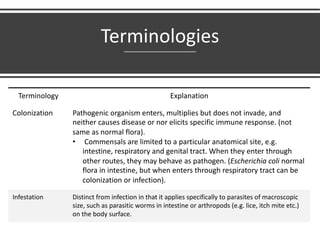
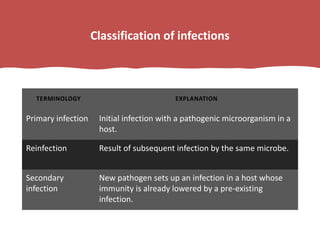
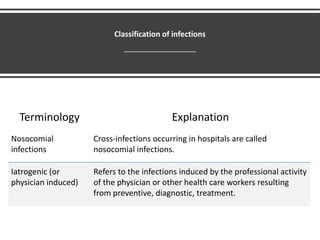
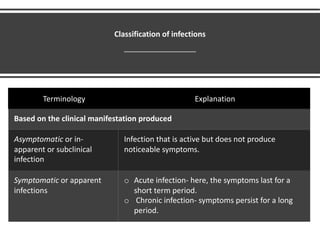
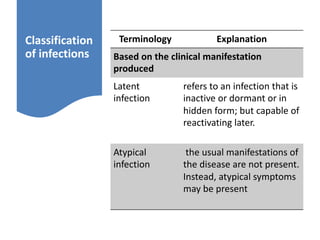
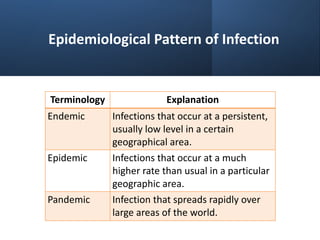
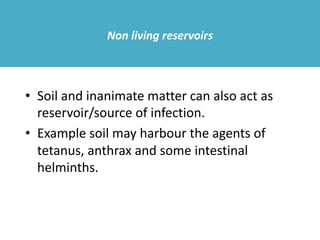
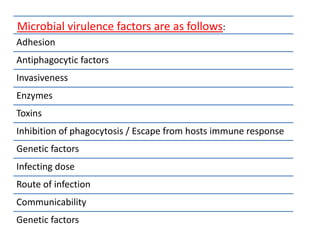
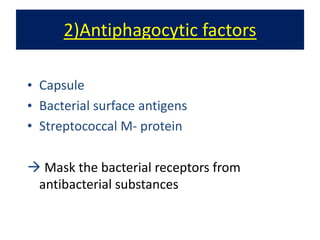
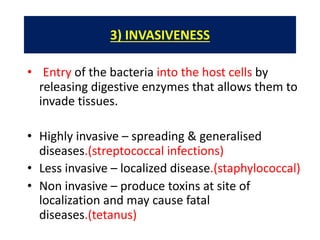
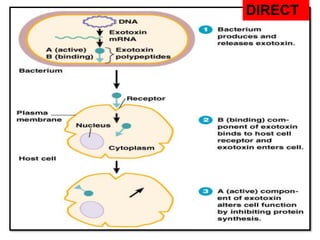
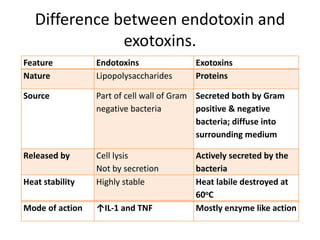
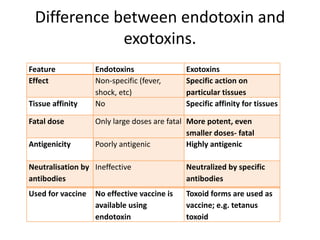
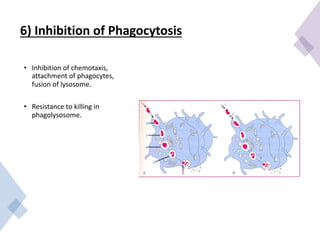
The document defines various terminologies related to microbial pathogenicity and infection. It discusses terms like saprophytes, parasites, commensals, pathogens, opportunistic pathogens, infection, colonization, infestation, and more. It also classifies infections based on factors like source, clinical manifestation, epidemiological patterns, and more. Finally, it covers various mechanisms of microbial pathogenicity like adhesion, invasiveness, toxins, inhibition of phagocytosis, and more.