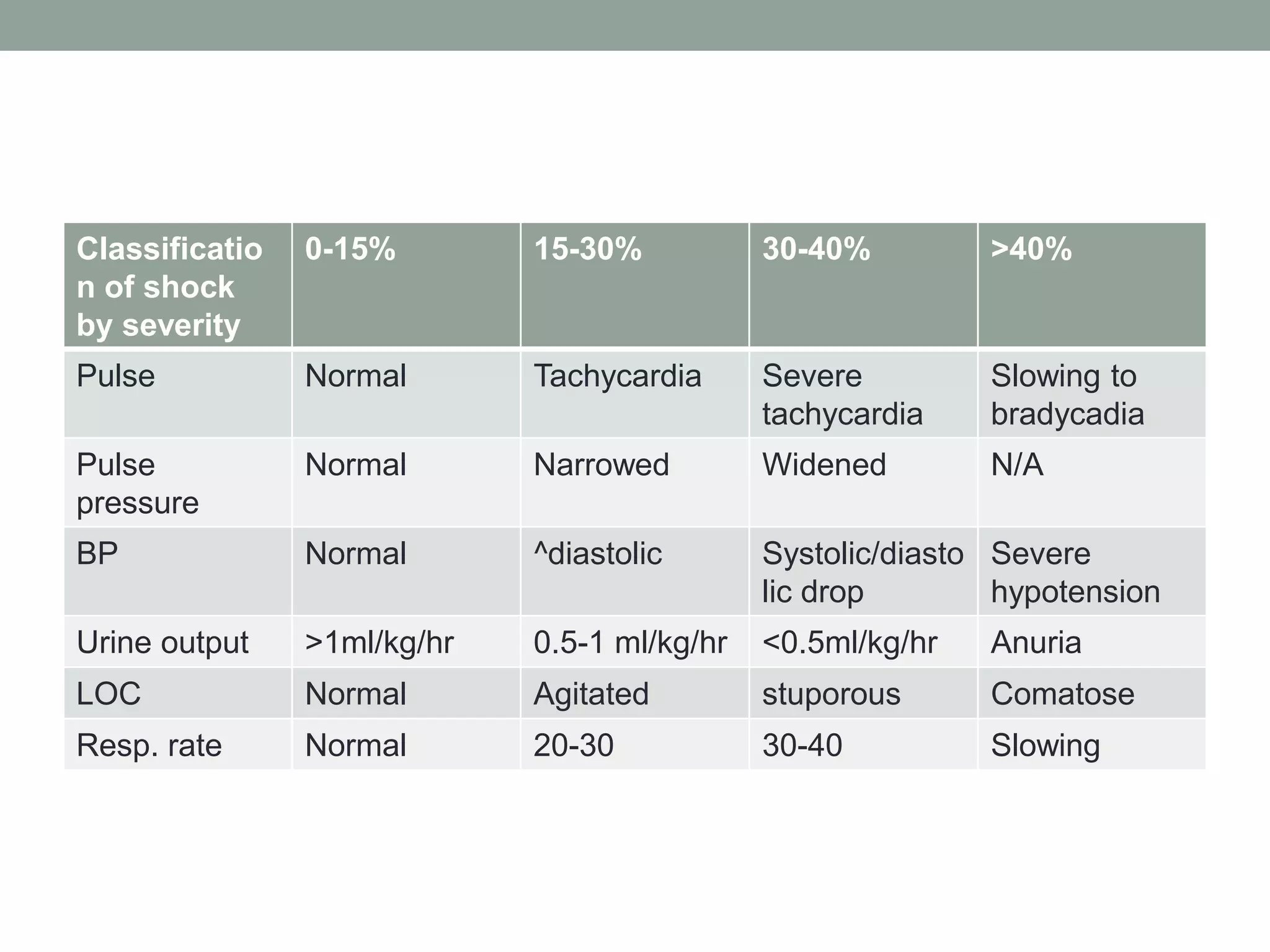
The document provides guidance on evaluating and treating polytrauma patients. It outlines the goals of trauma resuscitation which include identifying life-threatening injuries. The Advanced Trauma Life Support (ATLS) approach is recommended as a safe standardized method, beginning with the primary survey of ABCDE (airway, breathing, circulation, disability, exposure). Key assessments include mechanism of injury, vital signs, neurological status, and bleeding control. A thorough secondary survey then involves a full head-to-toe examination. Guidance is given on managing specific injuries such as abdominal trauma, with operative intervention prioritized for unstable patients or those with signs of internal bleeding.