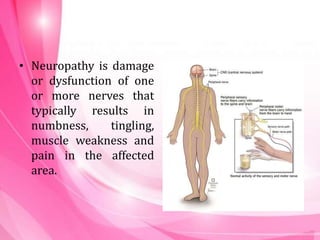
- Neuropathy is damage or dysfunction of nerves that causes numbness, tingling, weakness and pain. It can be cranial neuropathy affecting the brain/brainstem or peripheral neuropathy outside the brain/spinal cord.
- Cranial neuropathy types include Bell's palsy, microvascular issues affecting vision nerves, and damage to nerves controlling eye movement. Peripheral neuropathy can be motor, sensory or autonomic.
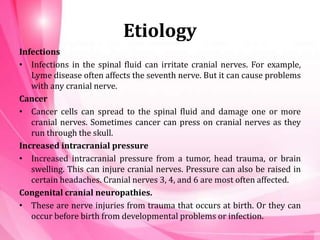
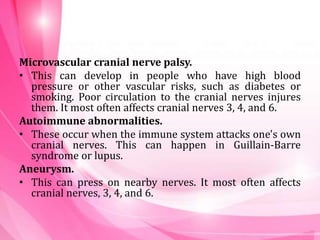
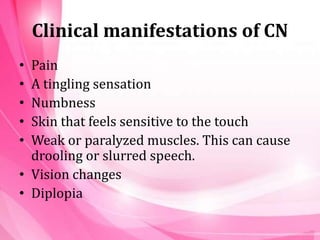
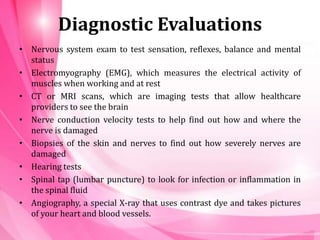
- Neuropathy is caused by infections, cancer, increased pressure, vascular issues like diabetes, autoimmune disorders, medications, and vitamin deficiencies. Symptoms vary but include pain, sensory changes, and weakness. Diagnosis involves exams, tests and sometimes biopsies. Treatment focuses on pain management, physical