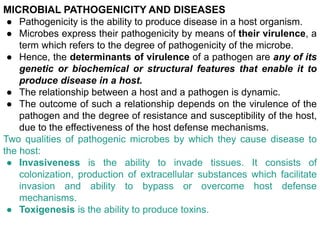
The document discusses microbial pathogenicity and the progression of infection and disease. It provides details on:
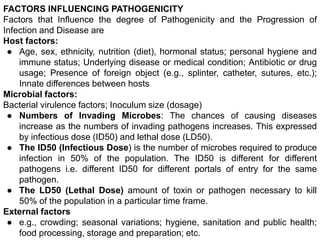
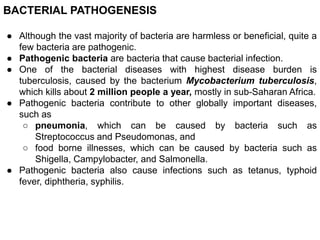
1) The factors that influence a microbe's pathogenicity, including host factors like age and immune status, and microbial factors like virulence factors and inoculum size.
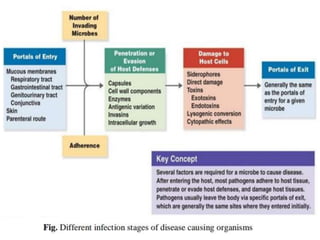
2) The steps in pathogenesis which include a microbe gaining access to the host, adhering to tissues, penetrating defenses, and damaging the host directly or through toxins.
3) The two qualities that allow microbes to cause disease - invasiveness and toxigenesis. It also discusses bacterial adherence, biofilm formation, and how pathogens prevent host defenses.