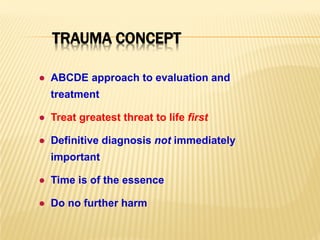
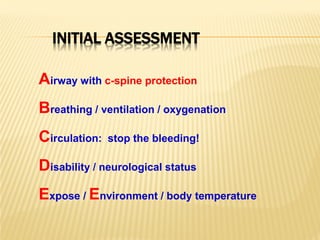
This document provides guidance on the management of multiple trauma patients. It outlines the ABCDE approach and trauma concept, which emphasizes rapidly assessing and treating the most life-threatening injuries first before making definitive diagnoses.
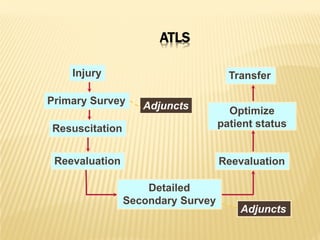
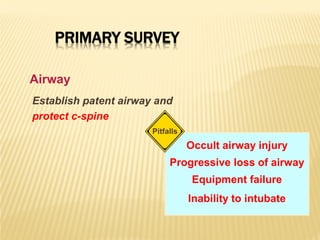
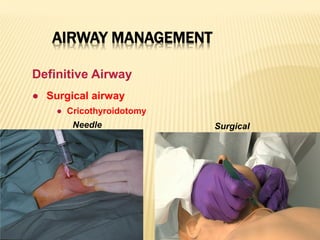
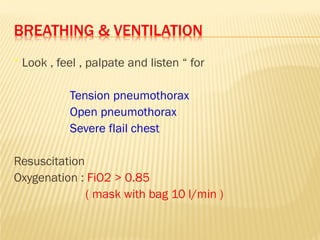
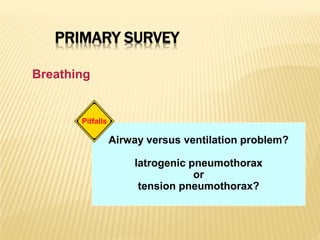
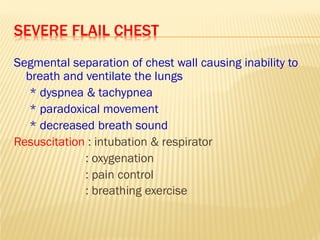
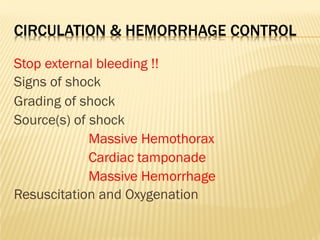
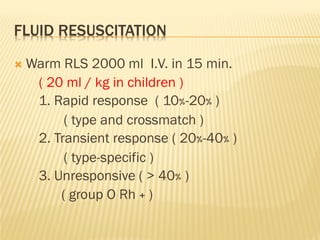
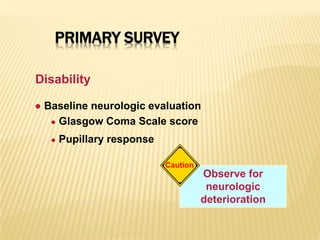
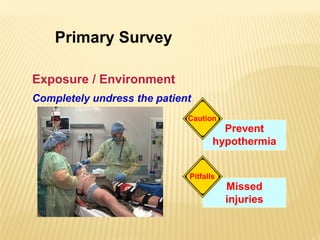
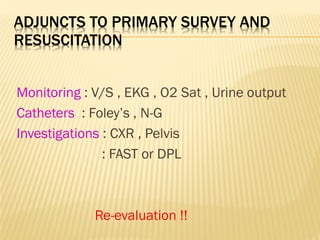
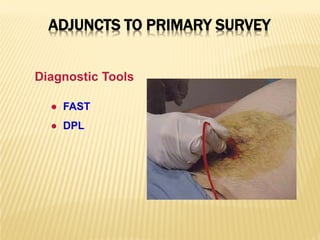
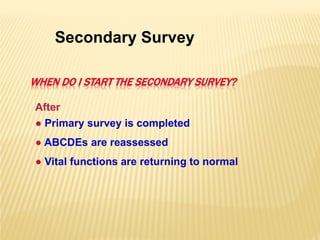
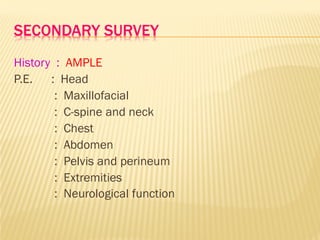
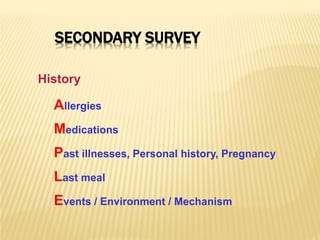
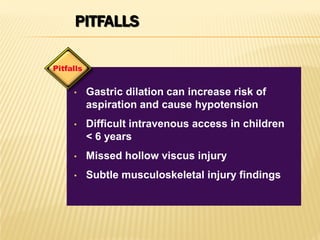
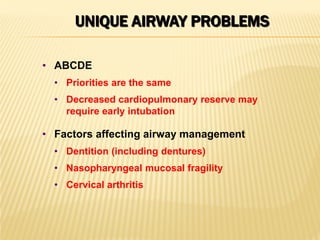
The primary survey involves simultaneously assessing the patient's airway, breathing, circulation, disability, and exposure. Adjuncts like monitoring, catheters and imaging may be used but not delayed transfer. The secondary survey obtains a more detailed history and physical exam.
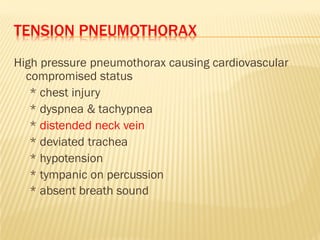
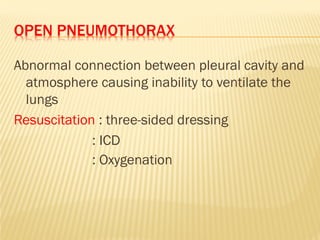
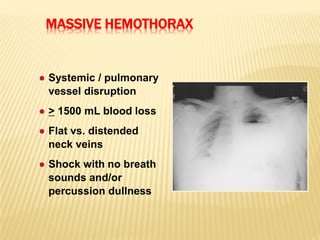
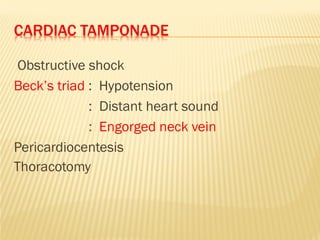
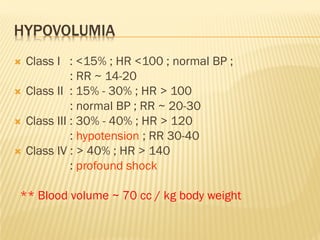
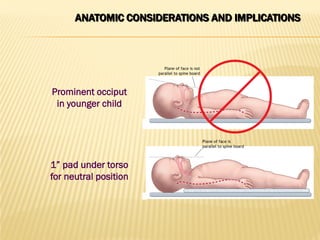
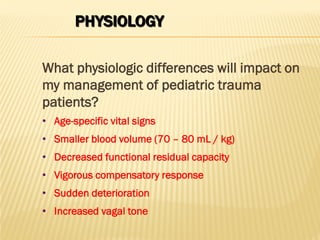
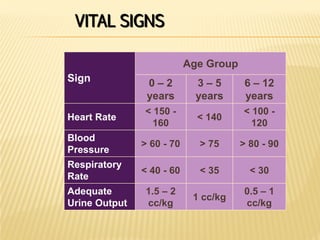
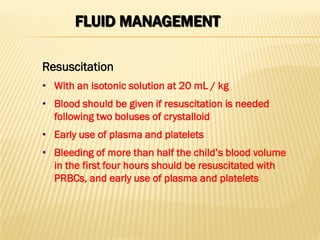
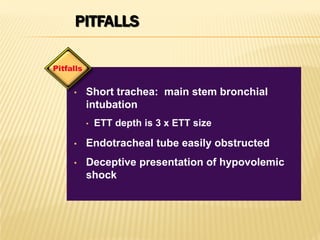
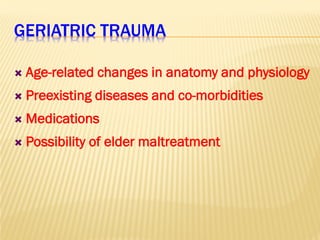
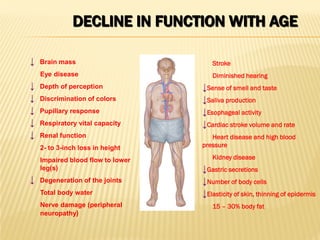
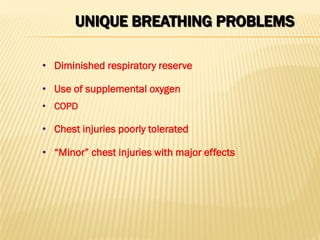
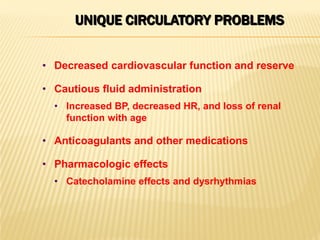
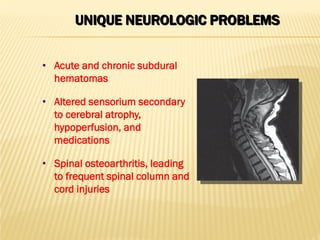
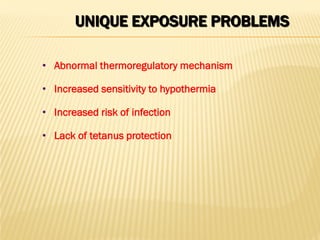
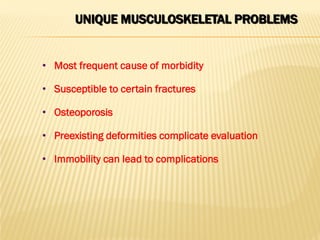
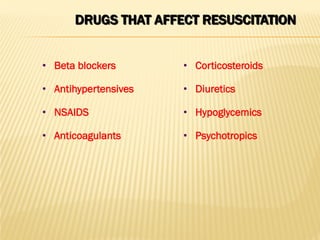
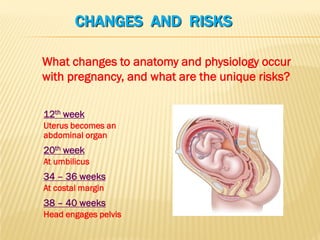
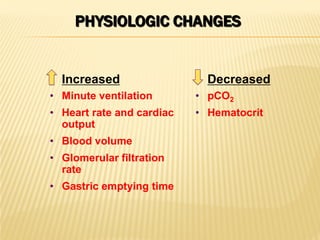
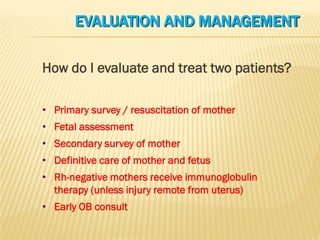
Special considerations for pediatric, geriatric, and pregnant trauma patients are discussed. Key physiological differences and injury patterns are highlighted. The document also reviews complications like tension pneumothorax, cardiac tamponade and hemorrhagic shock and their