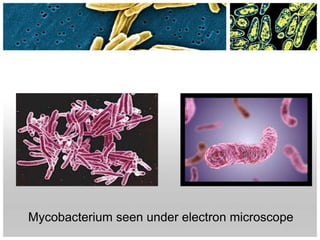
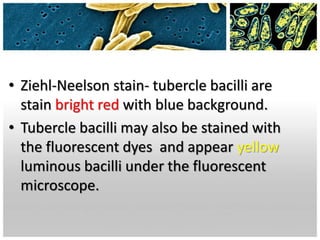
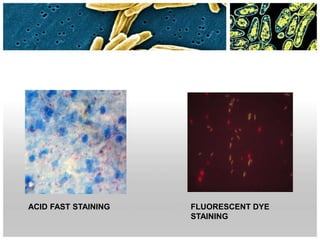
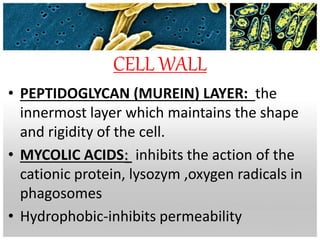
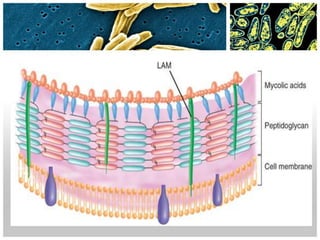
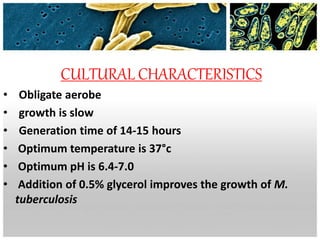
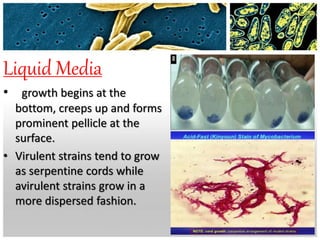
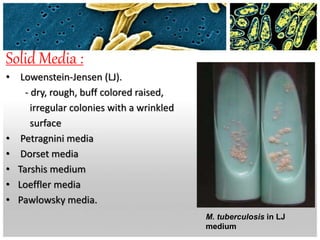
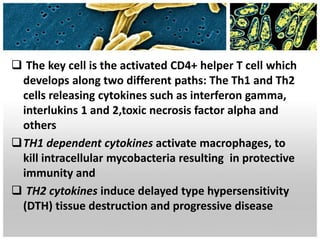
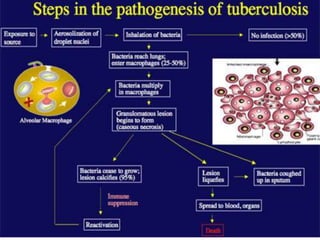
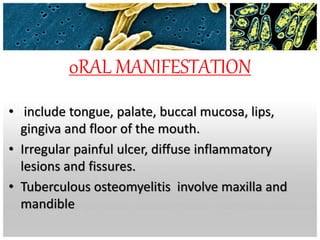
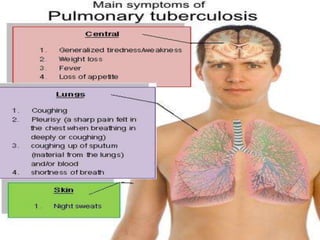
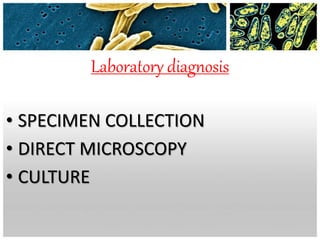
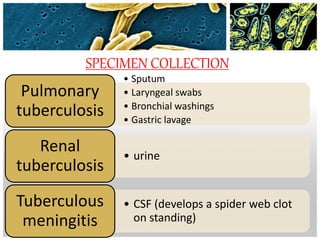
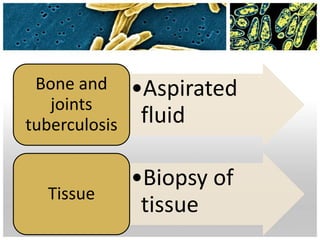
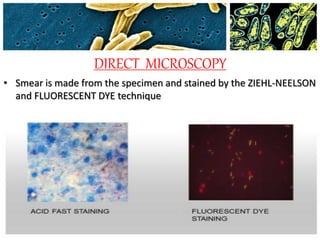
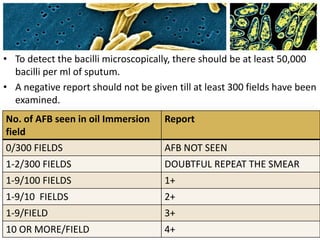
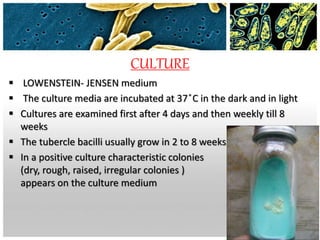
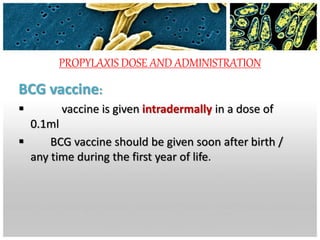
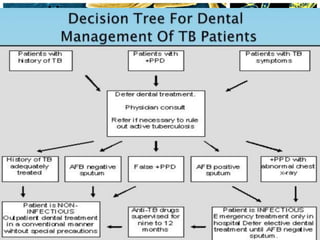
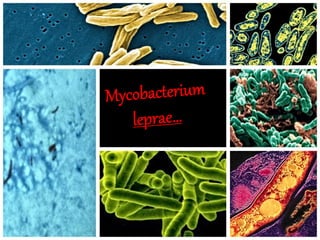
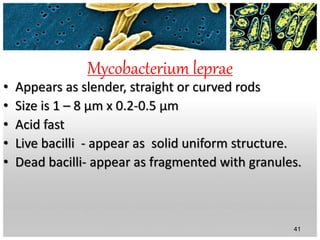
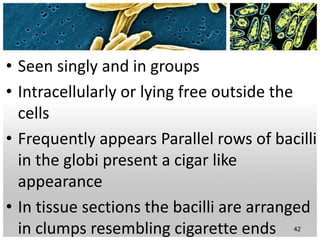
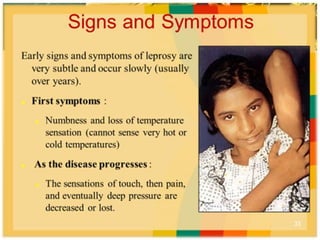
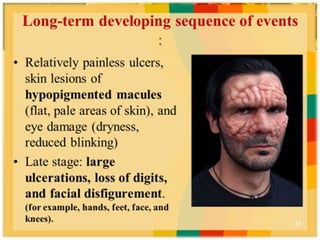
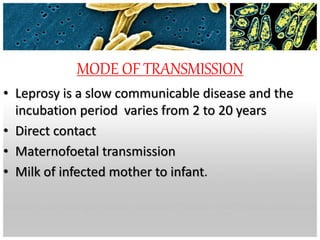
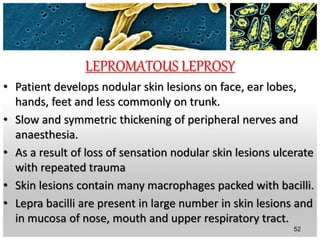
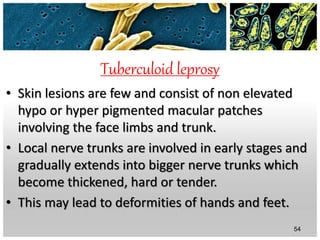
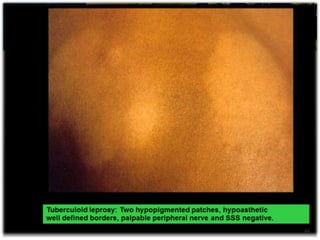
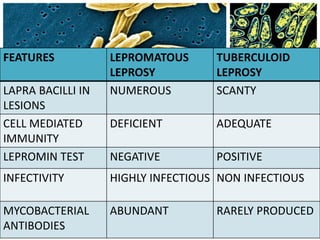
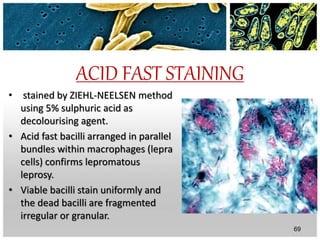
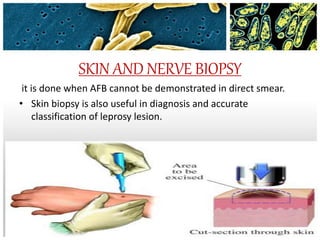
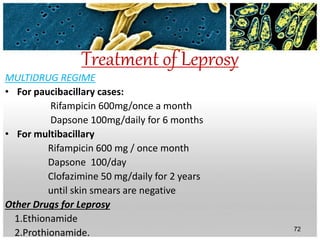
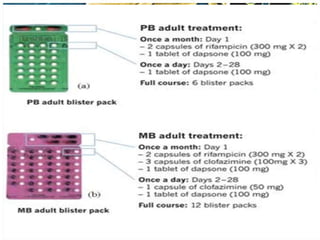
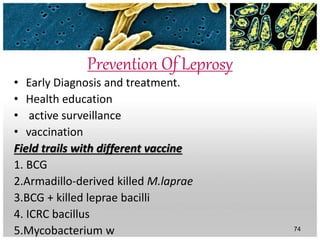
M. tuberculosis and M. leprae are acid-fast bacilli that cause tuberculosis and leprosy, respectively. M. tuberculosis was discovered in 1882 and is transmitted through droplets. It has a cell wall containing mycolic acids and is a slow growing obligate aerobe. Laboratory diagnosis involves acid-fast staining of samples from sputum or tissues, as well as culturing on media like LJ. Treatment uses multi-drug therapy including isoniazid and rifampin. M. leprae causes a chronic granulomatous disease affecting skin and nerves. It is not cultivable but can be propagated in animals. Classification systems include tuberculoid, lepromatous, and