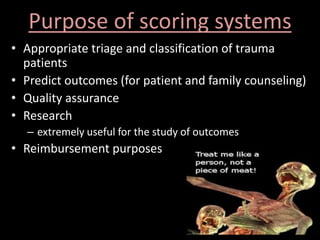
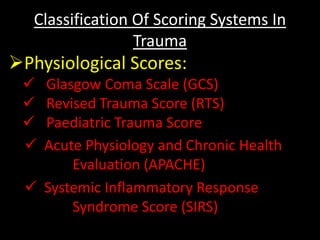
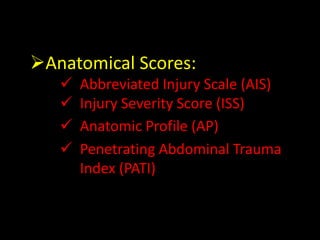
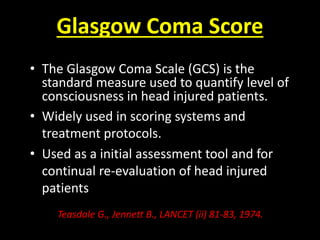
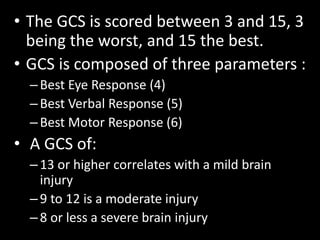
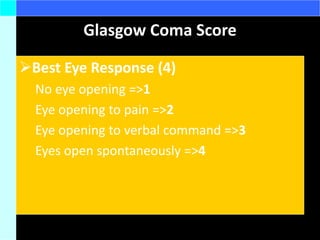
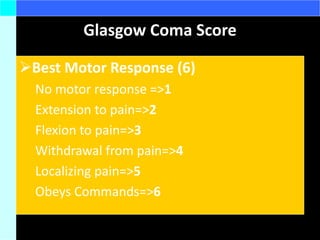
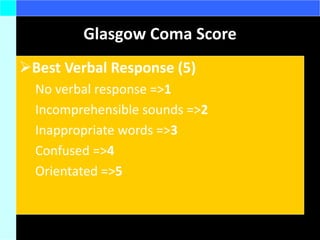
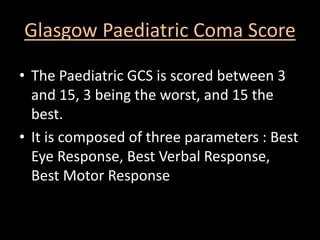
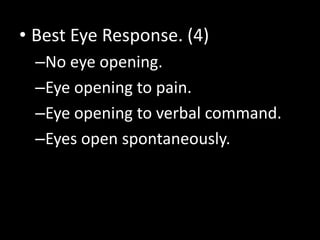
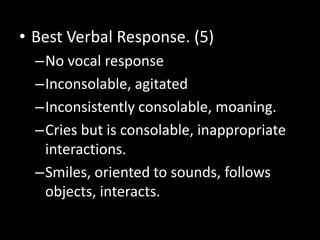
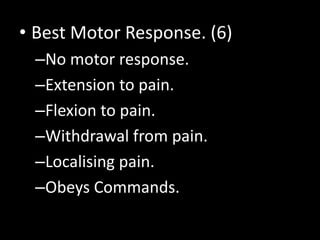
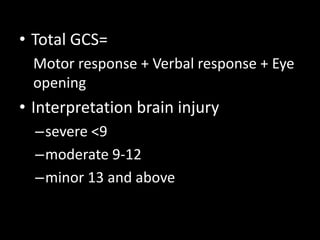
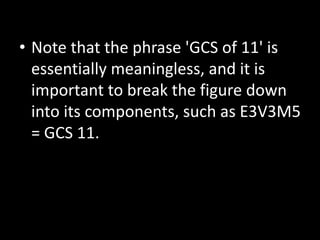
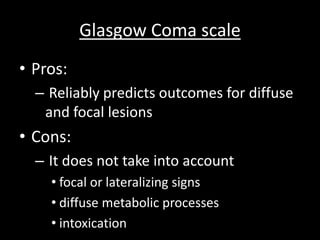
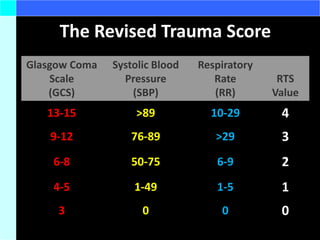
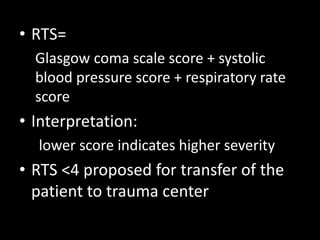
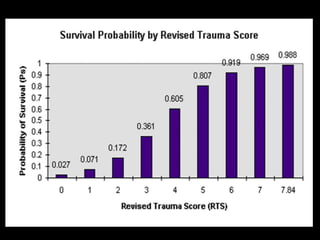
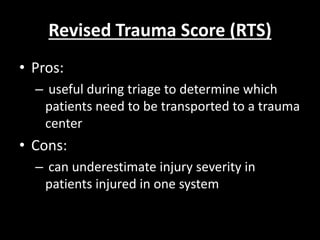
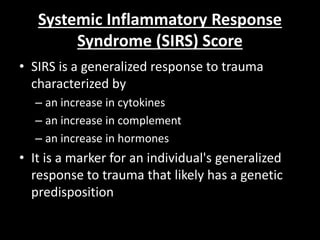
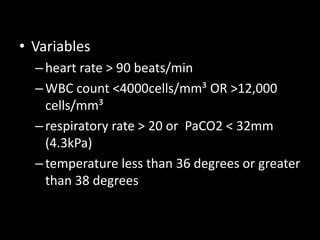
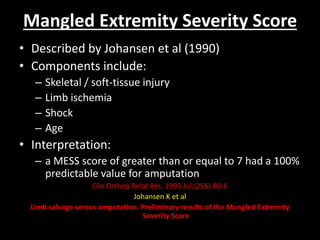
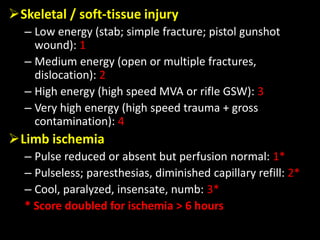
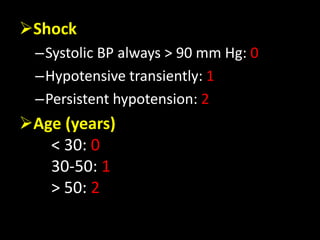
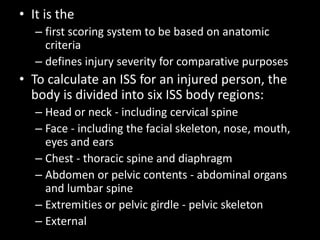
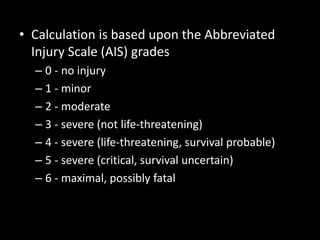
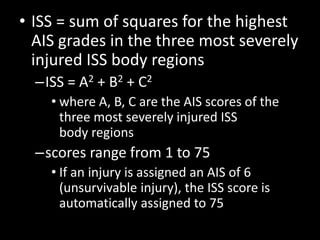
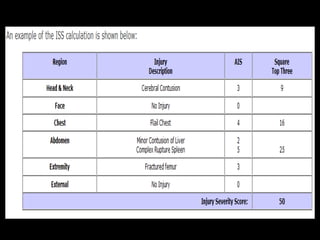
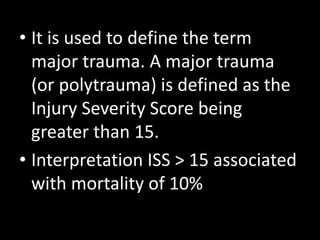
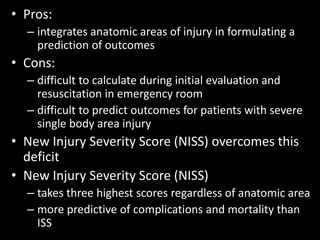
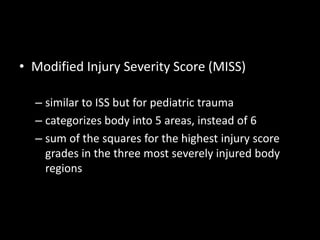
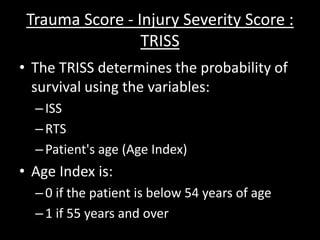
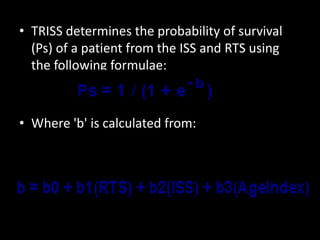
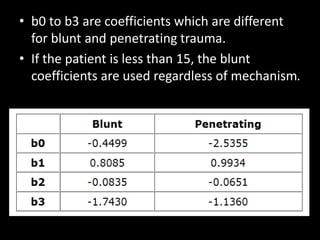
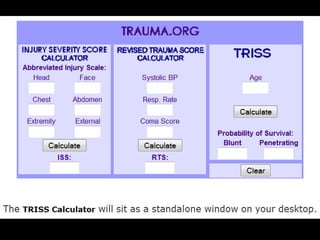
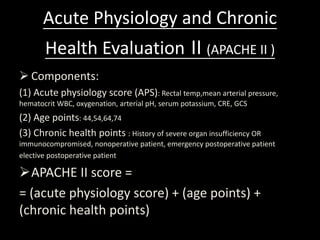
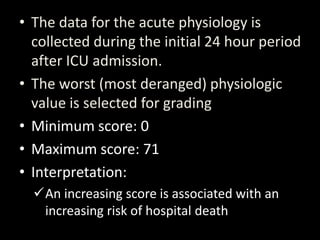
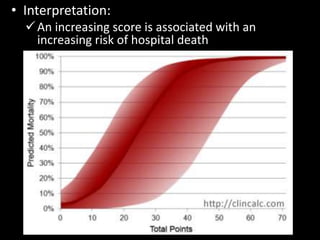
The document discusses various trauma scoring systems used to classify and predict outcomes in trauma patients. It describes physiological scores like the Glasgow Coma Scale (GCS) and Revised Trauma Score (RTS) that assess consciousness and vital signs. Anatomical scores like the Abbreviated Injury Scale (AIS) and Injury Severity Score (ISS) evaluate specific injuries. Combined scores like the Trauma Score-Injury Severity Score (TRISS) and Acute Physiology and Chronic Health Evaluation (APACHE) integrate multiple factors. Each score has benefits for triage, prognosis, and research but also limitations in certain clinical scenarios.