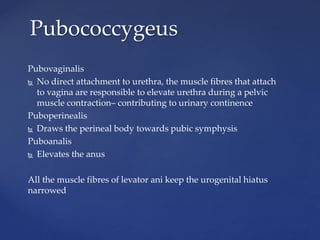
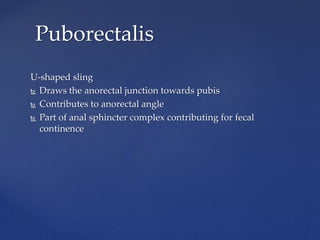
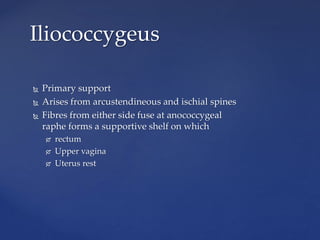
The document summarizes pelvic floor anatomy and functions. It describes the levator ani muscles as the most important muscles that support pelvic organs. It outlines the boundaries and contents of the pelvis, perineum, and anterior and posterior triangles. Key structures like the anal sphincter complex, perineal body, and pelvic floor innervation are defined. The document also discusses pelvic floor dysfunction, classifications of perineal tears, and exercises to strengthen the pelvic floor muscles.
![PELVIC FLOOR
DR. SOWJANYA KURAKULA
MBBS, MD [OBS & GYN]](https://image.slidesharecdn.com/pelvicfloor-150426091311-conversion-gate02/85/Pelvic-floor-1-320.jpg)