Hydrocephalus, commonly known as "water on the brain", is an abnormal buildup of cerebrospinal fluid (CSF) in the brain's ventricles. Congenital/infantile hydrocephalus develops before age 3 and causes the skull to enlarge rapidly. Common causes include brain hemorrhages, infections, or malformations. Symptoms include a tense, enlarged head and developmental delays. As pressure increases, vision loss, seizures, and cognitive impairments occur. Untreated, hydrocephalus can be fatal due to brain herniation through openings in the skull.
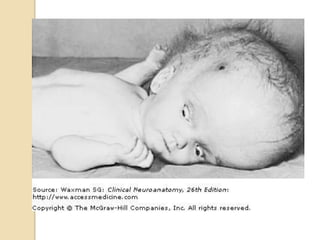








![ even of mild degree, it molds the
shape of the skull in early life
in radiographs the inner table is
unevenly thinned, an appearance
referred to as "beaten silver" or as
convolutional or digital markings.
The frontal regions are unusually
prominent [bossing]](https://image.slidesharecdn.com/hydrocephalus-120416141248-phpapp02/85/Hydrocephalus-by-DR-ARSHAD-10-320.jpg)












![ an increase in volume of any one of
these three components must be at
the expense of the other two [Monro-
Kellie doctrine]
Compensatory measures
Small increments in brain volume do
not immediately raise the ICP due to
displacement of CSF from the cranial
cavity into the spinal canal](https://image.slidesharecdn.com/hydrocephalus-120416141248-phpapp02/85/Hydrocephalus-by-DR-ARSHAD-23-320.jpg)























































