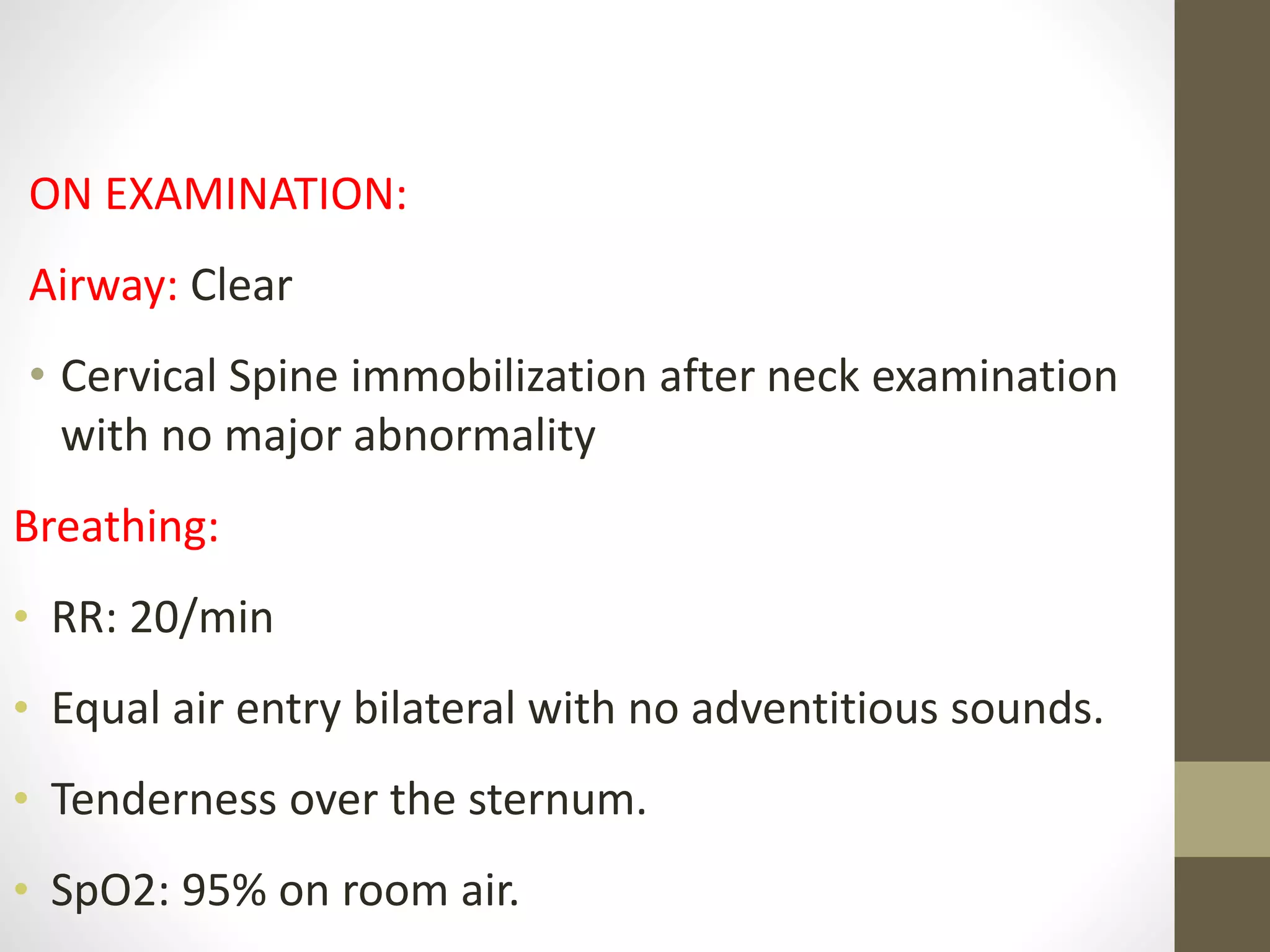
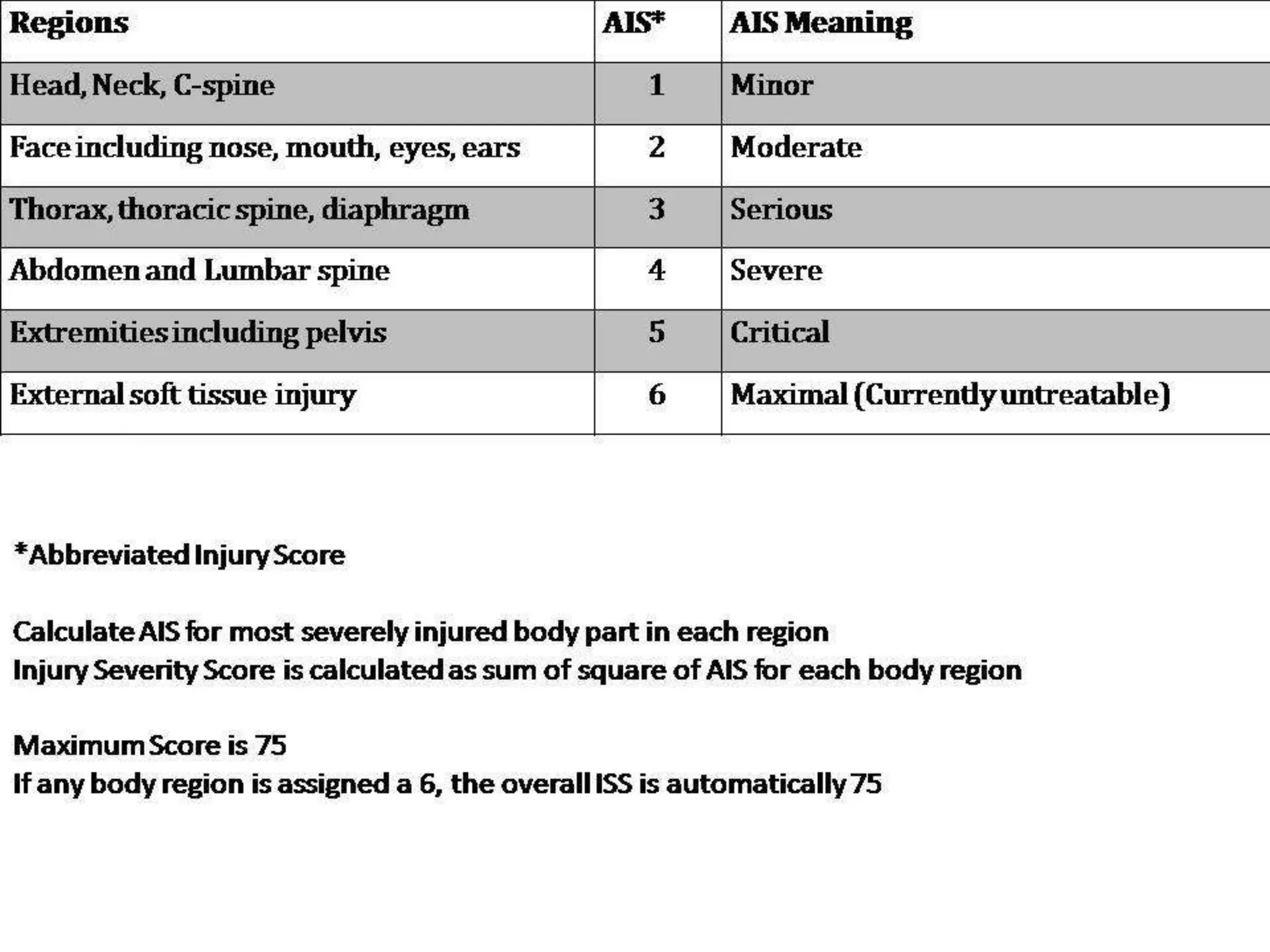
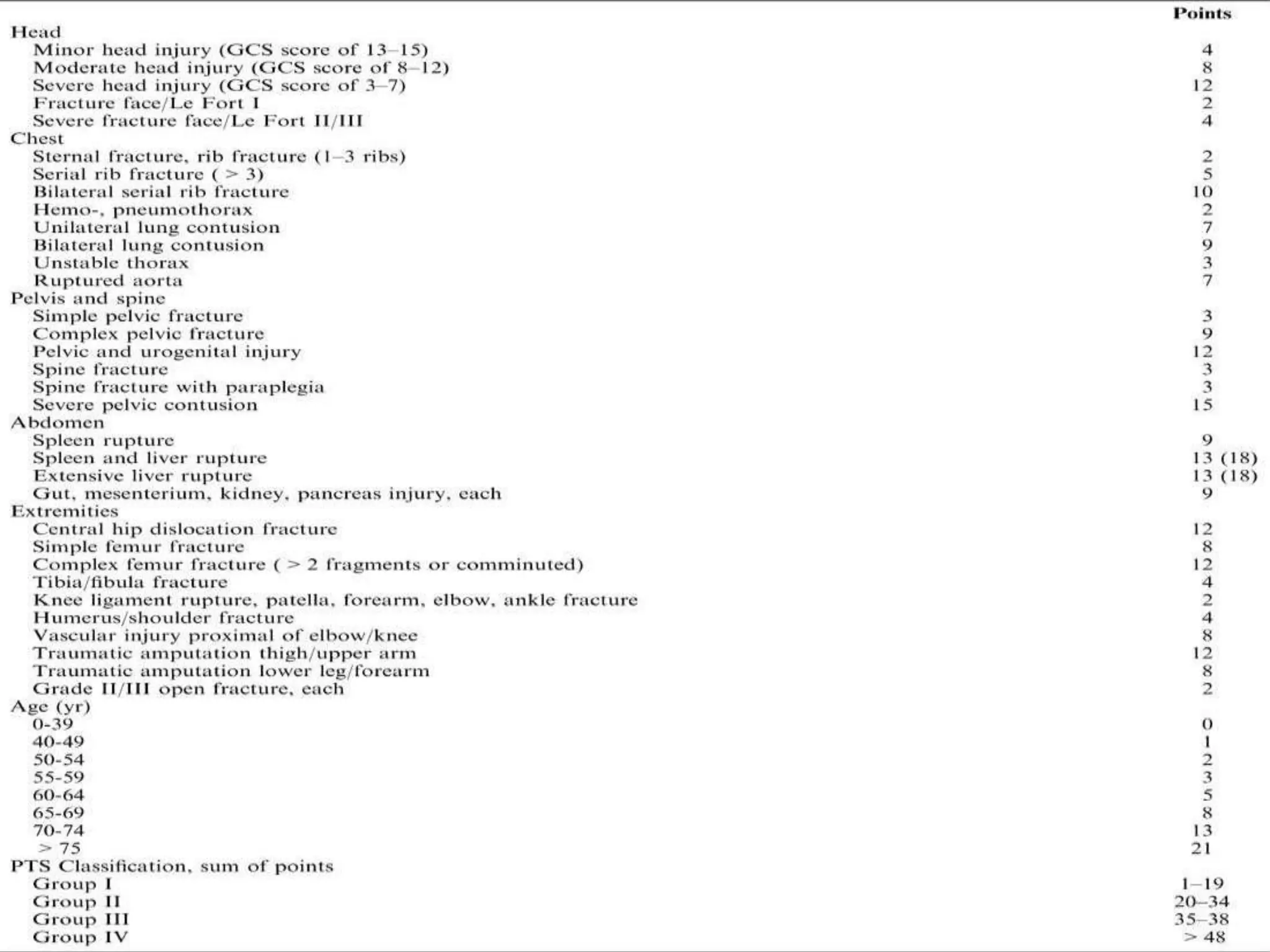
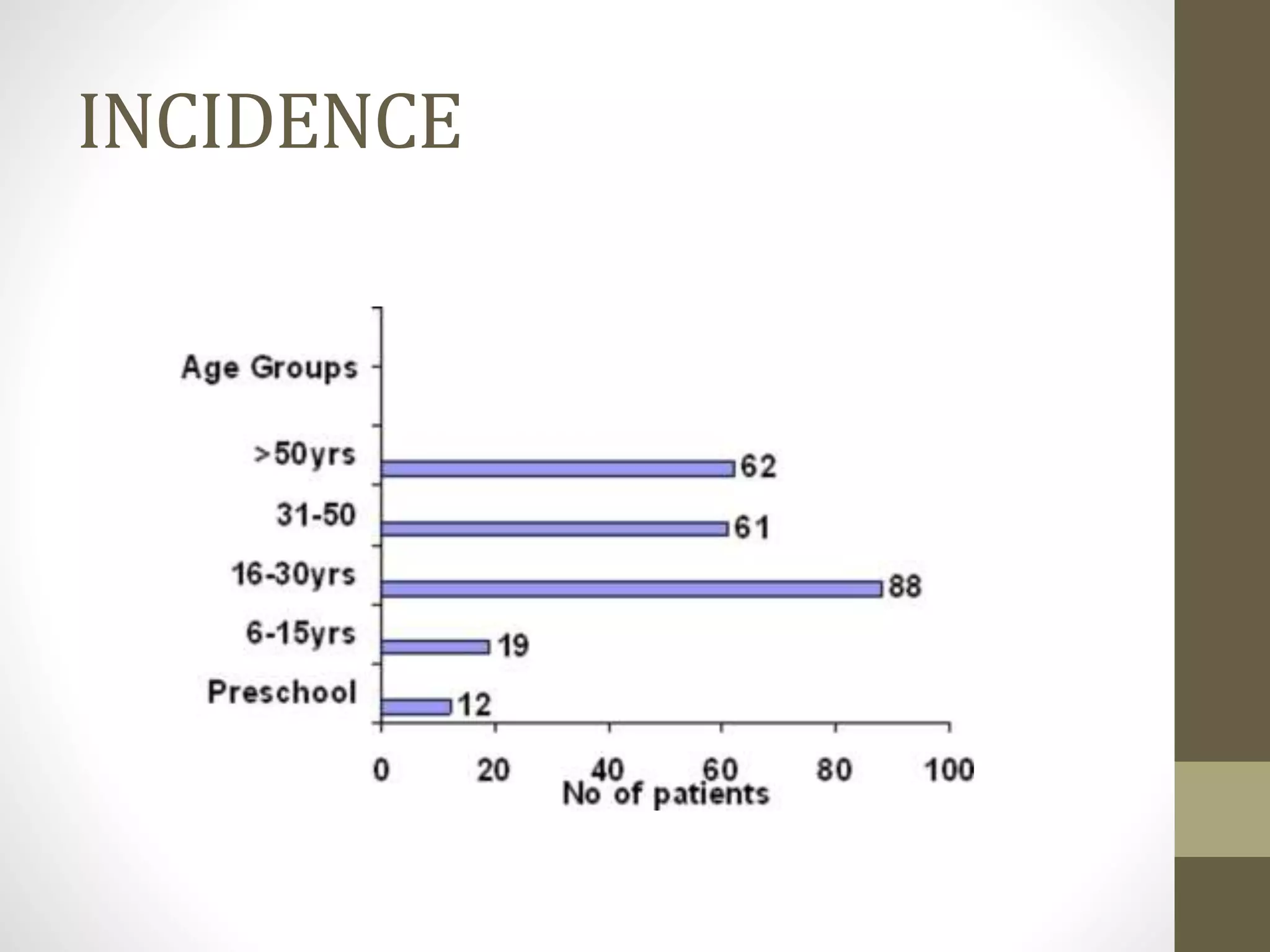
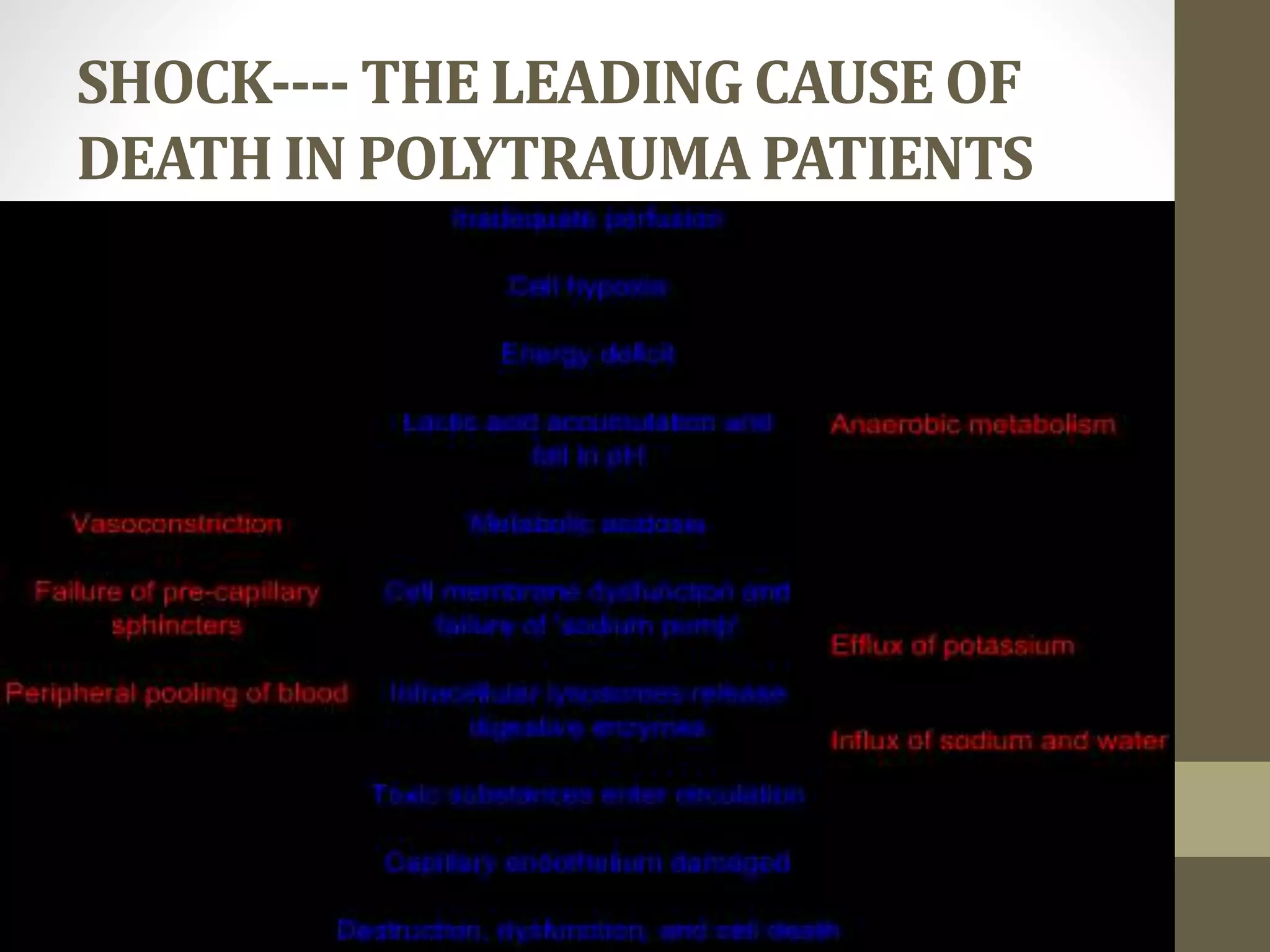
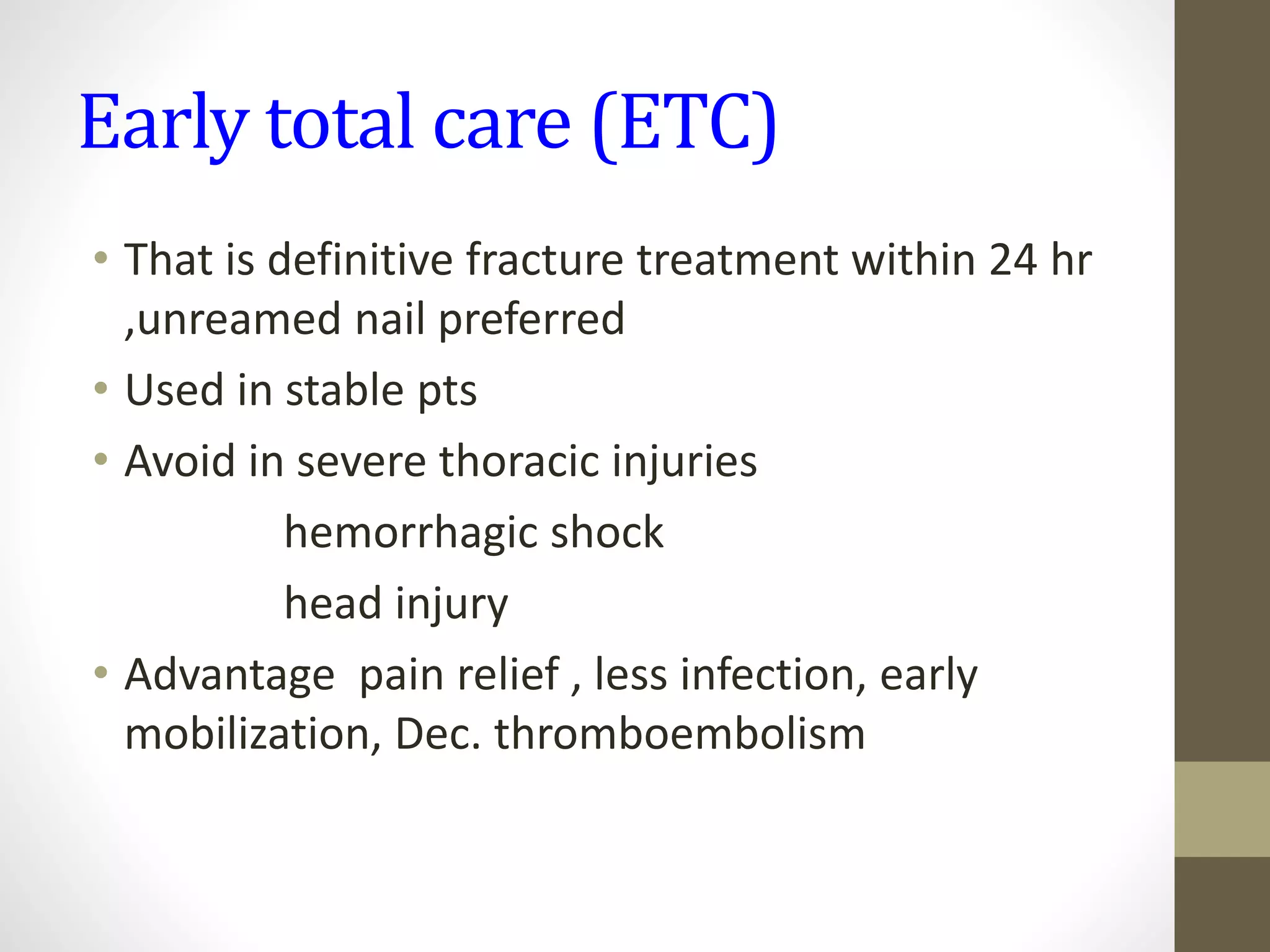
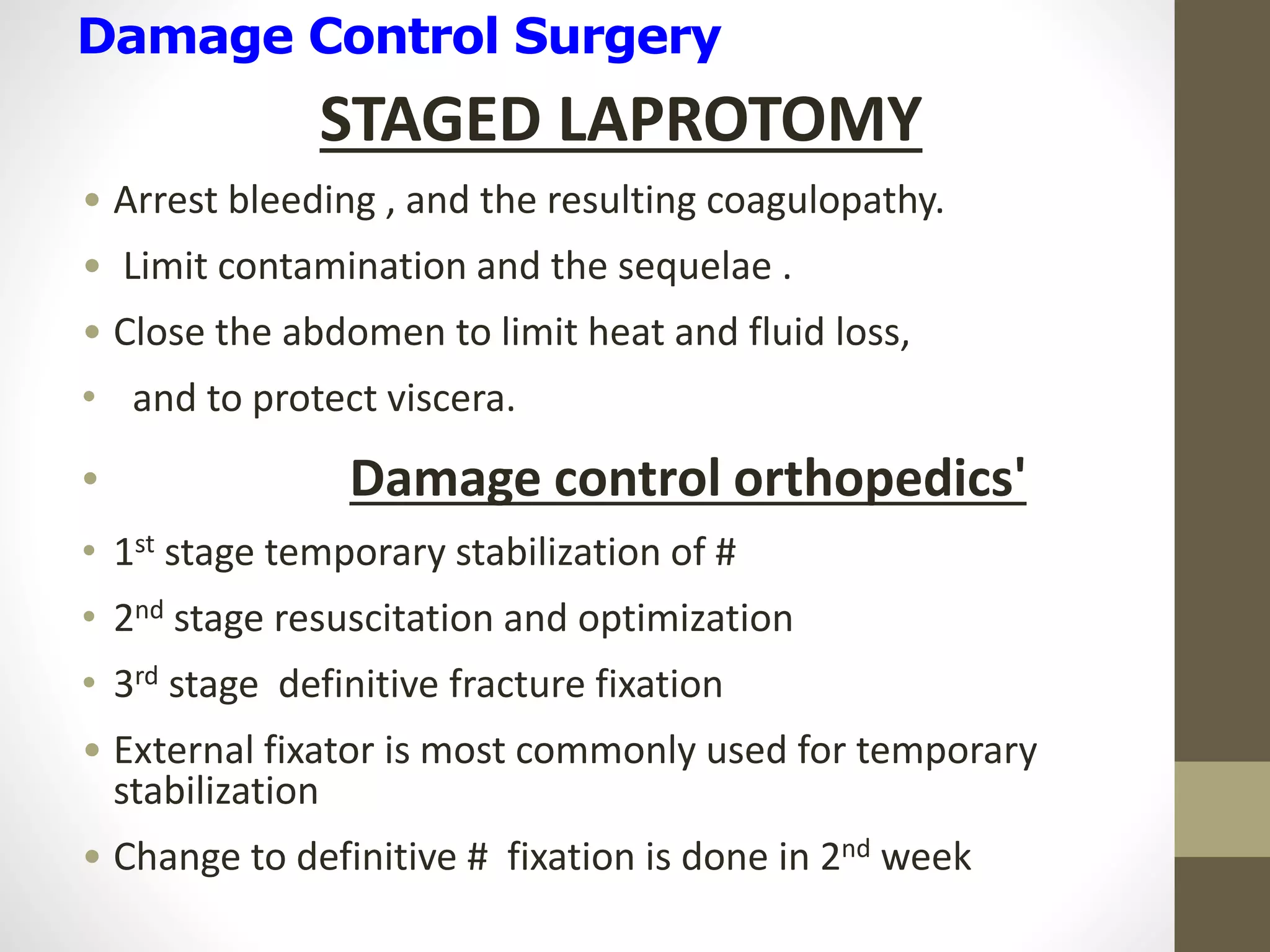
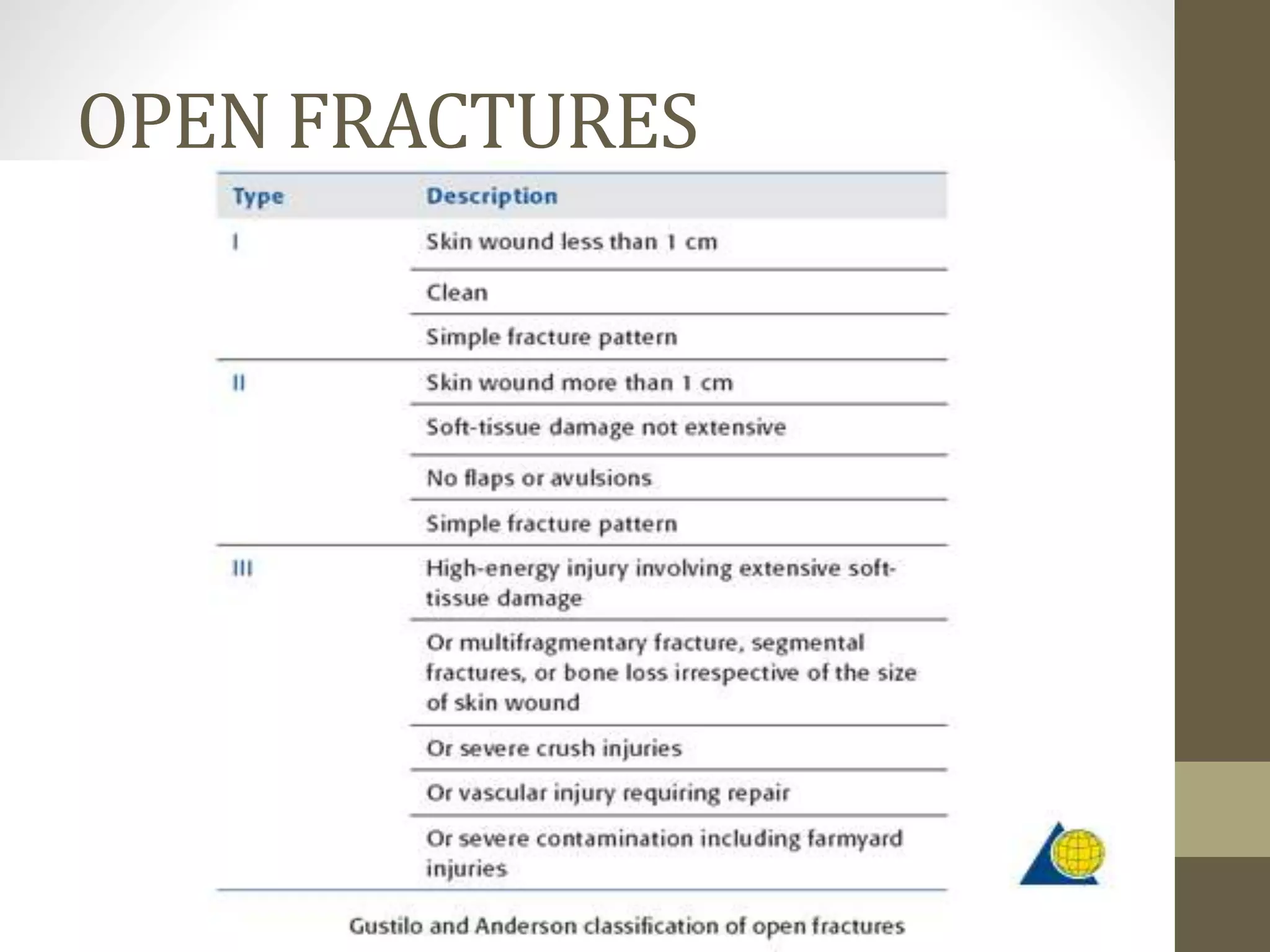
A 28-year-old male presented to the emergency room following a motor vehicle accident complaining of chest pain, a forehead laceration, right forearm pain, and multiple fractures. On examination, he had a Glasgow Coma Scale of 15/15 with stable vital signs. Imaging revealed multiple fractures and injuries consistent with polytrauma. Polytrauma, or multiple trauma, involves serious injuries to multiple body systems such as fractures and internal injuries from high-impact crashes. Proper management requires a team approach and stabilization of life-threatening injuries during the critical golden hour period.