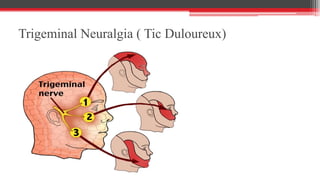
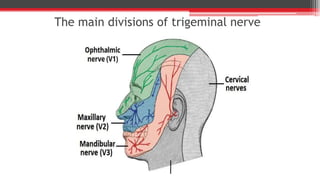
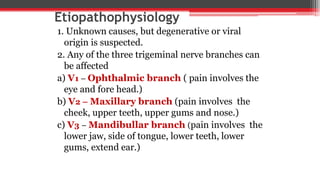
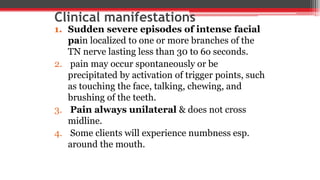
Trigeminal neuralgia, also known as tic douloureux, is a disorder of the trigeminal nerve causing episodes of severe, stabbing facial pain. It most often affects older adults and the pain is localized to areas innervated by the trigeminal nerve branches. Diagnosis involves evaluating the characteristic pain pattern and neurological exam. Treatment begins with carbamazepine medication and may require surgical interventions like microvascular decompression if medications fail. Nursing care focuses on pain management, nutrition support, and monitoring for anxiety or depression due to the chronic pain condition.