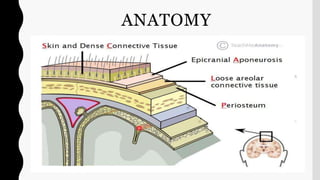
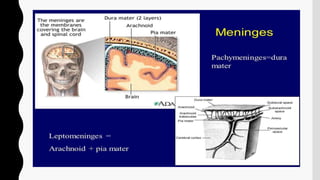
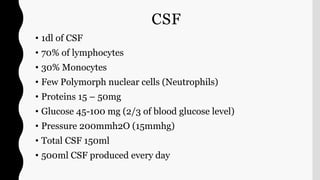
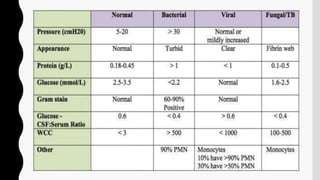
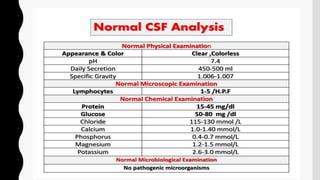
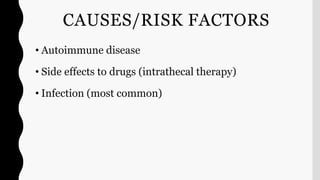
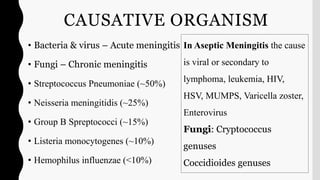
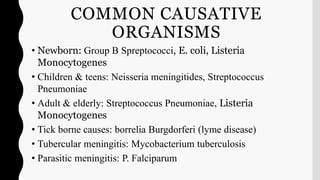
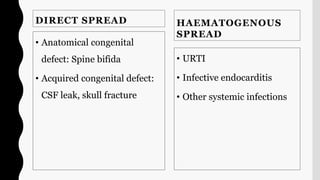
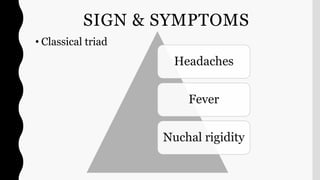
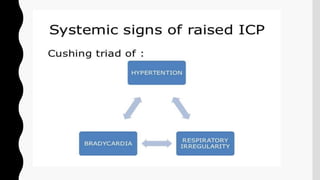
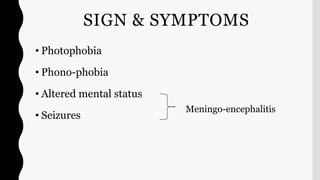
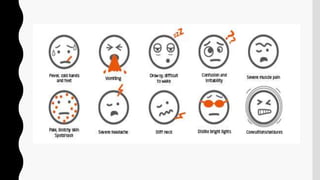
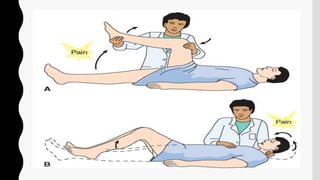
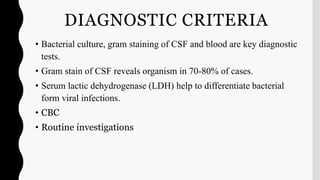
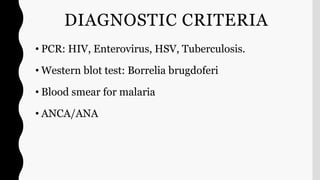
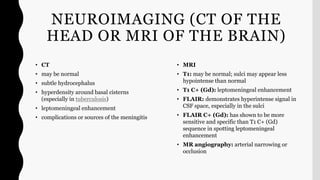
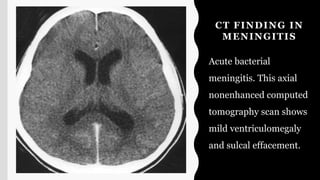
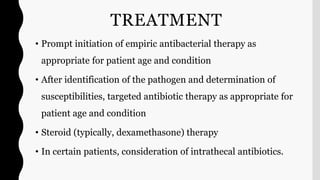
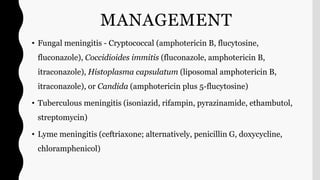
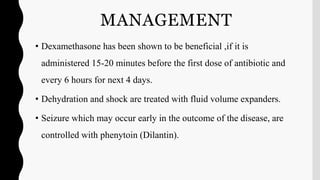
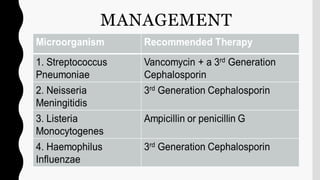
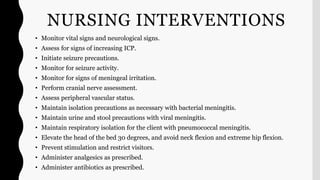
The document discusses meningitis, including its anatomy, causes, symptoms, diagnostic criteria, treatment, and nursing management. Meningitis is an inflammation of the protective membranes covering the brain and spinal cord known as the meninges, which can be caused by bacterial, viral, or fungal infections. Symptoms include headache, fever, and neck stiffness, while diagnosis involves lumbar puncture, CSF analysis, and neuroimaging.
![MENINGITIS
Evaluator: Mr L Anand Presenter: Shruti Shirke
[Asso professor, CON AIIMS BBSR] M.Sc Neuroscience Nursing](https://image.slidesharecdn.com/meningitisandbrainabscess-210806045753/75/Meningitis-and-brain-abscess-1-2048.jpg)