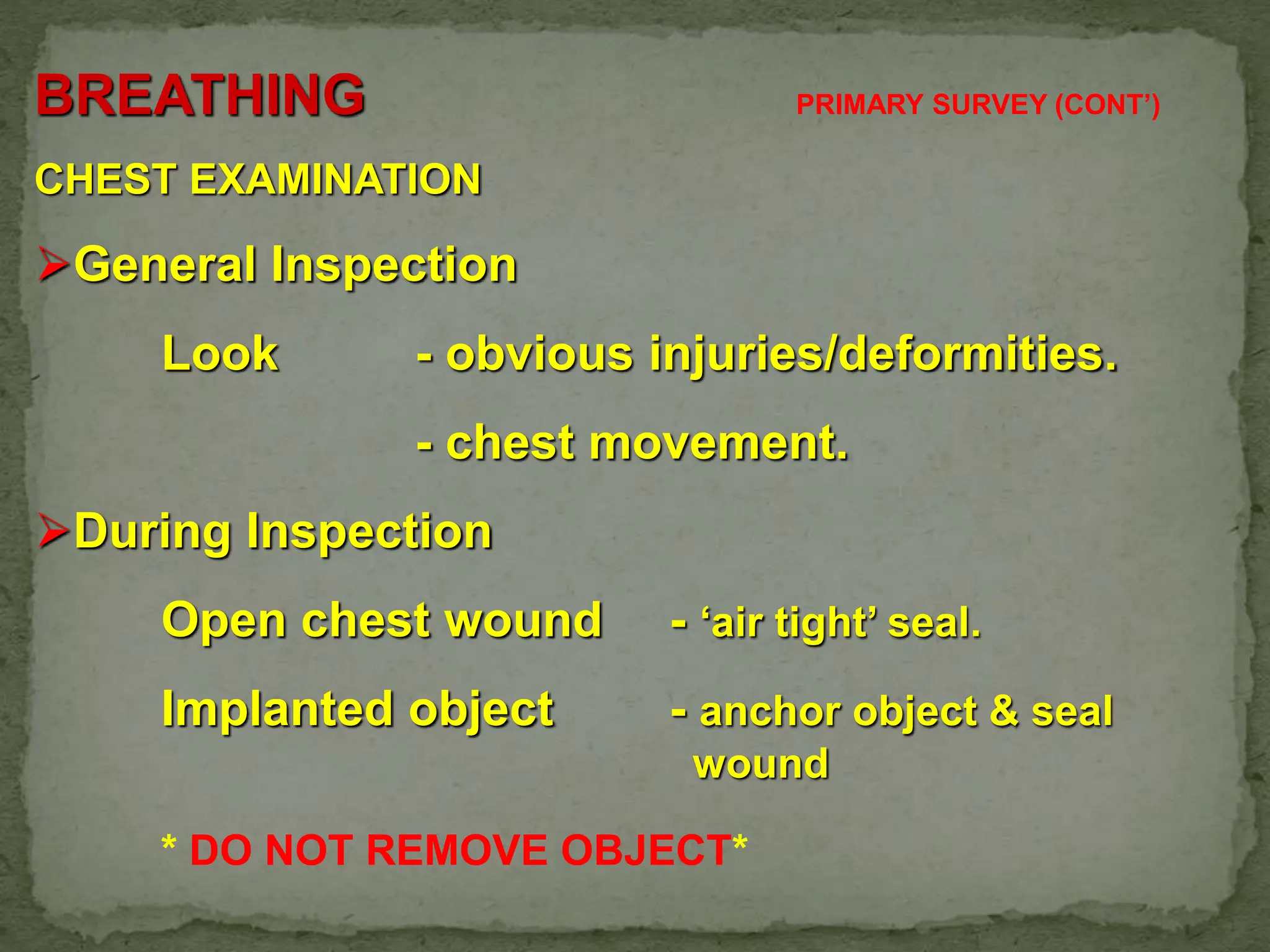
The document discusses the primary and secondary survey process for polytrauma patients. It outlines the three peaks of trauma death - within seconds to minutes, minutes to hours, and days to weeks after injury. The primary survey focuses on assessing life-threatening conditions involving the airway, breathing, circulation, disability, and exposure within 2 minutes. Conditions like tension pneumothorax, massive hemothorax, open pneumothorax, flail chest, and cardiac tamponade require immediate diagnosis and treatment. The secondary survey involves a full history and physical exam to identify and manage all injuries. Reevaluation of the patient is important after each survey due to the dynamic nature of trauma.