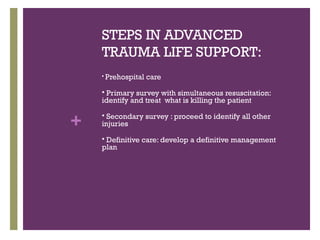
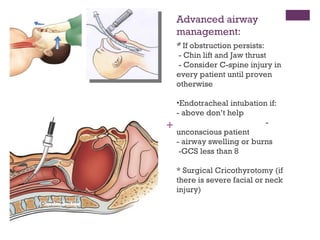
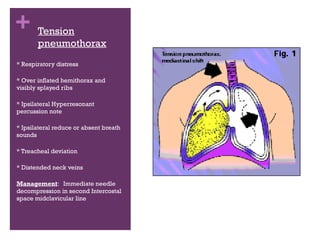
The document discusses trauma management and the primary and secondary surveys. It describes a case of a 25 year old male who fell 20 feet and is complaining of abdominal pain. It then covers the mechanisms of trauma, the three peaks of death from trauma, and the steps in advanced trauma life support. It provides details on the primary survey to assess the ABCDEs (airway, breathing, circulation, disability, exposure/environment). It then discusses performing the secondary survey to fully examine the patient and obtain their history.