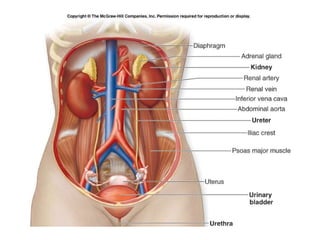
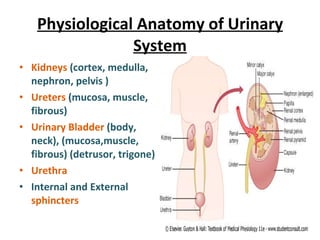
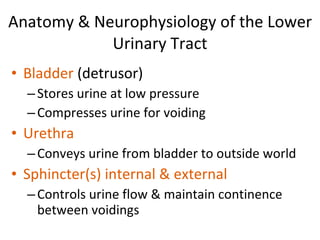
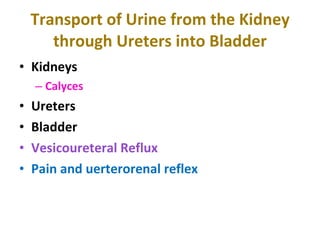
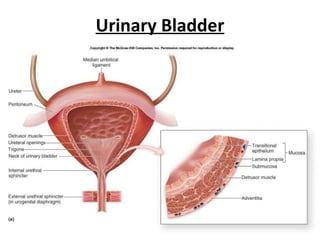
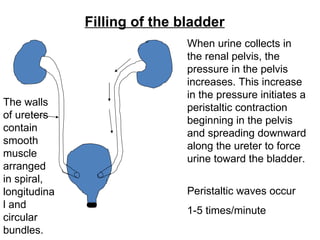
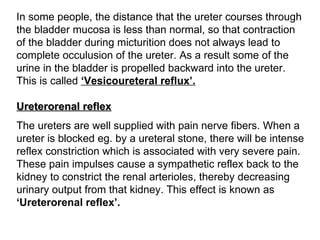
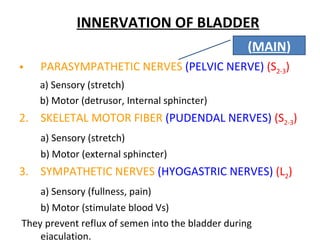
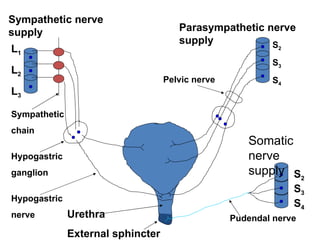
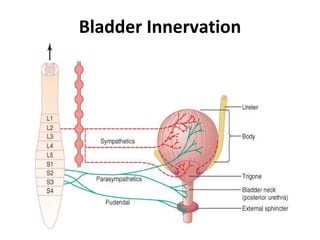
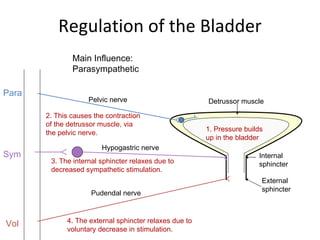
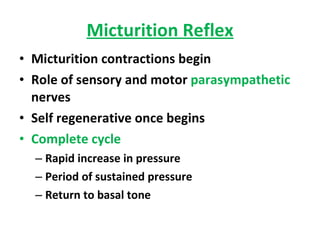
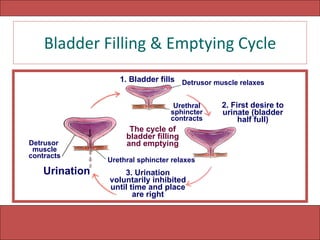
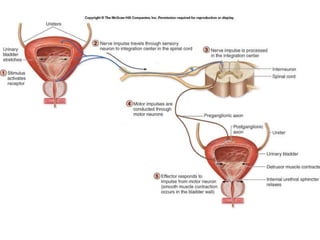
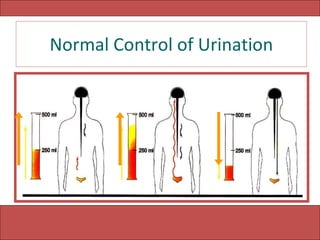
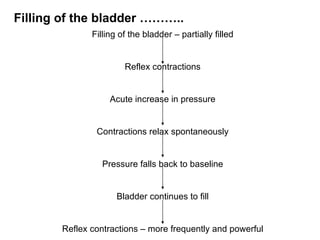
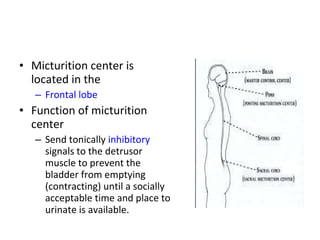
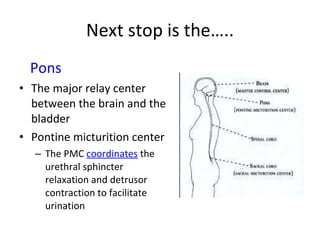
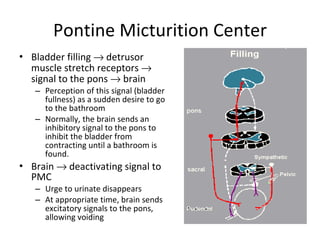
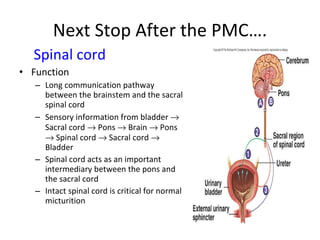
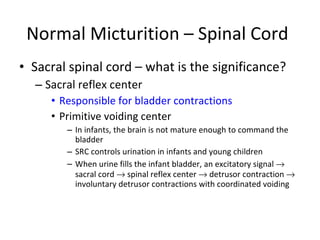
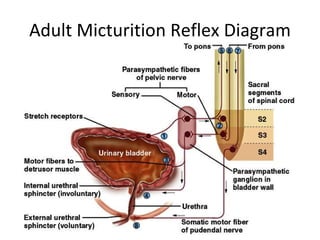
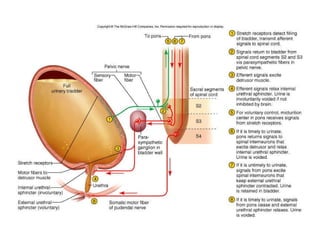
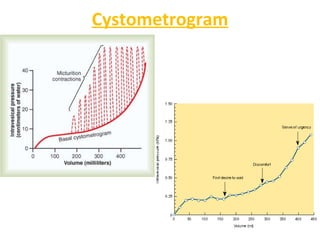
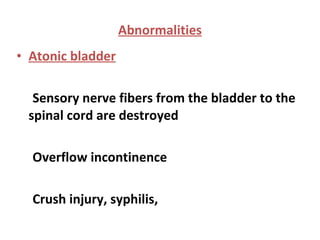
The document summarizes the anatomy and physiology of the urinary system and micturition process. It describes how urine is transported from the kidneys to the bladder through the ureters. It explains that the bladder stores urine through a balance of parasympathetic and sympathetic signals until reaching capacity, at which point a spinal micturition reflex is triggered to initiate voiding through coordinated detrusor contraction and urethral sphincter relaxation under control of the pontine micturition center. Higher brain centers can facilitate or inhibit micturition.